NIH Funds Barrow Study of Aging, Cell Senescence in Brain Aneurysm Rupture
The Barrow Aneurysm and AVM Research Center has received a $3 million, five-year R01 grant from the National Institutes of Health (NIH) to study the role of aging and cellular senescence in the rupture of brain aneurysms.
Senescence describes the phenomenon in which our cells reach their finite number of divisions but don’t die off. Instead, these “zombie cells” accumulate in the body, unable to carry out normal functions or produce new cells to take their place. Additionally, senescent cells can actually damage nearby healthy cells and tissues by secreting unnecessary levels of pro-inflammatory proteins called cytokines.

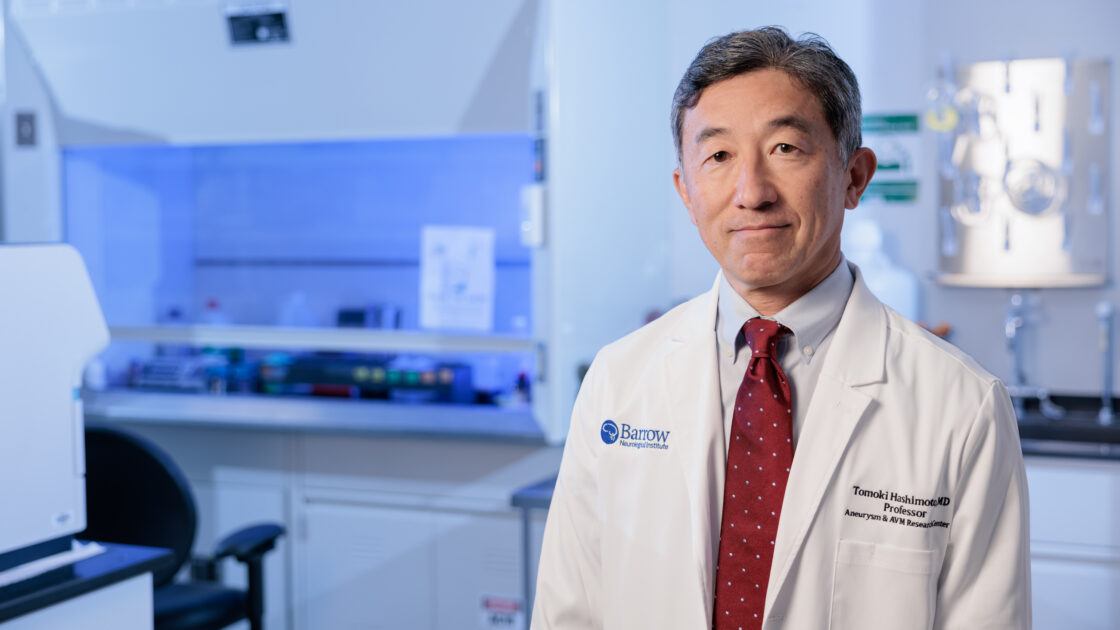
The number of senescent cells in our bodies normally increases with age, and clinical studies have consistently identified aging as a risk factor for aneurysm rupture. That led Tomoki Hashimoto, MD, and his colleagues to wonder if they could connect these dots.
“Our idea was that in brain aneurysm, cells may become senescent and start producing these toxic cytokines,” said Dr. Hashimoto, director of translational neurovascular research at Barrow. “Those cytokines may cause damage to the aneurysm wall and lead to rupture.”
We’ve traditionally thought of age as a non-modifiable risk factor for aneurysm rupture, unlike high blood pressure and smoking. However, Dr. Hashimoto has noted increasing evidence that suggests we may be able to turn back the clock after all, thanks to advancements in aging research and drug development. But first, the link between aging, cell senescence, and aneurysm rupture must be more firmly established. That’s exactly the aim of Dr. Hashimoto’s NIH-funded project, along with proof-of-concept that medications can modulate the aging process to reduce aneurysm risk.
Coming of Age: From Idea to Funding
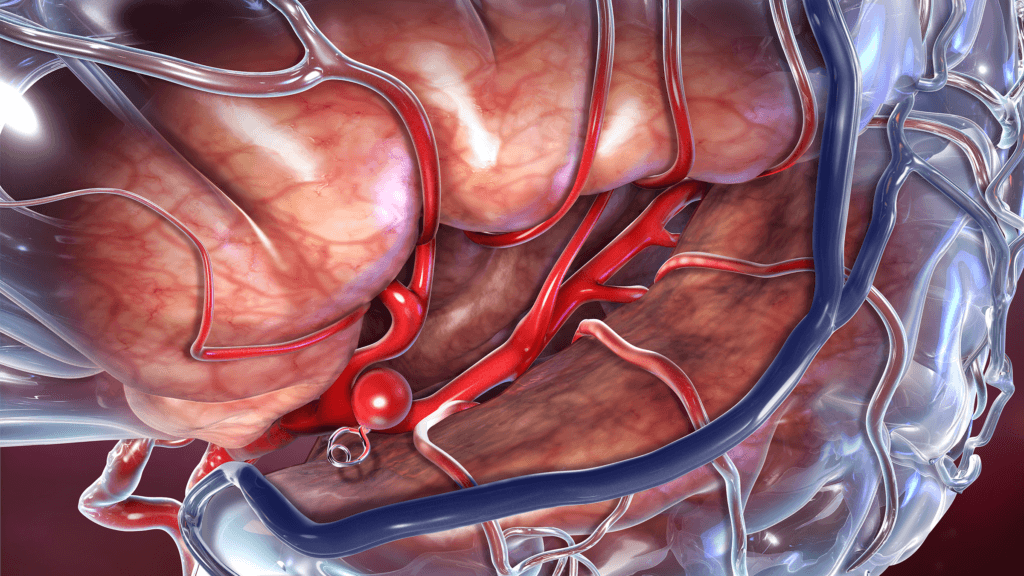
A brain aneurysm is a weak spot along a blood vessel in the brain that bulges outward. Often described as having a balloon-like appearance, an aneurysm may burst and bleed into the brain. This is called a hemorrhagic stroke, and it can cause life-threatening complications and permanent disability. According to the Brain Aneurysm Foundation, a brain aneurysm ruptures every 18 minutes in the United States. Worldwide, brain aneurysms account for nearly 500,000 deaths each year.
Dr. Hashimoto grew increasingly interested in aging as a risk factor for aneurysm rupture after discussions with neurosurgeons at Barrow, including President and CEO Michael T. Lawton, MD. While reviewing epidemiological data for insights into who experiences aneurysm rupture and why, they narrowed in on aging for a couple of reasons. “Aging affects everyone,” Dr. Hashimoto said, “and the biology of aging is an up-and-coming field.”

Over the last decade, researchers have made strides in better understanding biological processes associated with aging. This includes the discovery of premature senescence resulting from chronic conditions, like diabetes, high blood pressure, and a buildup of plaque in the arteries known as atherosclerosis. These conditions may induce early senescence through inflammation and changes to hemodynamics, or how the blood flows through the vessels.
“I have long felt that aneurysm formation is the end result of hemodynamic punishment that arterial walls endure as blood flows against them under pressure, so studying the effects of aging on aneurysm formation will be, I think, very enlightening,” said Dr. Lawton, who founded the Barrow Aneurysm and AVM Research Center and specializes in the surgical treatment of vascular abnormalities like aneurysms. “I congratulate Tomoki on yet another exciting area of exploration in aneurysm biology,” he added.
Equipped with funding from Barrow Neurological Foundation and a unique mouse model, Dr. Hashimoto gathered promising preliminary data to submit to the National Institute on Aging at NIH. When the male mice received a drug known as a senolytic—to which these mice are designed to be sensitive—they had a reduced risk of aneurysm rupture. Senolytics selectively clear senescent cells and are currently used for chemotherapy.
In Its Infancy: Study to Test Fundamental Question
Dr. Hashimoto will continue to use this mouse model, which was developed at another laboratory, to validate his preliminary findings. He is collaborating with Satoru Eguchi, MD, PhD, a cardiovascular researcher at the Lewis Katz School of Medicine at Temple University in Philadelphia.
“This project is testing a very basic question: When we eliminate senescent cells, can we decrease aneurysm rupture?” He explained. “We’ve got a really exciting tool to answer this question. We have experiments showing that preliminarily, so we’re expanding those experiments to make sure this is a true phenomenon.”
Although senolytics can help answer this fundamental question, Dr. Hashimoto sees senomorphic drugs as a more suitable candidate for future human trials, due to their relative tolerability.
“We want to use a drug that has less toxicity, so that’s where senomorphics come in,” he said. “We may be able to use them for prevention of aneurysm rupture for patients who are not the best candidates for surgery, or we may be able to use them as an additional therapy. That’s my long-term hope for this study.”
