Meningioma
Meningioma Overview
A meningioma is a type of brain tumor or spine tumor that starts in the meninges, or the protective coverings of your brain and spinal cord.
Your meninges consist of three layers of tissue that fill the space between your brain and skull and the space between your spinal cord and spine: the dura mater, the arachnoid mater, and the pia mater. When a meningioma forms, it emerges from the arachnoid cells in the arachnoid layer.
- The arachnoid mater lies between the outer layer (dura mater) and the inner layer (pia mater). It has a delicate, web-like structure that helps cushion the brain and spinal cord by holding cerebrospinal fluid, which provides additional protection and nourishment. This layer plays an important role in protecting the nervous system from injury.
- The dura mater is the thick, outermost protective layer that covers your brain and spinal cord, acting like a shield to keep these vital areas safe. It’s the outermost of the meninges.
- The pia mater is a thin, delicate layer of tissue that covers the surface of the brain and spinal cord. It is the innermost meningeal layer. It provides essential support by containing blood vessels that nourish the brain and spinal cord, helping to protect these vital structures from injury. Although soft and almost invisible to the naked eye, the pia mater plays a critical role in keeping the brain healthy and functioning properly.
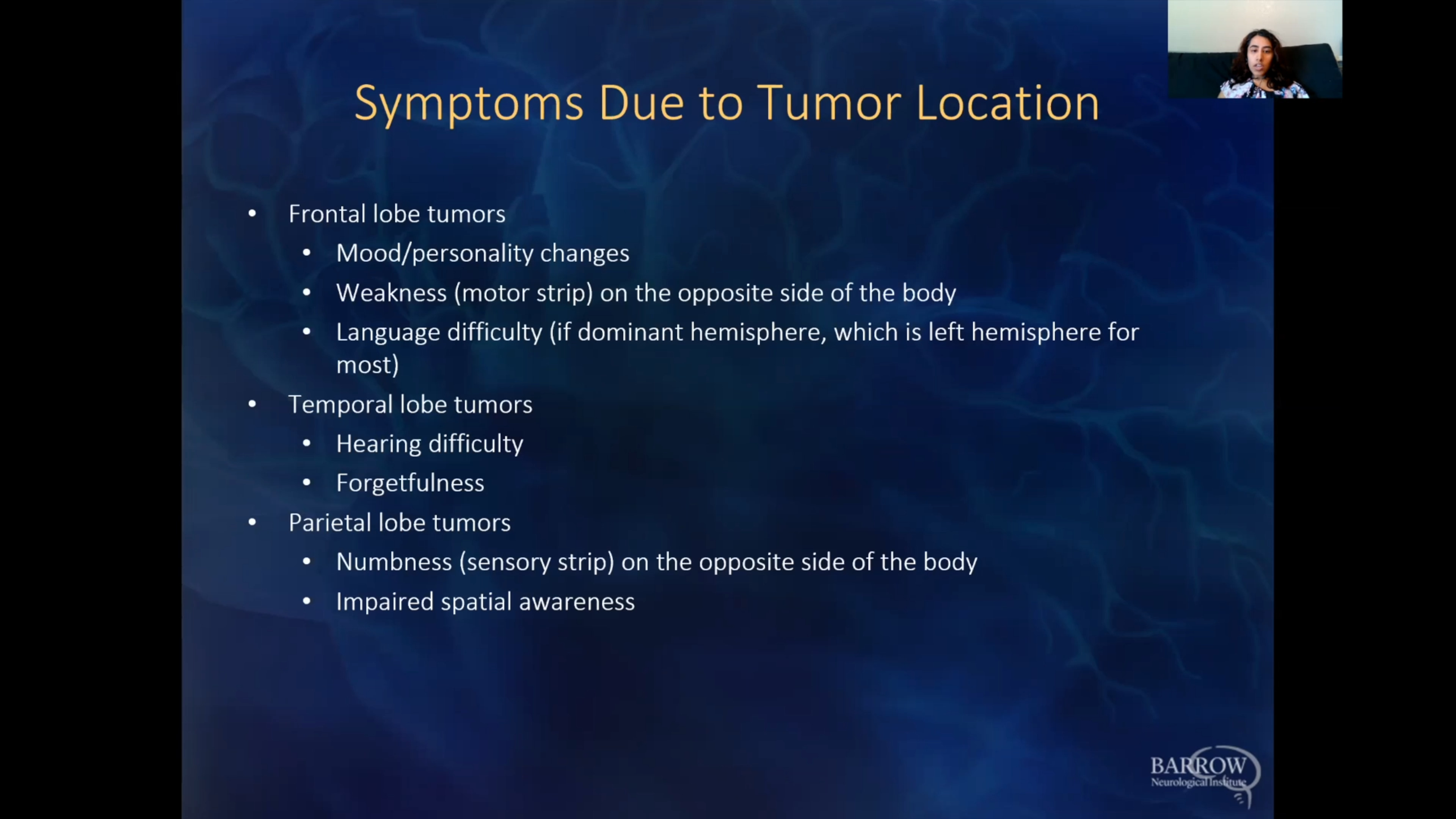
Symptoms are dependent on where the meningioma is and how big it gets. They can range from headaches and blurred vision to problems with memory or seizures.
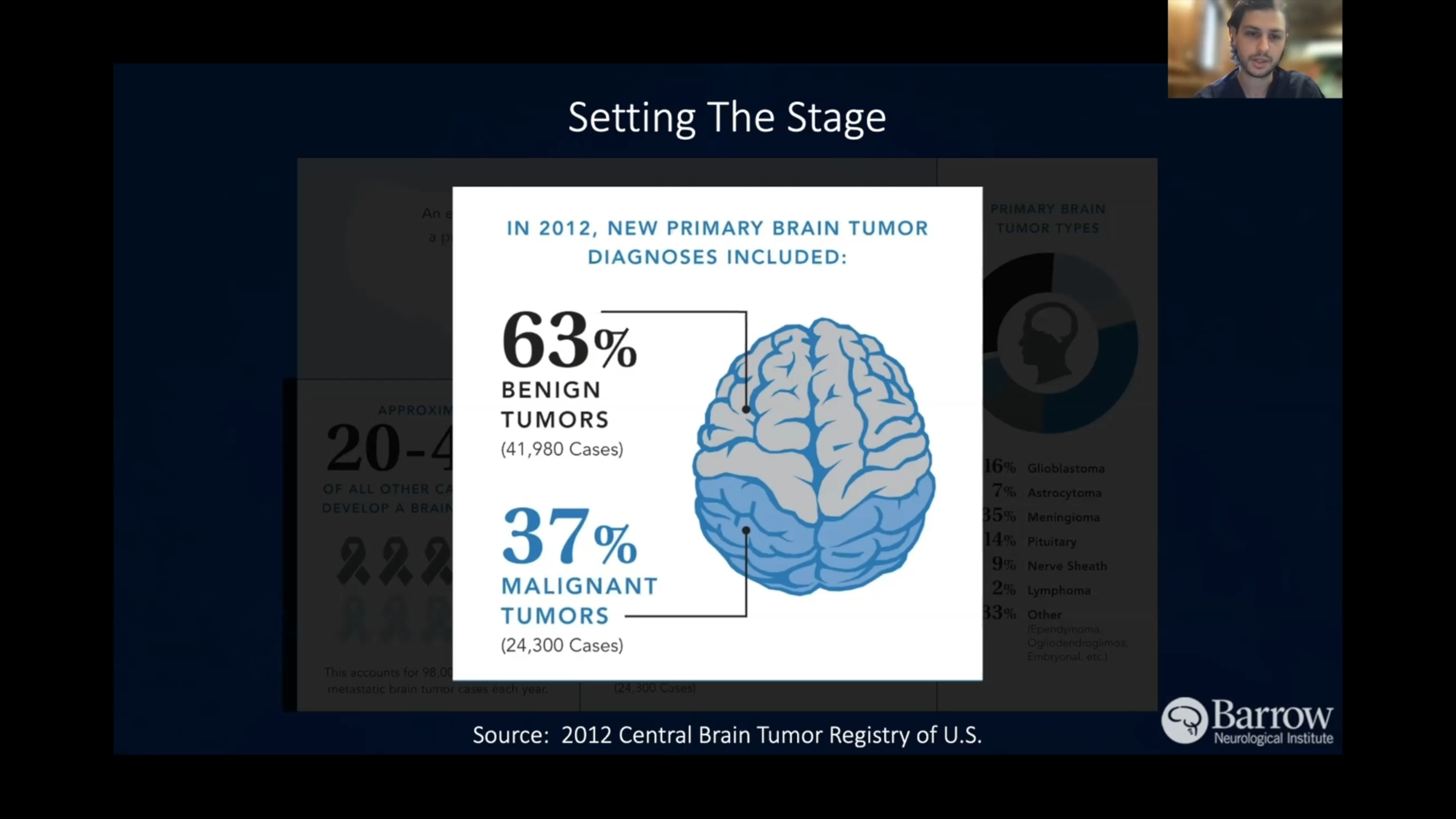
Meningiomas are the most common intracranial tumors, meaning they’re the most frequent tumors found in the spaces protected by the bones that form the head or skull. Most meningiomas are benign or noncancerous—they don’t invade nearby tissue or migrate (metastasize) to other parts of your body—and they’re slow-growing. This is both good news and not-so-good news: a meningioma’s slow growth can take years to cause symptoms, but at the same time, it makes it more challenging to catch in the earlier stages.
What causes meningioma?
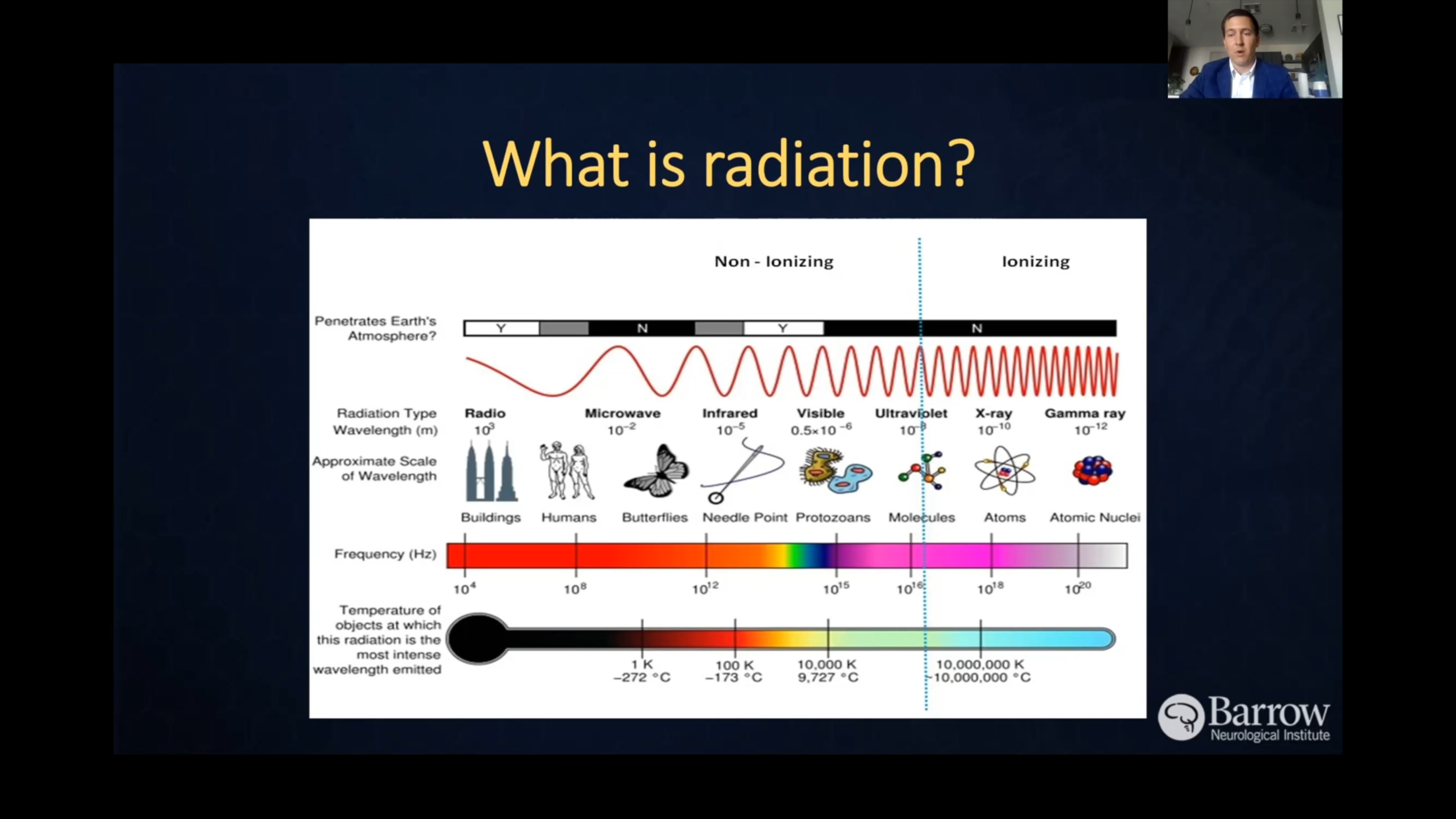
The exact cause of meningiomas is not fully understood. We do know that, overall, cancer is a genetic disease caused by changes to genes that control the way our cells function. Exposure to radiation, especially in childhood, is the only identified environmental risk factor for developing meningioma. Additionally, those diagnosed with genetic conditions called schwannomatosis and neurofibromatosis type 2 are at an increased risk of developing malignant or multiple meningiomas.

Meningioma Symptoms
Because meningiomas are known to be slow-growing, they only sometimes cause symptoms once they have grown into a large tumor. At the same time, some meningiomas can remain asymptomatic for a lifetime or are only detected when a patient has a brain scan for unrelated symptoms.
Some meningiomas grow in a way that can pressure your brain or your skull. If this is the case, your symptoms will depend on the location of the meningioma.
Symptoms you or a family member with meningioma might notice include:
- Headaches, especially ones that are worse in the morning
- Nausea or vomiting
- Vision changes
- Loss of hearing or smell
- Weakness, difficulty walking, and coordination problems
- Confusion
- Changes in personality or behavior
- Seizures
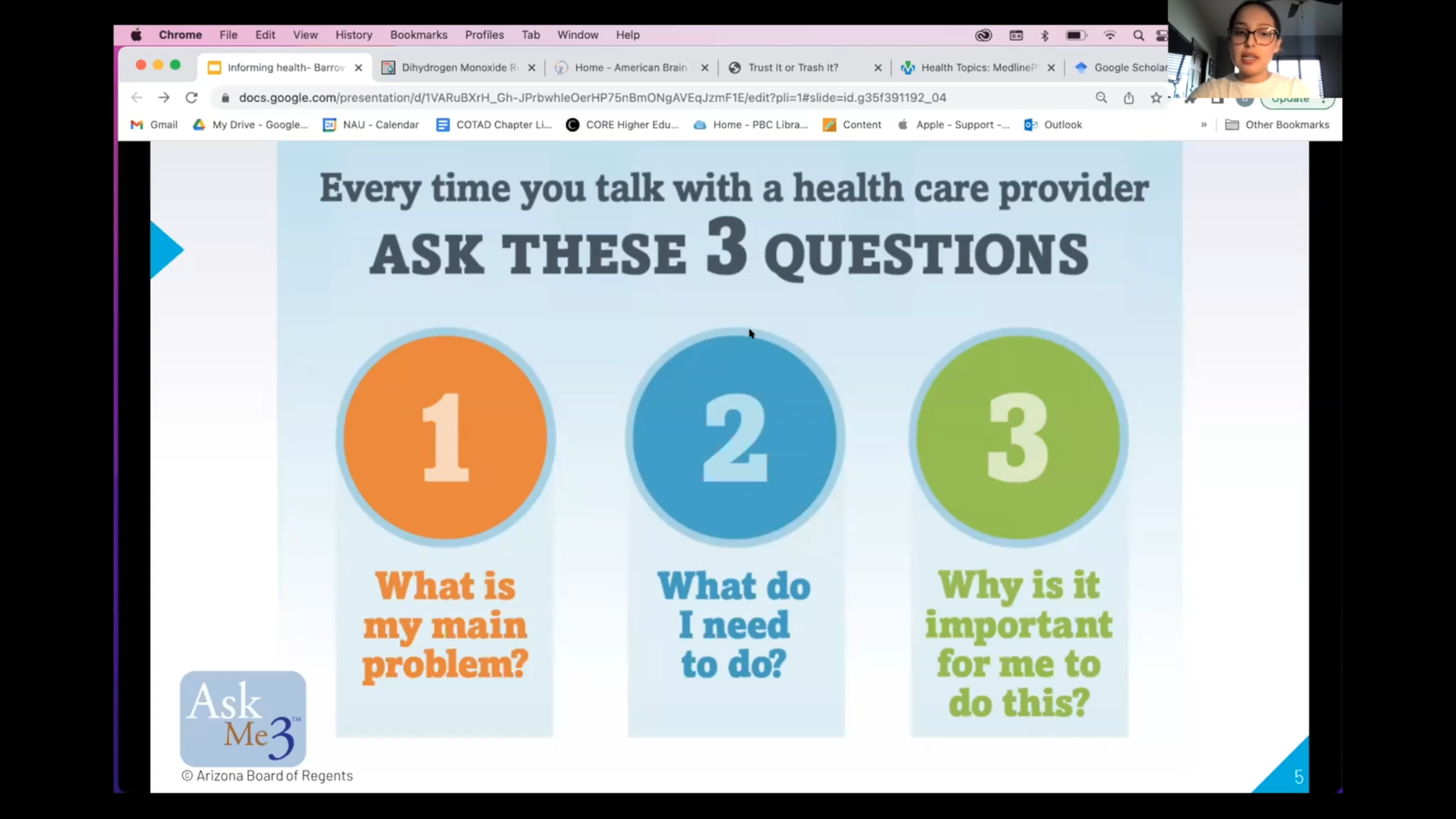
Remember, your doctor can’t diagnose a meningioma based on symptoms alone; a definitive diagnosis requires medical imaging and a biopsy. If you’re concerned about any of these symptoms, it’s always a good idea to seek the help of a healthcare professional.
Meningioma Diagnosis
Because most meningiomas are slow-growing and typically only affect adults, symptoms can be so subtle that people often mistake them for the effects of aging. As a result, misdiagnosis is unfortunately common.
Diagnostic imaging—like magnetic resonance imaging (MRI) or a computed tomography (CT) scan—confirms the presence of meningioma. The only way to get a definitive diagnosis is through a biopsy, when a pathologist studies a small sample taken from the tumor with a needle.
Like most other forms of cancer, meningiomas are grouped into three grades based on their attributes:
- Grade 1: These tumors are the most common and comprise nearly 80 percent of diagnosed meningiomas. They’re low-grade, meaning the tumor cells grow slowly.
- Grade 2: These atypical meningiomas are mid-grade tumors, meaning they have a higher chance of reoccurring after removal and radiation.
- Grade 3: These meningiomas are malignant and fast-growing (anaplastic) and need close monitoring after surgery and radiation.

Meningioma Treatments
There’s no single approach that works universally for every person with a brain tumor—each treatment is unique, just like the patient.
After a meningioma is diagnosed, your healthcare team will want to monitor it to determine if it’s growing or creating further problems. Tumor profiling for gene mutations may also help determine your best course of treatment.
If the meningioma is small and does not cause symptoms, your team may regularly monitor the tumor through diagnostic imaging alone. Conversely, if the meningioma is growing or causing symptoms, your team is likely to recommend surgery or radiation therapy to shrink or remove it. As a rule of thumb, chemotherapy is generally only used as a last-resort meningioma treatment.
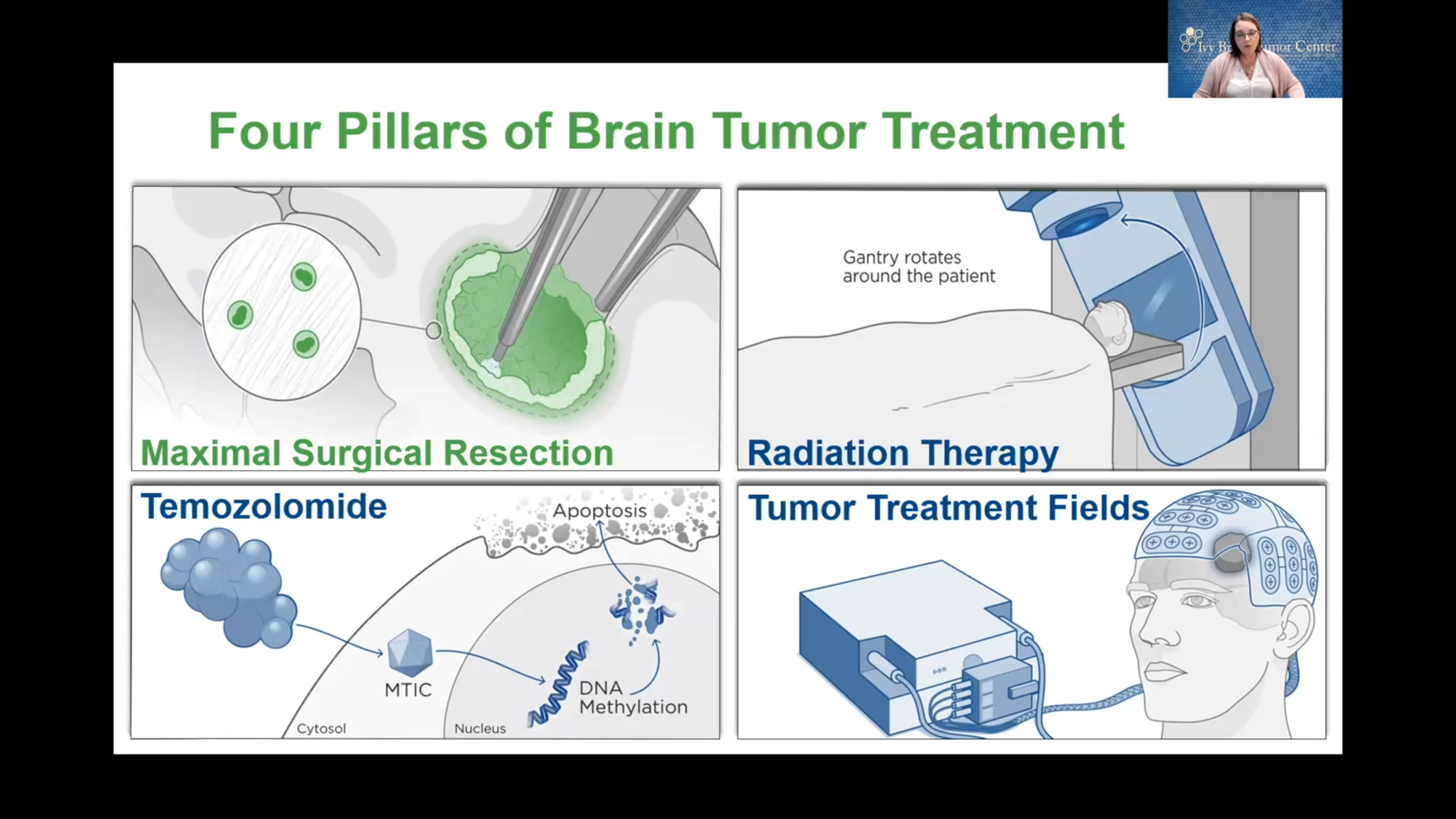
Surgery
At Barrow, our surgeons specialize in two types of precise surgery for meningiomas: microsurgery and endoscopic surgery.
- Microsurgery uses a powerful operating microscope to help your surgeon distinguish between tiny structures in and around your meninges, the three layers of protective coverings in the brain and spinal cord.
- Endoscopic cranial surgery uses small tubes and a tiny camera to help your surgeon remove your tumor in small pieces.
Radiosurgery
Gamma Knife radiosurgery is an advanced form of accurate radiation therapy that achieves results similar to those used in traditional surgical techniques.
The ‘knife’ in this surgery consists of many small beams of radiation focused on a single point. Each beam is too weak to damage healthy tissue, but at the point where the beams converge, they deliver a dose of radiation that’s lethal to the tumor.
Gamma Knife is an outpatient procedure, doesn’t involve incisions, and requires only brief sedation under general anesthetic. This treatment allows people to go home the same day without the pain and risk of complications associated with traditional surgery.
Cyberknife is another form of radiosurgery that delivers focused beams of radiation to tumors without a surgical incision. Its technology uses image-guided robotics to supply surgically precise radiation to destroy a tumor while sparing surrounding healthy tissue.
Cyberknife radiosurgery makes previously unreachable tumors accessible. It’s best suited for tumors otherwise diagnosed as inoperable.
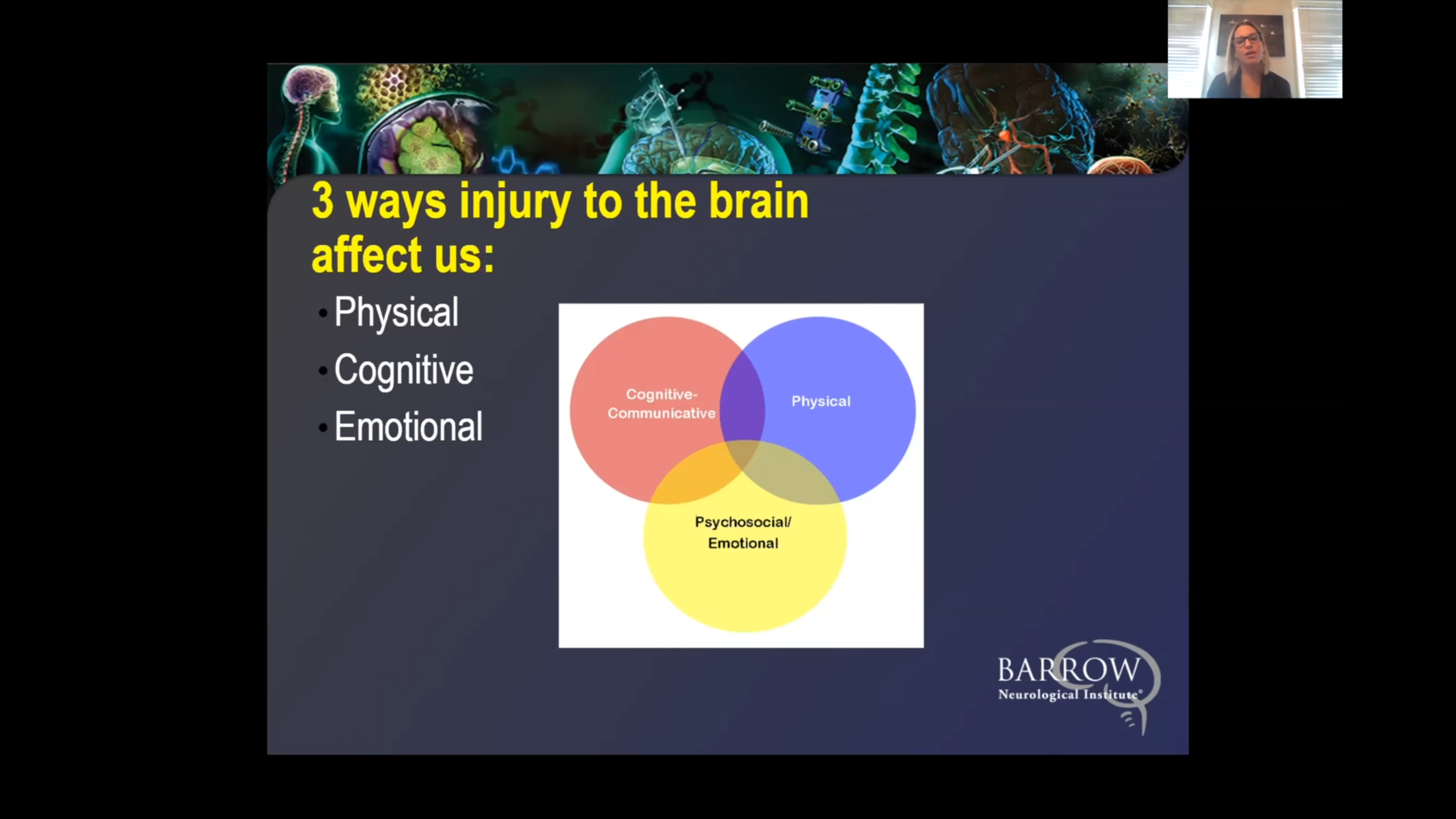
Quality of Life Considerations
When we treat a brain tumor at Barrow, we’re not only focused on extending your life; we’re focused on optimizing your quality of life, too. This is why we provide access to neuro-rehabilitation specialists to help you maximize your independence after a brain tumor like meningioma and return to your life with a renewed sense of self-confidence. The critical thing to remember is that, by and large, meningiomas can be managed, and many people diagnosed with one lead normal lives with treatment.
Common Questions
How common are meningiomas?
It isn’t easy to know how often meningiomas happen, since those who have them are usually without symptoms (asymptomatic). Between one and two percent of autopsies reveal an undetected meningioma.
Thanks to modern medical imaging, the rate at which meningiomas are discovered has tripled, resulting in an occurrence rate of 19 cases per 100,000 individuals, or 0.02 percent.
Who gets meningiomas?
People who have been exposed to excessive amounts of radiation, especially to their scalp, may have an increased risk of developing a meningioma.
Meningiomas are more common in females, but Grades 2 and Grade 3 meningiomas occur more frequently in males. Research has found that obesity is associated with increased risks of meningiomas. The risk of meningioma increases with age—they most often occur in people who are around 60 years old—and in people diagnosed with neurofibromatosis type 2 (NF-2). Children between the ages of 0-14 are at the lowest risk of developing meningioma.
What is the prognosis for those with meningioma?
Many individuals with meningiomas have a good prognosis, especially if the tumor is diagnosed and treated early. That said, the prognosis can vary widely, depending on the meningioma characteristics, a person’s age and overall health, the effectiveness of their treatment, and whether or not the condition reoccurs. Some general information about the prognosis for each grade of meningioma is below.
Grade 1 (Benign Meningioma)
This is the most common and least aggressive form of meningioma, accounting for 80-85% of all cases. The prognosis is generally excellent. Most people can expect long-term survival after surgical removal, with a 5-year survival rate of approximately 80-90%.
Recurrence rates are low (10-20%), especially when complete surgical tumor removal is achieved.
Postoperative treatment is typically not required unless the tumor is incompletely resected or inoperable, in which case your care team may recommend radiation therapy.
Grade2 (Atypical Meningioma)
This type is more aggressive than Grade 1. The 5-year survival rate for a Grade 2meningioma is lower compared to Grade 1, ranging from 60-80%.
Recurrence rates are higher (20-40%) even after complete resection, and these tumors tend to grow faster.
Treatment often includes surgery followed by radiation therapy, especially if your neurosurgeon can’t remove the tumor entirely. Close monitoring with regular MRI scans is necessary due to the higher likelihood of recurrence.
Grade 3 (Anaplastic/Malignant Meningioma)
A grade 3 meningioma is the rarest and most aggressive form of meningioma, with a 5-year survival rate of around 30-50%.
These tumors have a high recurrence rate (50-90%) and tend to spread more rapidly. Even after aggressive treatment with surgery and radiation, recurrence is common, and your care team may suggest additional therapies (like chemotherapy). The malignant nature of these tumors often leads to damage to nearby structures of the brain, which can produce significant symptoms. There’s generally a better outcome if your neurosurgeon can remove the entire tumor. However, depending on the meningioma’s location, this is not always possible.
Can meningioma be prevented?
Since the exact cause of meningiomas has yet to be fully understood, no strategies have been proven to prevent them. Meningiomas have been associated with certain risk factors, meaning a lifestyle change can influence the likelihood of developing a brain tumor in general, as well as a meningioma. These modifications include following a healthy diet, maintaining a healthy weight for your body type, regular and consistent exercise, and limiting radiation exposure.
Additional Resources
American Brain Tumor Association
/
References
- Zhou JJ, Farber SH, de Andrada Pereira B, DiDomenico JD, Williams GP, Almefty KK, Kakarla UK, Uribe JS, Turner JD. Metastasis of Intracranial Meningioma to the Osseous Spine: Systematic Literature Review and Case Report. World Neurosurg. 2024 Mar;183:192-203. doi: 10.1016/j.wneu.2023.11.056. Epub 2023 Nov 22. PMID: 37995989.
- Anand SK, Sardari H, Sadeghsalehi A, Bagheri SR, Eden SV, Lawton MT, Alimohammadi E. Radiopathologic predictors of recurrence in patients with a gross totally resected atypical meningioma. Neurol Res. 2022 May;44(5):468-474. doi: 10.1080/01616412.2021.2022915. Epub 2021 Dec 30. PMID: 34967283.
- Sarris C, Sanai N. Convexity meningioma resection in the modern neurosurgical era. Handb Clin Neurol. 2020;170:87-92. doi: 10.1016/B978-0-12-822198-3.00030-6. PMID: 32586511.