
Role of Image Guidance in the Diagnosis and Treatment of Neck and Back Pain
Alan Pitt, MD
Erin Prenger, DO
Juan Bartolomei, MD†
Division of Neuroradiology
† Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Abstract
Nerve root irritation, facet disease, and disk disease all contribute to back pain. In some cases imaging and physical findings do not identify a clear origin for back pain. Imaging-guided spinal injections offer an additional diagnostic and therapeutic tool. By selectively injecting various parts of the spine, a more specific diagnosis can be made. In certain patients, the injection also may offer a therapeutic benefit, delaying or preventing more invasive options. This article describes the various types of spinal injections and their role in the treatment of back pain.
Key Words: back pain, diskography, imaging, spinal injections, vertebroplasty
Spine-related pain is a common cause of morbidity in our society. As many as 80% of adults are afflicted with back pain during their life. Along with the substantial medical costs, there is an associated burden of lost productivity on society. Unfortunately, the etiology of back pain is often elusive. The common misconception ascribes the majority of cases to “disk herniation,” but this cause is relatively rare. Spinal stenosis, nerve root impingement, facet disease, and annular disease are all considered to be major contributors. Often these pathologies coexist, making it difficult for physicians to decide on appropriate management.
Spinal injection procedures have been used for many years. In the past, many of these procedures were performed in a relatively blinded fashion. Anatomic landmarks were palpated, and trigger point injections were completed either with anesthetic or anesthetic mixed with steroid preparations. More recently, however, there has been a shifted to image-guided procedures, which allow selective placement of medication further aiding in diagnosis and treatment. This article describes the rationale for spinal injections (Table 1), some of the commonly performed procedures, and their role in the clinical management of back pain.
Mechanisms of Back Pain
The understanding of the origin of back pain has lagged behind advances in imaging. In the early part of the 20th century, many investigators considered the posterior elements a primary source of pain. This hypothesis was discarded in the 1930s in favor of the discogenic theory, which attributed pain to herniations of the nucleus pulposus. Direct compression of the nerves and thecal sac was considered the etiology for most pain. With the advent of magnetic resonance (MR) imaging, it is now clear that the causes of pain are multifactorial. Many patients with large disk extrusions are asymptomatic while others with no definable abnormality are in pain.10
Back pain and sciatica most likely reflect a combination of mechanical and inflammatory alterations.12 As the disk degenerates, the intravertebral height diminishes. The taut annular curtain becomes loose and permits increased degrees of rotatory and translational motion. The increased mobility stresses facet joints and ligamentous structures (Fig. 1). Ultimately, degenerative changes lead to hypertrophy of the ligaments and osseous structures, further compromising the spinal canal and foramen. However, the relative lack of correlation between pain and structural changes can likely be explained by the associated chemical response.5
Inflammatory changes are probably modulated by a host of chemical compounds, including phospholipase A2. This compound is a potent inflammatory mediator.18 Although found in normal disks, concentrations of phospholipase A2 increase with degeneration. Annular disruption likely leads to dispersion of the enzyme around the thecal sac and root sleeves inciting a chemical cascade. Notably, inflammatory infiltrates are found in the dorsal root ganglion of patients undergoing diskectomy. Injection of steroids is thought to blunt the inflammatory cascade, essentially disrupting the cycle of pain.1
Patients with back pain often have one or more possible pathologies that contribute to their symptoms. By selective injection of a nerve root, facet, or disk, each component can be isolated, permitting more precise diagnosis and therefore more effective treatment planning. In a significant percentage of cases, an injection provides symptomatic relief, helping patients return to work and physical therapy.
Epidural Steroid Injections
The epidural space extends from the foramen magnum to the sacral hiatus. The space is located between the osseous canal and the dural sac. An interconnected dorsal and ventral nervous plexus is present as well as veins comprising a portion of Batson plexus. A median raphe often separates the space into left and right sides.
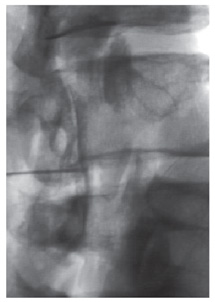
Epidural steroid injections have been performed since the 1930s, but Goebart published the first series in 1961.6 This injection can be performed via an interlaminar or transforaminal approach. The typical patient has multilevel degenerative disk disease or spinal canal stenosis. Risks associated with the procedure include bleeding, infection, headache, thecal puncture, and the possible intrathecal placement of steroids. The latter can cause arachnoiditis. Multiple studies have shown that the needle can be positioned inappropriately when the procedure is performed without image guidance. In 30 to 52% of the cases, the needle misses the epidural space or is placed in the venous plexus (Fig. 1).17,19 Using fluoroscopy Johnson et al.13 performed more than 5000 epidural steroid injections with a complication rate of only 0.07%, all of which were minor and self-limited. Using image guidance, they confirmed needle placement and the distribution of medication within the epidural space.
The efficacy of epidural steroid injection is debated in the literature. However, most examinations are performed without image guidance biasing the data. We believe proper needle placement with imaging for documentation is critical. Using imaging, Yates compared the response of injections of anesthetic to injections of anesthetic combined with steroids and found better outcomes in the latter group.20 In a double-blind study, Dilke and coworkers3 compared steroids to placebo injections and found a significant improvement in the treatment group. Their symptomatology improved and they returned to work more quickly than the placebo group.
Because the use of image guidance is limited, much of this literature is unlikely to reflect the actual efficacy of epidural steroid injections. We recommend using epidural steroid injections in appropriate patients. If they fail to improve after a single injection, a trial of three injections (current practice) is probably not indicated.
Selective Nerve Root Blocks
Selective nerve root blocks are used both to diagnose and to treat patients with back pain. Using image guidance, a small volume of anesthetic and steroid is applied directly to a specific nerve root. If pain is relieved, the procedure identifies the origin of the pain to be the nerve or one of the structures that it innervates. Dooley and coworkers4 reported that the accuracy of the procedure for identifying single nerve roots as radicular pain generators was 85%. This ability can be particularly important when patterns of pain are complex. Imaging studies may identify multiple levels that could contribute to symptomatology. Often nerve roots do not follow an expected dermatomal distribution or there is somatotopic misrepresentation.11 Temporary numbness would be expected from the selective injection of separate nerve roots with an anesthetic agent. The numbness lasts only a few hours but provides useful clinical information. Studies have correlated patients’ response to injection and their ultimate surgical outcome.4,14 Steroids are also administered in the hope of providing patients some degree of long-term benefit.
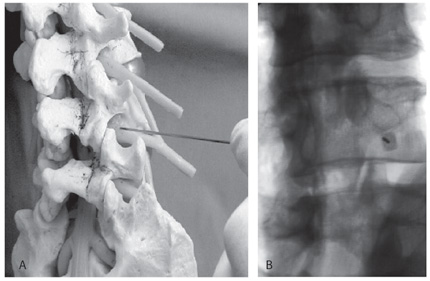
Additional candidates for selective nerve root blocks include patients with far-lateral disk herniations, foraminal stenosis, and postoperative patients. Surgical options are limited for these groups, and selective nerve root blocks can be tried as a primary treatment option. Although this procedure can be performed under computed tomographic (CT) guidance, we prefer to use fluoroscopy in the cervical and lumbar regions (Fig. 2). The procedure requires 10 to 15 minutes and can be associated with complications. At least two known deaths have been associated with cervical nerve root blocks, both performed without confirmation of the location of the needle by injection of contrast. The vertebral artery as well as radicular arteries and veins lie close to the nerve root; consequently, a small amount of contrast is always injected to confirm the location of the needle before medication is injected. If the patient improves after an injection, a series of three injections, typically separated by 10 to 14 days, can be performed. After 6 months, the series is repeated.
Facet Injections
Degenerative facet disease is extremely common. More than two-thirds of people older than 60 years exhibit some degree of degenerative change. Although controversial, the notion that pain originates from the facet joints was introduced at the turn of the century. In 1933 Ghormley coined the term “facet joint syndrome.” He injected facet joints with hypertonic saline and elicited pain that was relieved by anesthetic injection.7
Typical patients with lumbar facet disease experience pain in the hip that radiates to the knee but not to the foot. Pain is often made worse with extension or sudden rotatory movement. Pain also may be elicited by palpating the joint. Imaging studies demonstrate degenerative facets with hypertrophy. Occasionally, an associated synovial cyst is identified compressing the adjacent nerve root.
In the cervical spine, facet disease is thought to cause cervical headaches (related to the third cervical nerve) and intrascapular dorsal pain.7,16 In both syndromes, the pain is relatively unilateral and may or may not be associated with neck pain. The medial nerve, a small sensory branch of the dorsal nerve root, innervates the facet joint. Typically, the medial nerve extends from the nerve root at the level of the facet with an additional supply from the level above. This supply is responsible for the referred symptomatology often associated with facet disease.
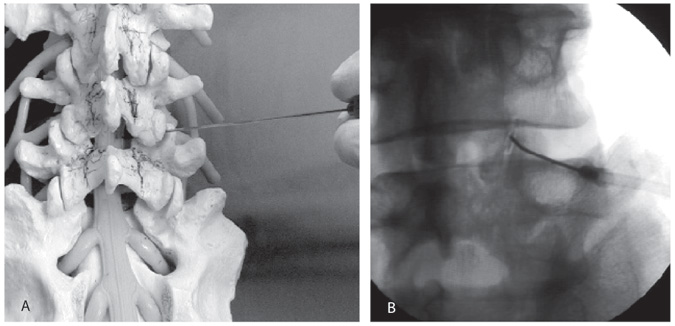
Image-guided procedures can be directed at the joint or medial nerve. If the joint is injected directly, we prefer to enter its inferior recess (Fig. 3). A small amount of contrast is injected followed by about 1 ml of anesthetic and steroid. Degenerative changes and anatomic considerations often make more lateral approaches unsuccessful. Occasionally, the joint cannot be investigated directly because the degenerative hypertrophy is too advanced. In such cases, a periarticular injection at the medial nerve can be performed at the level of concern and one level above.
Although some workers have questioned the value of facet injections, most studies indicate that they offer a short-term benefit. Long-term results are less encouraging. 8,15 We believe that the benefit of facet injections is primarily diagnostic; a positive injection identifies the source of pain and excludes other etiologies. This information can prevent unnecessary surgical interventions. In well-selected patients, rhizotomy of the medial nerve, which is particularly effective in the cervical region, can be performed
Diskography
In 1941 Lindgren first reported diskography to the Swedish Radiologic Society. Since then the procedure has gone through various phases of acceptance—from widespread to almost not at all. Many radiologists trained in the 1980s and 1990s have never performed the procedure. Recently, however, there has been a resurgence of interest in diskography. Unlike the other injection procedures, diskography is performed strictly for diagnostic purposes. It offers no intrinsic therapeutic benefit.
Diskography is a provocative test. Contrast injected into the disk stresses the surrounding annular fibers. The patient’s response to this injection is recorded and used to plan treatment. Typically, diskography is performed on patients with multilevel degenerative disk disease in the hope of identifying an appropriate level or levels for fusion. Evidence correlates patients’ response to diskography with surgical outcome. Colhoun et al.2 reported that 89% of their patients experienced significant relief after fusion when diskography demonstrated internal derangement and elicited a positive pain response. In contrast, only 52% of their patients with disk derangements alone responded to surgery.
This procedure is not without complications. Infection, the primary concern, is estimated at 0.15% per disk injected.9 The rate of infection decreases slightly when the procedure is performed with a coaxial system. We routinely administer antibiotics intravenously before the procedure. Although many practitioners continue to perform cervical diskography, we do not offer this service because of the risk of infection.
Vertebroplasty
Vertebroplasty is a relatively new procedure used to treat pain related to spinal compression fractures. Most of these fractures cause self-limited pain, but it is sometimes so severe that patients are essentially immobilized. No good surgical option is available. External bracing and narcotics are seldom effective. Typically, the fractures are benign and related to underlying osteoporosis, but the procedure also can be used to treat aggressive hemangiomatosis and metastatic disease to the spine.
Patient selection is critical. Central back pain should be focal; few or no radicular symptoms should be present. The vertebral body should be compressed less than 70%, and retropulsion into the spinal canal should be less than 20%. An MR image or (less optimally) a bone scan and CT are obtained to document active edema of the bone marrow.
Vertebroplasty is performed on an outpatient basis under local anesthesia. A needle is inserted into the vertebral body, and polymethylmethacrylate (the bone cement used for artificial joints) is injected. Most often patients are sent home the same day. In 80 to 90% of the cases, pain related to the fracture is significantly reduced or eliminated. The cement maintains some height, thereby preventing further collapse of the vertebral body.
Kyphoplasty is an alternative technique. The methods are similar except that high-pressure balloons are used to create a cavity before the cement is placed. Some height might also be restored, but this claim is not clearly documented.
Conclusions
Image-guided spine interventions offer an opportunity to assist in the management of back pain. By offering a thorough assessment of the various possible causes of pain, treatment planning can be tailored to patients’ pathophysiology. These procedures also offer the opportunity to manage patients with a minimally invasive procedure.
References
- Benzon HT: Epidural steroid injections for low back pain and lumbosacral radiculopathy. Pain 24:277-295, 1986
- Colhoun E, McCall IW, Williams L, et al: Provocation discography as a guide to planning operations on the spine. J Bone Joint Surg Br 70:267-271, 1988
- Dilke TF, Burry HC, Grahame R: Extradural corticosteroid injection in management of lumbar nerve root compression. Br Med J 2:635-637, 1973
- Dooley JF, McBroom RJ, Taguchi T, et al: Nerve root infiltration in the diagnosis of radicular pain. Spine 13:79-83, 1988
- Dussault RG, Kaplan PA, Anderson MW, et al: Interventional musculoskeletal radiology of the spine, in Taveras JM, Ferrucci JT (eds), Radiology. Philadelphia: Lippincott-Raven, 1998, pp 1-21
- Evans W: Intrasacral epidural injection in treatment of sciatica. Lancet 2:1225-1229, 1930
- Ghormley RK: Low back pain with special reference to articular facets with presentation of an operative procedure. JAMA 101:1773, 1933
- Carette S, Marcoux S, Truchon R, et al: A controlled trial of corticosteroid injection into facet joints for chronic low back pain. N Engl J Med 325:1002, 1991.
- Guyer RD, Ohnmeiss DD: Lumbar discography. Position statement from the North American Spine Society Diagnostic and Therapeutic Committee. Spine 20:2048-2059, 1995
- Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al: Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 331:69-73, 1994
- Jinkins JR, Whittemore AR, Bradley WG: The anatomic basis of vertebrogenic pain and the autonomic syndrome associated with lumbar disk extrusion. AJR Am J Roentgenol 152:1277-1289, 1989
- Johnson BA: Image-guided epidural injections. Neuroimaging Clin N Am 10:479-491, 2000 1
- Johnson BA, Schellas KP, Pollei SR: Epidurography and therapeutic epidural injections: Technical considerations and experience with 5334 cases. AJNR Am J Neuroradiol 20:697-705, 1999
- Kinard RE: Diagnostic spinal injection procedures. Neurosurg Clin N Am 7:151-165, 1996
- Murtagh FR: Computed tomography and fluoroscopy guided anesthesia and steroid injection in facet syndrome. Spine 13:686-689, 1988
- Poletti CE: Third cervical nerve root and ganglion compression: Clinical syndrome, surgical anatomy, and pathological findings. Neurosurgery 39:941-948, 1996
- Renfrew DL, Moore TE, Kathol MH, et al: Correct placement of epidural steroid injections: Fluoroscopic guidance and contrast administration. AJNR Am J Neuroradiol 12:1003-1007, 1991
- Saal JS, Franson RC, Dobrow R, et al: High levels of inflammatory phospholipase A2 activity in lumbar disc herniations. Spine 15:675-678, 1990
- White AH, Derby R, Wynne G: Epidural injections for the diagnosis and treatment of low-back pain. Spine 5:78-86, 1980
- Yates DW: A comparison of the types of epidural injection commonly used in the treatment of low back pain and sciatica. Rheumatol Rehabil 17:181-186, 1978

