
Craniopharyngioma
Overview
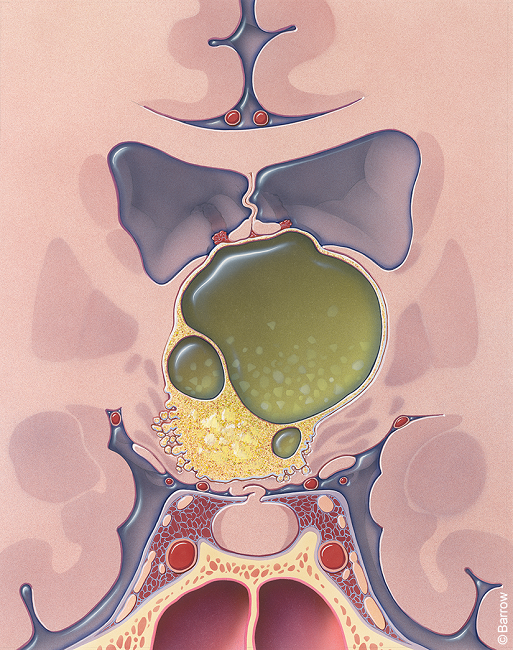
Craniopharyngiomas are rare, non-cancerous tumors that develop near the pituitary gland at the base of the brain. The pituitary gland is a small organ that secretes hormones that are responsible for numerous functions, such as growth and the production of other hormones in the body.
Craniopharyngiomas tend to be slow-growing and don’t spread, or metastasize, to other parts of the brain or body parts. Despite this, they can cause significant health problems because they grow close to critical brain structures.
As a craniopharyngioma grows and presses on nearby parts of the brain, it can affect the function of the pituitary gland. It can also cause vision loss due to proximity to the optic nerves and threaten other vital structures in the brain. If left untreated, most craniopharyngiomas are aggressive and invade surrounding structures.
Two types of craniopharyngiomas are known at this time: the adamantinomatous variant (ACP) and the papillary variant (PCP). While ACPs and PCPs have distinct features, they can cause similar symptoms due to their location near the same important brain structures.
- Adamantinomatous Variant (ACP): Adamantinomatous craniopharyngiomas are the most common, accounting for approximately 85-95 percent of all instances. These tumors tend to occur more often in children and adolescents, although they can be found in adults.
- Papillary Variant (PCP): Papillary craniopharyngiomas are less common, accounting for approximately 5 to 15 percent of all instances. PCPs tend to occur in adults. At Barrow, we are leading a national consortium called RAPID to study craniopharyngiomas. The goal of this effort is to develop treatments for craniopharyngiomas.
What causes craniopharyngioma?
Most craniopharyngiomas occur sporadically, which means their cause isn’t known. They’re thought to come from tissue remnants left in the embryo during the development of the craniopharyngeal duct.

Craniopharyngioma Symptoms
Craniopharyngiomas are generally detected when they begin pressing on the brain, pituitary gland, nearby blood vessels, optic nerves, or optic chiasm, where the two optic nerves intersect just before entering the brain.
While symptoms will vary, the most common symptoms of a craniopharyngioma include persistent or reoccurring headaches, vision problems, and endocrine dysfunction or deficiencies. The exact location of the craniopharyngioma will determine the specific symptoms.
If the tumor compresses the pituitary gland or pituitary stalk, symptoms can include:
- Stunted growth
- Delayed puberty
- Loss of normal menstrual function
- Loss of sexual desire
- Increased sensitivity to cold
- Fatigue
- Constipation
- Nausea
- Diabetes insipidus, a rare condition where the body to makes too much urine
- Excessive thirst and excessive urination
- Increased prolactin levels, which can cause milky discharge from the breasts
If the tumor compresses the optic nerve or optic chiasm, symptoms can include:
- Blurred vision
- Decreased visual field, or partial vision loss
- Blindness
If the tumor compresses the hypothalamus, the part of the brain that communicates between the endocrine system and the central nervous system, symptoms can include:
- Obesity
- Increased drowsiness
- Body temperature regulation abnormalities
- Diabetes insipidus is a rare disorder that causes the body to make too much urine
- Personality changes
- Confusion
- Vomiting
Depending on the location of the tumor and its effects on surrounding structures, craniopharyngiomas can cause other neurological symptoms, such as seizures and difficulties with balance and coordination.
The severity and combination of symptoms often vary from person to person. To make diagnosis more challenging, symptoms of craniopharyngiomas can overlap with those of other medical conditions. If you’re concerned about experiencing new or persistent symptoms that align with these descriptions, you should speak to your healthcare provider as soon as possible.
Diagnosis
The following exams and imaging options are frequently used to diagnose a craniopharyngioma:
- Physical and neurological exam: Your healthcare provider will first ask about your symptoms, overall health, and family history of brain tumors or genetic conditions. Next, they’ll complete a neurological examination to analyze neurological function, including reflexes, coordination, strength, and sensation.
- Magnetic Resonance Imaging (MRI): Neuroimaging studies are crucial in visualizing the brain and identifying abnormalities. An MRI provides detailed brain images and can help visualize a craniopharyngioma’s location relative to other nearby structures, like the pituitary gland, optic nerves, and surrounding tissue.
- Computed Tomography (CT) Scan: CT scans rely on X-rays to create detailed cross-sectional images of the brain and can help evaluate the tumor’s size and location, particularly if an MRI is contraindicated.
- Blood tests to measure hormone levels: Craniopharyngiomas can cause hormonal imbalances due to their proximity to the pituitary gland. Hormone testing is usually done to look for hormone deficiencies, like thyroid deficiency, growth hormone deficiency, adrenal insufficiency, and other abnormalities.
- Visual field testing: Visual field testing can be done to look for deficits caused by the craniopharyngioma’s compression or damage to the optic nerves.
Craniopharyngioma Treatments
For most patients, surgical removal of a craniopharyngioma is the first course of treatment because it removes as much of the tumor as possible and can relieve pressure on the brain.
Surgical Treatments
Neurosurgeons most often remove craniopharyngiomas through one of two surgeries: a craniotomy, which is an opening made in the skull, or endoscopic transsphenoidal surgery, which consists of surgery using the nasal passages to reach the tumor safely. The location of the craniopharyngioma will influence which surgical procedure your neurosurgeon recommends.
- Transsphenoidal Surgery: This surgical approach allows the neurosurgeon to access the craniopharyngioma through the nasal passages and the sphenoid sinus. It allows the neurosurgeon to avoid important brain structures by reaching the pituitary gland from underneath the brain. Transsphenoidal surgery minimizes complication risk, leaves no visible scar, and lends itself to a faster recovery. For these reasons, it is the most common surgical procedure used to treat craniopharyngiomas at Barrow Neurological Institute.
- Craniotomy: During a craniotomy, a neurosurgeon makes an incision in the scalp, removes a portion of the skull, and accesses the brain to remove the tumor. The surgeon may use specialized tools, such as microscopes, endoscopes, or intraoperative imaging techniques, to visualize and safely remove the tumor while minimizing damage to surrounding brain tissue. Your neurosurgeon may recommend this approach for craniopharyngiomas that they can’t access safely via transsphenoidal surgery.
Nonsurgical Treatments
If your neurosurgeon is not able to remove the entire tumor, radiation therapy can destroy existing tumor cells and stop further growth.
- Stereotactic radiosurgery: Stereotactic radiosurgery is a non-invasive treatment option for brain tumors that are particularly small or located in areas of the brain that are difficult to access via traditional surgery. Stereotactic radiosurgery delivers a highly focused radiation beam to the tumor, destroying it while minimizing radiation exposure to surrounding healthy tissue. The most common types of stereotactic radiosurgery include:
- Gamma Knife radiosurgery: This option destroys tumor tissue through radiation beams focused on a precise tissue area and is only lethal to cells within the immediate vicinity. The Gamma Knife can only treat lesions in the head and involves attaching a metal frame to the skull to target beams of radiation accurately.
- CyberKnife radiosurgery: This technique uses targeted energy beams to destroy tumor tissue while sparing healthy tissue. It uses image-guided robotics to deliver surgically precise radiation to help destroy tumors like craniopharyngiomas.
Recently, researchers have developed medications for papillary craniopharyngioma. These may be considered as part of a comprehensive treatment plan.
Successfully treating a craniopharyngioma requires an expert team of healthcare professionals. For example, craniopharyngioma patients need a neurosurgeon, endocrinologist, ophthalmologist, and radiation specialist, among others.
At Barrow Neurological Institute, we’re proud to be the most experienced Pituitary Center in the Southwest. Year after year, no other hospital performs more pituitary surgeries than we do. Regarding craniopharyngiomas, we treat more patients with these tumors than any other center in Arizona.
Common Questions
How common are craniopharyngiomas?
Craniopharyngiomas are rare—fewer than 1,000 people in the U.S. are diagnosed with one each year.
While they are one of the most common brain tumors in children, craniopharyngiomas are less common in adults. They make up 5 to 10 percent of all childhood brain tumors and between 2 to 5 percent of all primary brain tumors, otherwise known as tumors that start in the brain or the brain’s surrounding tissues.
Who gets craniopharyngiomas?
Craniopharyngiomas can occur in individuals of any age, but are most commonly diagnosed in two age groups: children between the ages of 5 and 14 and adults between 40 and 60.
While craniopharyngiomas can affect all genders equally, some studies suggest a slightly higher incidence in males than females, particularly in children.
What is the prognosis for those with craniopharyngioma?
The prognosis for individuals diagnosed with a craniopharyngioma depends on a combination of factors, like tumor size and location, age, and a person’s response to treatment. Considerations that will affect prognosis include:
- Tumor characteristics: The size and location of a craniopharyngioma can significantly impact its prognosis. Larger tumors or tumors located near critical structures in the brain can be more challenging to treat.
- Degree of surgical removal: Complete surgical removal of a craniopharyngioma is tied to better outcomes because it reduces the risk of recurrence and progression. That said, a complete removal is often more complicated for tumors found in complex or deep-seated areas of the brain.
- Hormonal deficiencies: Due to their proximity to the pituitary gland, craniopharyngiomas can cause hormonal imbalances and deficiencies. Conversely, growth hormone deficiency, thyroid hormone deficiency, or adrenal insufficiency can have long-term implications for a person’s quality of life. A diagnosis with hormone replacement therapy can be vital for managing hormone imbalances and improving outcomes.
- Risk of recurrence: Craniopharyngiomas have a relatively high recurrence rate. Children tend to have a higher recurrence rate than adults.
Can craniopharyngioma be prevented?
Craniopharyngiomas are sporadic tumors, meaning their cause is not well understood. While you can’t prevent yourself from getting a craniopharyngioma, having a regular checkup with your doctor can help to identify early signs of a craniopharyngioma.
Resources
American Brain Tumor Association
References
- Karsy M, Kshettry V, Gardner P, Chicoine M, Fernandez-Miranda JC, Evans JJ, Barkhoudarian G, Hardesty D, Kim W, Zada G, Crocker T, Torok I, Little A. The RAPID Consortium: A Platform for Clinical and Translational Pituitary Tumor Research. J Neurol Surg B Skull Base. 2022 Dec 30;85(1):1-8. doi: 10.1055/a-1978-9380. PMID: 38274483; PMCID: PMC10807961.
- Zaidi HA, Chapple K, Little AS. National treatment trends, complications, and predictors of in-hospital charges for the surgical management of craniopharyngiomas in adults from 2007 to 2011. Neurosurg Focus. 2014 Nov;37(5):E6. doi: 10.3171/2014.8.FOCUS14366. PMID: 25363434.



