Deep Brain Stimulation (DBS) Surgery
Deep Brain Stimulation (DBS) Surgery Overview
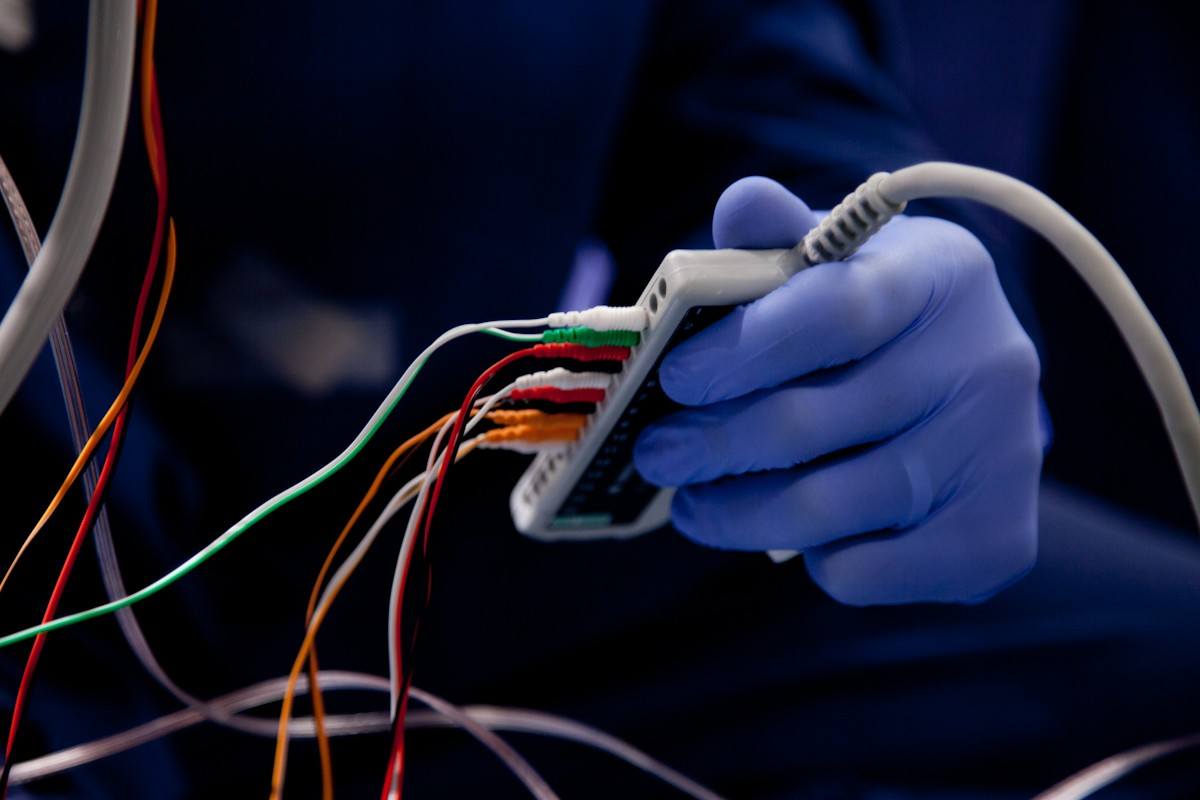
Deep brain stimulation (DBS) is a neurosurgical treatment in which electrodes are implanted in an area of the brain and connected to a pulse generator—a pacemaker-like device placed under the skin, just below the collarbone. This pulse generator is then programmed to deliver electrical pulses into the targeted areas of the brain.
These pulses change the brain’s electrical activity pattern to regulate abnormal signals that are caused by Parkinson’s disease, dystonia, essential tremor, and epilepsy.
The DBS device consists of three distinct parts:
- The electrode or lead: A thin, insulated wire inserted through a small opening made in the skull and implanted in a specific area of the brain, depending on the disorder.
- The extension: This is an insulated wire passed under the skin of the head, neck, and shoulder, connecting the lead to the implanted pulse generator.
- The pulse generator: The “battery pack” of the treatment, the pulse generator is most commonly implanted under the skin beneath the collarbone.


What does Deep Brain Stimulation (DBS) help treat?
Deep brain stimulation aims to improve disease symptoms and medication side effects, although in some cases, treatment addresses one but not both. In movement disorders like Parkinson’s disease, dystonia, or essential tremor, symptoms can include rigidity, tremor, and dystonic movements; involuntary, erratic, or twisting movements of the face, arms, legs, or trunk (dyskinesias), and motor fluctuations. In epilepsy, DBS works to reduce the overall seizure burden, including the frequency, severity, and duration of seizures.
Your healthcare provider may also explore DBS when medications are ineffective or initially effective but become less effective, or their side effects interfere with daily activities.
While DBS is a surgical treatment and all surgeries have risks, the risks associated with it are relatively low. Treatment won’t cure your condition, but it can offer significant relief. Medication may still be needed to help manage symptoms, although it’s often taken at reduced dosages following the DBS procedure.

Asleep Deep Brain Stimulation (Asleep DBS)
Through intraoperative imaging and computer-guided neurosurgery advancements, we can now offer the asleep procedure to all of Barrow Neurological Institute’s DBS patients for movement disorders and epilepsy.
Early DBS procedures for movement disorders required a patient to be awake and temporarily off of their medications. During surgery, a neurosurgeon would use specialized monitoring equipment to determine a safe path to the part of the brain where the DBS electrodes would be implanted. The patient would then be asked to provide responses to help verify the proper placement of the electrodes.
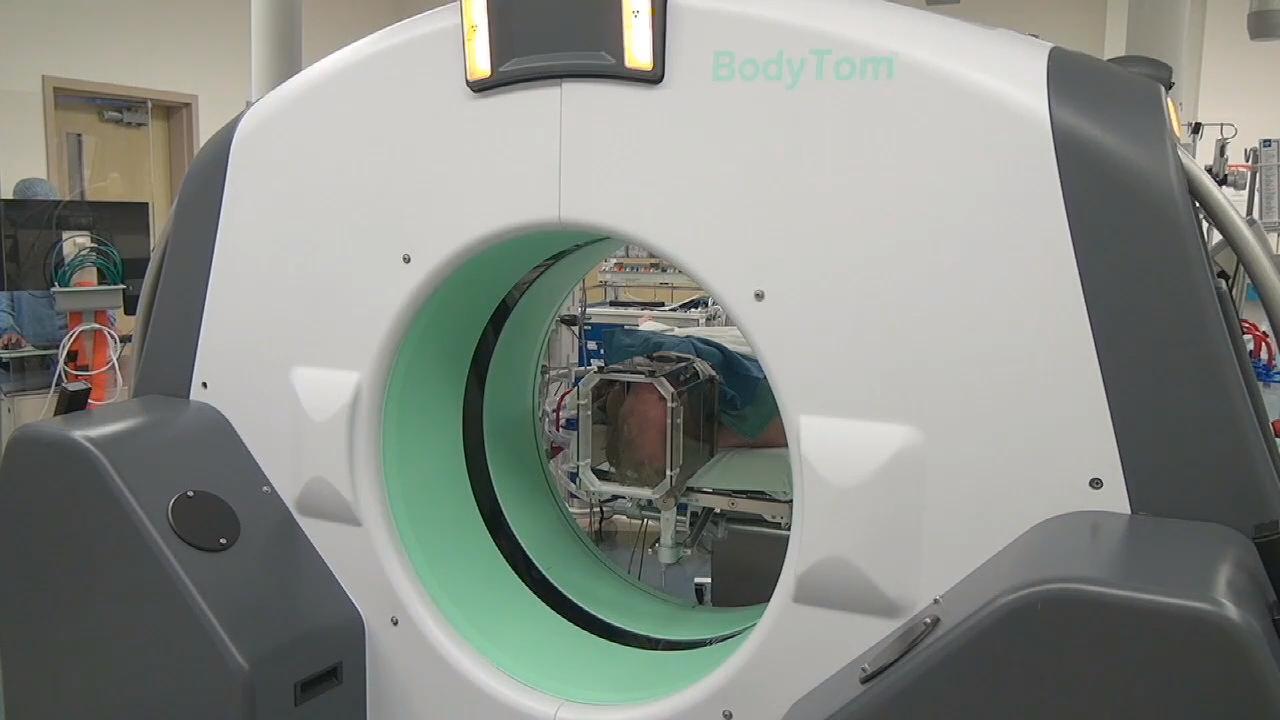
With asleep DBS, the goal is to preoperatively plan the placement of the electrodes in the targeted areas. Asleep DBS surgery is performed while a patient is under general anesthesia and a computed tomography (CT) machine is used to target and verify the placement of electrodes during surgery.
Here’s how it works:
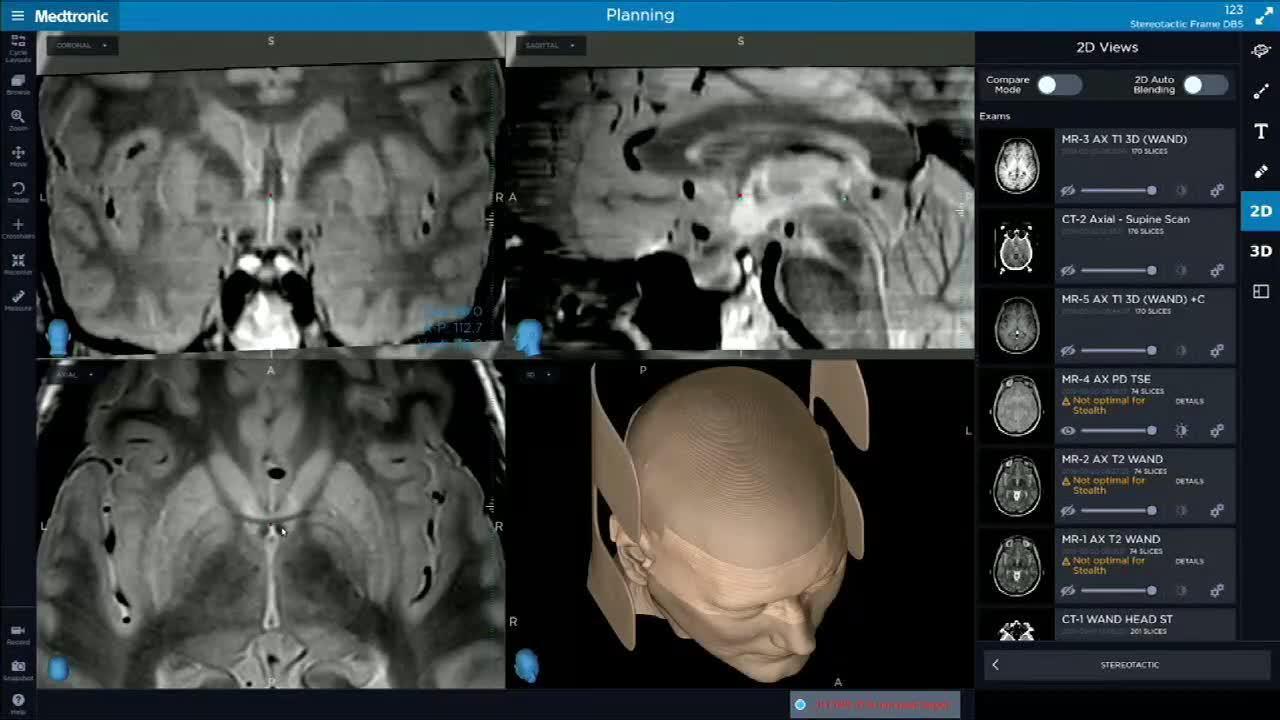
- Preoperative imaging: Prior to surgery, your medical team will use highly detailed magnetic resonance imaging (MRI) or CT imaging to precisely locate the areas of your brain where the electrodes should be implanted.
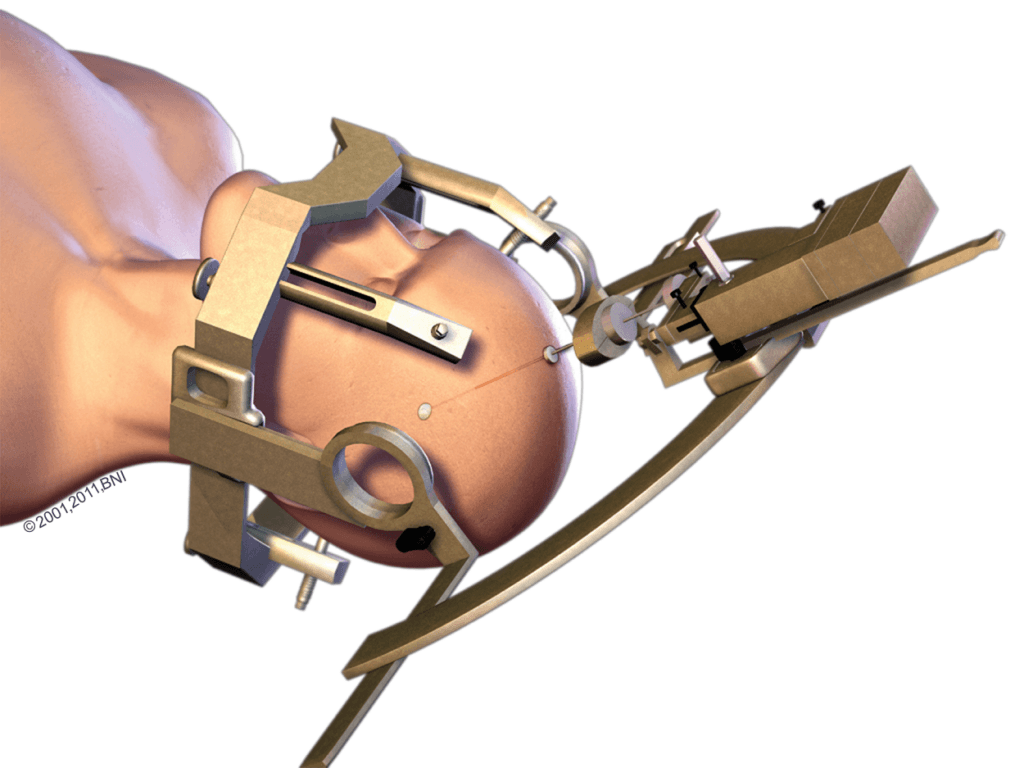
- Electrode implantation: Under anesthesia, your neurosurgeon will attach a stereotactic frame to your head to keep it still and guide the placement of the electrodes to the precise location established during preoperative planning. A small hole is drilled in your skull after the frame is placed and the electrodes are gently positioned in the correct location in your brain using image guidance and metal attachments that connect to the stereotactic frame.
- Programming: After the electrodes are successfully implanted, they’reconnected to the pulse generator, the pacemaker-like device implanted just below your collarbone. Once you’ve recovered from the procedure, your medical team will program the pulse generator to deliver the appropriate amount of electrical impulses to relieve your symptoms.
- Follow-up care: Most patients are required to stay in the hospital for one day after surgery. Frequent follow-up appointments with your medical team are also scheduled to monitor your progress and adjust the pulse generator for the best settings specific to you. You may even see a reduction in medication usage following DBS surgery.
Overall, asleep DBS offers a more comfortable and less stressful patient experience. Even if you’re not apprehensive about the prospect of awake brain surgery, research has shown no additional benefits to choosing awake surgery over asleep surgery.
In other words, good candidates for DBS almost always make excellent candidates for asleep DBS.
DBS for Movement Disorders
When it comes to movement disorders, DBS can target specific areas that control movement—like the subthalamic nucleus (STN), the globus pallidus internus (GPi), or the ventral intermediate nucleus (VIM) of the thalamus—and modulate the dysfunctional neural circuits causing symptoms. This, in turn, leads to improved motor control because the stimulation normalizes electrical activity.
DBS has been shown to be highly effective in reducing motor symptoms in movement disorders like Parkinson’s, frequently resulting in a significant reduction in medication.
DBS for Epilepsy
The goal of DBS in epilepsy is to interrupt the abnormal electrical activity that leads to seizures and reduce their frequency, intensity, and duration; particularly when seizures are drug-resistant. Common target areas include the anterior nucleus of the thalamus (ANT) and the centromedian nucleus (CM) of the thalamus. However, the type of epilepsy and the specific patterns of seizure activity will determine an individual’s targeted areas.
While the efficacy of DBS for epilepsy can vary—it’s reported to reduce seizure frequency by nearly 50 percent in many patients—complete eradication of symptoms is less common than with DBS for movement disorders.
Programming and Adjustment
DBS systems for both movement disorders and epilepsy require careful programming and regular adjustments to optimize the effects of deep brain stimulation. That said, system settings will vary across different diseases, their objective targets, and within each patient, depending on their desired outcomes.
Common Questions about Deep Brain Stimulation (DBS)
Who is a good candidate for DBS?
You may be a good candidate for DBS if you have epilepsy, Parkinson’s disease, or another movement disorder with moderate to severe symptoms that don’t respond to medications, the medications aren’t working as well as they once did, or are causing severe side effects. DBS has no age limit, although the strongest candidates are those in otherwise good health.
Is DBS safe?
DBS was introduced in the 1980s and is recognized as a safe and effective treatment for numerous neurological diseases and movement disorders. It’s estimated that around 12,000 DBS surgical treatments happen every year. What’s more, DBS has been used to treat more than a quarter million people for a variety of neurological conditions.
While DBS is a surgical treatment and all surgery has risks, the risks associated with DBS are low and can include bleeding or infection at the site of placement. Complications such as bleeding, strokes, or swelling of brain tissue are rare but may result from the mechanical stress of device placement.
Other complications can include headaches, new or worsening seizures, temporary pain post-surgery, or a secondary surgery to replace parts of the device that have eroded with use or broken down.
What kind of results can I expect?
DBS won’t cure your condition, but it can offer significant relief. You may still need to take medication to manage your symptoms, although often at reduced dosages.
Researchers who have followed patients after DBS treatments have found many continue to improve their symptoms for several years after the procedure. As with all other areas of life, it’s essential to maintain a healthy lifestyle with regular exercise and a balanced diet to optimize your DBS benefits.
At this time, Parkinson’s disease is a progressive disorder that cannot be stopped entirely. Even while DBS continues to work on tremors, stiffness, and slowness, other symptoms like speech impairment, gait freezing, balance problems, and dementia may still occur. We recommend these risks be discussed with your medical team and weighed against the potential benefits of DBS.
Can I have magnetic resonance imaging (MRI) done if I’ve had DBS surgery?
Yes, you can have an MRI done after having DBS surgery, but there are considerations and precautions to take. Modern DBS systems are often designed to be MRI conditional, which means they can be safe under specific conditions specified by the DBS manufacturer. These include the type of MRI, the strength of the magnetic field, and the body area being scanned.
Before an MRI, it’s crucial to check the specifications of your DBS system. Healthcare providers and technicians must adjust the MRI machine’s settings accordingly to ensure it doesn’t interfere with or damage your DBS system. Always inform the healthcare professional who manages your DBS therapy if you require an MRI scan. They will coordinate with the MRI technicians to ensure all safety protocols are followed.
It’s also wise to carry information about your DBS system, like the model and manufacturer’s guidelines regarding MRIs, so that MRI staff can appropriately prepare and adjust settings. In some cases, your DBS device may need to be temporarily turned off before the imaging is done to prevent any potential interactions between the MRI’s magnetic field and the electronic components of the DBS system.
Can I fly with a DBS device?
Traveling by air is generally safe for people with DBS implants. It’s a good idea to carry the medical device card issued after your surgery that provides information about your DBS system. This card typically includes details like the type of device, the manufacturer, and emergency contact information and can be helpful during security screenings to explain the presence of your device. While DBS devices aren’t usually affected by airport security scanners, a manual check is frequently advised to avoid potential issues.
Moreover, you won’t need to turn off your DBS system during the flight—it won’t be affected by the aircraft’s systems and will function normally. After flying, if you experience any discomfort or suspect that the device settings might have been altered (which is very unlikely), consult your healthcare professional or a specialist.
Information and Resources about Deep Brain Stimulation (DBS)
References
- Olson MC, Shill H, Ponce F, Aslam S. Deep brain stimulation in PD: risk of complications, morbidity, and hospitalizations: a systematic review. Front Aging Neurosci. 2023 Nov 17;15:1258190. doi: 10.3389/fnagi.2023.1258190. PMID: 38046469; PMCID: PMC10690827.
- Yang AI, Raghu ALB, Isbaine F, Alwaki A, Gross RE. Sensing with deep brain stimulation device in epilepsy: Aperiodic changes in thalamic local field potential during seizures. Epilepsia. 2023 Nov;64(11):3025-3035. doi: 10.1111/epi.17758. Epub 2023 Sep 11. PMID: 37607249.
- Schulder M, Mishra A, Mammis A, Horn A, Boutet A, Blomstedt P, Chabardes S, Flouty O, Lozano AM, Neimat JS, Ponce F, Starr PA, Krauss JK, Hariz M, Chang JW. Advances in Technical Aspects of Deep Brain Stimulation Surgery. Stereotact Funct Neurosurg. 2023;101(2):112-134. doi: 10.1159/000529040. Epub 2023 Feb 21. PMID: 36809747; PMCID: PMC10184879.
- Yang AI, Isbaine F, Alwaki A, Gross RE. Multitarget deep brain stimulation for epilepsy. J Neurosurg. 2023 Jul 14;140(1):210-217. doi: 10.3171/2023.5.JNS23982. PMID: 37486888.