Clinical Images: Progressive Spondylosis
G. Michael Lemole, Jr., MD
Nicholas Theodore, MD
Volker K. H. Sonntag, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Key Words: progressive spondylosis, cervical degeneration
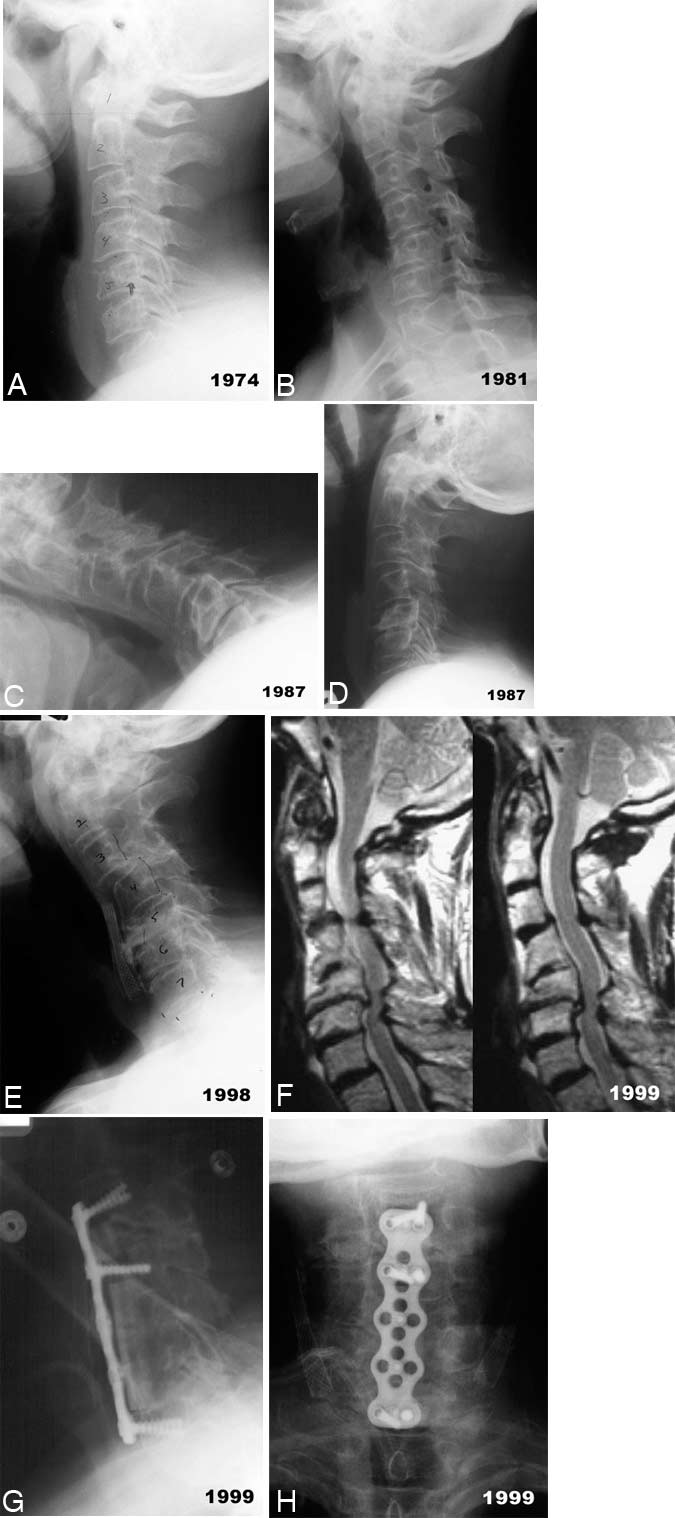
A 71-year-old male complained of persistent neck pain. While playing football in high school, he had sustained nonspecific neck injuries and had again injured his neck in a skiing accident 25 years before seeking treatment at our institution. At that time, a radiograph of the cervical spine revealed an old wedge fracture of the lateral body of C7, a chip fracture of the lateral body of C5, and loss of cervical lordosis between C5 and C7 (Panel A).
Seven years later, a radiograph showed retrolisthesis of C5 relative to C4 and slight anterior wedging of C5 (Panel B). The disk spaces at C4-C5 and C5-C6 were narrowed, and significant osteophytic formations were present.
Six years later, radiographs showed that the retrolisthesis at C5 had increased about 5 mm relative to the vertebral bodies of C4 and C6 with cervical flexion (Panel C). Progressive spondylotic changes, including a slight anterolisthesis of C3 on C4, were present throughout the entire cervical spine. Extension was limited on a flexion-extension view (Panel D).
More than a decade later, a radiograph demonstrated increased anterior wedging of C5 and retrolisthesis relative to C4 and C6 (Panel E). The anterolisthesis of C3 on C4 had also worsened. Diffuse degenerative changes were present throughout the entire cervical spine, including the C1-C2 junction.
At his most recent examination, a slight degree of torticollis was present when the patient bent and rotated his neck to the left. Other than a subtle bilateral weakness of the deltoid muscles, his strength was within normal limits as was his sensory examination.
Deep tendon reflexes were unremarkable except knee jerk reflexes, which were asymmetric and brisk.
Magnetic resonance imaging of the cervical spine (Panel F) confirmed the patient’s cervical misalignment. Disk and osteophytic protrusions, particularly at C4-C5 and C5-C6, significantly narrowed the cervical spinal canal. The spinal canal was also narrowed at C3-C4.
Posterior degenerative changes were noted, but the signal intensity of the spinal cord was normal. Flexion-extension radiographs showed marked instability from C3 to C6.
Because of the patient’s severe cervical spondylosis, progressive multilevel instability, and evidence of early myelopathy, surgical decompression with fusion and stabilization was recommended. The patient underwent anterior cervical corpectomies at C5 and C6 with an anterior cervical diskectomy at C3-C4. Fibular allograft bone was used to reconstruct the spinal column, and an anterior cervical plate was placed from C3 to C7. The patient’s postoperative course was uneventful (Panels G and H).
These images demonstrate the gradual, progressive, and often insidious nature of cervical degenerative disease, which may be related to minor, past traumas. Furthermore, as the load-bearing dynamics of the cervical spine are altered by progressive deformity, degenerative changes at one level can influence similar disease at adjacent levels.