
OLIF Spine Surgery Saves Top Instructor’s Golf Swing
Golf has played a central role in Jim McLean’s life since his childhood. He’s amassed a long list of accomplishments in the sport—spanning his amateur, professional, and teaching careers.
But after nearly two decades of worsening lower-back pain, Jim learned he needed spinal fusion surgery. Concerned that the procedure could force him to retire his clubs for good, he turned to the golf community for help.
Fellow golfers pointed Jim toward Randall Porter, MD, a neurosurgeon at Barrow Neurological Institute in Phoenix. Dr. Porter assured Jim that he could reduce Jim’s back pain while still maintaining much of his spinal mobility.
“I liked Barrow a lot, and I liked those good recommendations,” Jim said. “I also liked the fact that Dr. Porter is a golfer too, so he understood what I’d need to be able to play.”
A Life on the Green
As a kid growing up in Seattle, Jim demonstrated that he had a promising future in golf. He dabbled in other sports—baseball, football, basketball—but golf was ever-present in his life. Both of his parents played golf, and their family home was located near a course.
“I just had early success playing,” Jim recalled. “So I ended up dropping baseball and playing golf in the summers.”
Jim went on to win more than 50 junior and amateur titles in the Pacific Northwest. He earned a four-year scholarship to play golf at the University of Houston, where he as an All-American athlete. Jim took first place in three National Collegiate Athletic Association tournaments and played on an NCAA championship team. He participated in two United States Opens and the Senior U.S. Open and, in 1972, made the cut at the Masters Tournament.
Jim played two years of professional golf after college, winning the Westchester PGA Championship and three PGA Club Pro winter events.
Today, Jim is a renowned golf instructor and the CEO of the No. 1 ranked golf school in America, which has eight locations across four different countries. Golf Digest named him the sixth “Best Teacher in America” in its 2022-23 listing.
Jim is a member of multiple golf halls of fame, both for his instruction and playing record. Many golfers know him as the father of the “X-factor” swing, a method for generating power to drive the ball farther.
Exploring Options for Spinal Fusion
But as Jim’s teaching career began to thrive, intensifying back pain threatened the future of his own game.
“It started for me when I was in my early 50s,” said Jim, who is now 72. “I had epidurals for 15 years and took medications. I was still playing quite a bit, but it just started getting worse and the epidurals weren’t working.”
Jim had degenerative disc disease, a condition that occurs when the discs between the bones of the spine wear down and no longer provide adequate cushioning for spinal movements.
While it’s normal for spinal discs to wear down with age, degenerative disc disease is being diagnosed in an increasing number of young golfers. This may be explained by the evolution of the golf swing, a topic explored by Barrow spine surgeons and discussed in a Journal of Neurosurgery: Spine paper.
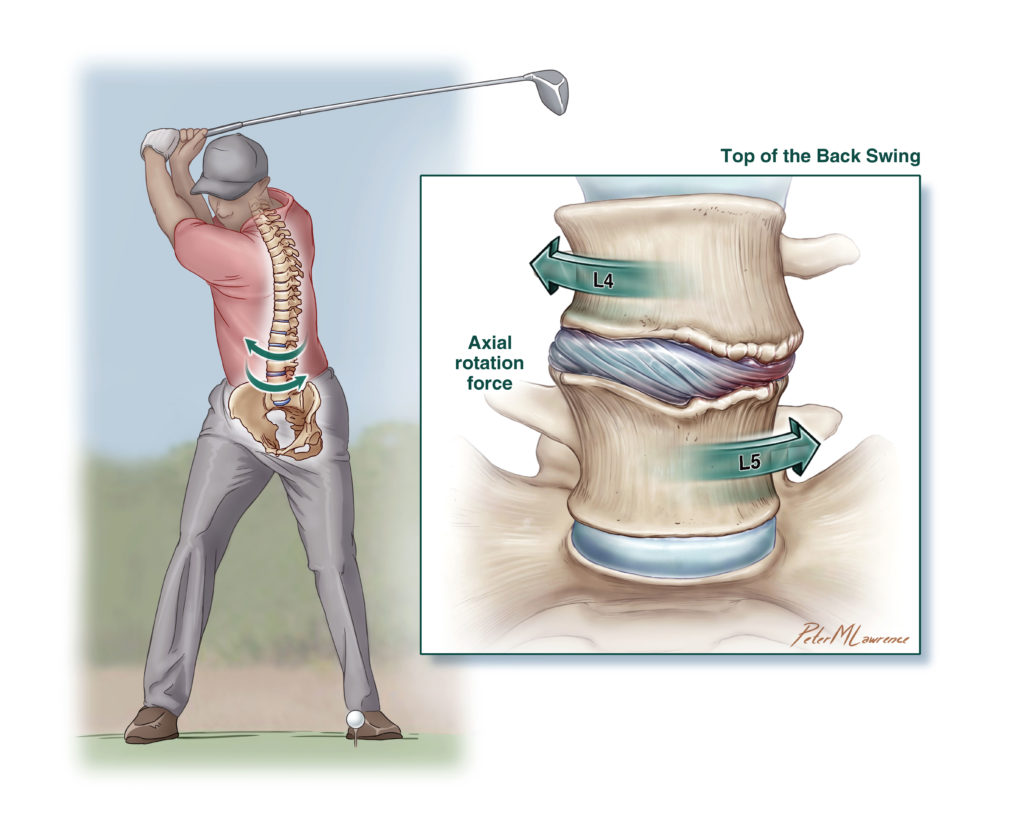
When today’s golfers drive the ball more than three football fields in distance, they twist their spines with a force similar to being ejected from a military aircraft. Golfers repeatedly endure this impact, taking an average of more than 300 swings per day over many years, or even decades, of participating in the sport.
Jim underwent a spinal procedure in New York, but it was unsuccessful at relieving his pain—which had started to radiate down his legs.
“I could still teach; it just made playing difficult,” he said. “I was just not happy with the whole thing.”
Jim consulted with various doctors, all of whom recommended a spinal fusion. This procedure involves removing diseased discs and joining the adjacent vertebrae together. While this procedure relieves pain, it also eliminates movement at the level of the spine where it is performed. The surgeon may place instrumentation—such as metal plates, rods, and screws—to stabilize the spine as the bones naturally fuse together.
One spine surgeon told Jim he would need a rod on each side of his spine. The rods would extend about a foot and a half, from the mid-back to the base of the spine, and be held in place with 18 pedicle screws.
Worried about having that much hardware in his back, Jim sought another opinion. He scheduled an appointment with Dr. Porter, who had recently performed a minimally invasive spinal fusion on Jim’s longtime friend and fellow golfer Joe Colello.
Minding What Matters Most™: Preserving Movement with OLIF
When Jim met with Dr. Porter in August of 2018 and shared the other surgeon’s plans, Dr. Porter warned Jim that such an invasive procedure would inhibit his ability to rotate his spine. In other words, Jim would not likely be able to swing a golf club again.
Instead, Dr. Porter suggested placing spacers between the vertebrae at four levels of Jim’s spine. These devices would restore the height between the vertebrae while preserving spinal mobility.
“We’ve shown in our biomechanics spine research lab at Barrow that if you place rods and screws and cages, you’ll immobilize the spine by 80 to 100 percent,” Dr. Porter explained. “Performing an OLIF on four levels with spacers would limit range of motion at those areas by only 50 percent.”
The OLIF approach, short for oblique lateral interbody fusion, involves accessing the spine using a natural corridor on the side of the body. Rather than cut through Jim’s back muscles, Dr. Porter would use computer-assisted imaging guidance to navigate the spacers to their precise locations within the spine.
“Our approach was a motion-preservation option—without rods, without the stiffness that comes with rods, and without the risk of adjacent level disc disease,” Dr. Porter said. “You can always do more surgery, but you can’t undo too much surgery.”
As doctors, we have to take the time to know our patients, know their baseline level of activity and what kind of activity they want to get back, and tailor our surgeries to their lifestyle.
Randall Porter, MD, Barrow Neurosurgeon
The Spine Program at Barrow has treated many professional and amateur golfers, both with and without surgery. When surgery is necessary, Barrow spine surgeons recommend the least invasive option possible and can often avoid implanting rods and screws. Through minimally invasive techniques, they can reduce muscle trauma, scar tissue, blood loss, time in surgery, and recovery time.
Jim traveled from Miami to Phoenix to undergo an OLIF with Dr. Porter. He stayed with his friend and fellow Barrow patient, Joe, who has a winter home in the Valley.
“I was nervous about the surgery, but I just felt I was in good hands,” Jim said. “Dr. Porter is an extremely great doctor. He’s very smart, he had great recommendations, he speaks all over the world, he’s on top of all the things to do, and I think he’s a very calming person too. I thought everybody took great care of me there.”
After taking a few weeks to recover, Jim returned to Miami and began rehabilitation with a specialist recommended by Dr. Porter.
“I got back to teaching pretty fast,” Jim said. “Then I started hitting balls probably about six months later.”
Today, Jim is able to teach and play golf with significant pain relief.
“Telling a patient to never golf again is devastating for people who have been golfing every weekend for their whole life,” Dr. Porter said. “As doctors, we have to take the time to know our patients, know their baseline level of activity and what kind of activity they want to get back, and tailor our surgeries to their lifestyle.”

