
Osteoporosis of the Spine
Osteoporosis Overview
Osteoporosis is when the bones in your body become weak and brittle, making them more prone to fractures from minor falls or everyday activities. Osteoporosis is a systemic disease that can affect any bone in your body, including the bones that make up your spine. This condition is more common as you age, particularly in women after menopause, due to lower estrogen levels. Other factors that can increase your risk include:
- Poor diet
- Lack of exercise
- Smoking
- Excessive alcohol consumption
- Certain medical conditions or medications
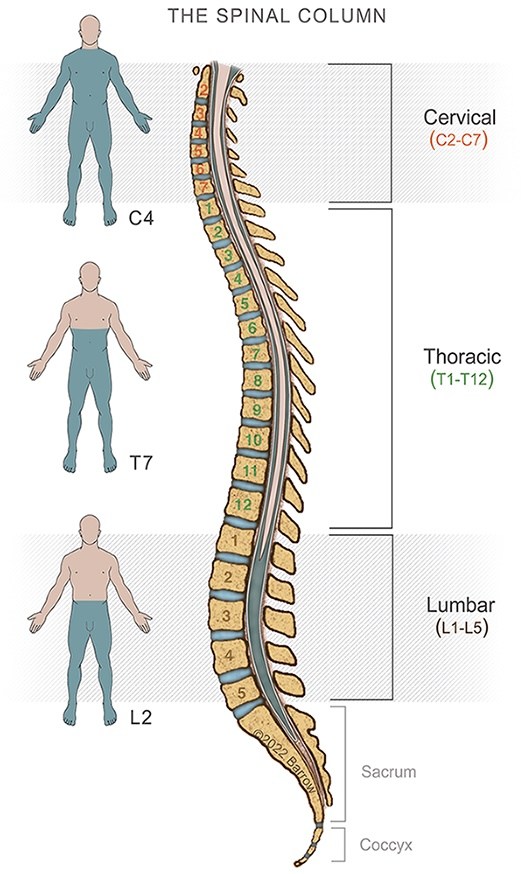
Often, spinal osteoporosis doesn’t show symptoms until a bone breaks. When symptoms do occur, you might experience back pain, loss of height, or a stooped posture due to fractures in the spine. Diagnosing this condition typically involves a bone density test, which measures the strength of your bones, and X-rays, which can reveal fractures or bone loss.
Treatment aims to strengthen your bones and prevent fractures. This can include medications to slow bone loss or to increase bone mass, ensuring you get enough calcium and vitamin D, engaging in weight-bearing exercises, and making lifestyle changes like quitting smoking, reducing alcohol intake, and eating a healthy diet.
Living with spinal osteoporosis requires ongoing management. Staying active, maintaining a balanced diet, and following your doctor’s advice on medications and supplements are essential. Regular check-ups are necessary to monitor your bone health. If you have any concerns or questions about your condition, your healthcare provider can help you develop a plan to keep your bones as healthy as possible.

Osteoporosis and Spine Surgery
If you have osteoporosis and are considering spine surgery, several essential factors must be remembered. Osteoporosis weakens the bones, which can complicate both the surgery itself and the recovery process.
Here are the key considerations:
- Bone Quality: Osteoporotic bones are more fragile, making it harder for surgeons to anchor screws and other hardware needed to stabilize the spine. Poor bone quality can increase the risk of hardware loosening or failing after surgery.
- Fracture Risk: The weakened bones are more susceptible to fractures, both during the surgical and postoperative periods. Surgeons must take extra care to avoid causing fractures during the operation.
- Healing and Recovery: Osteoporosis can slow down the healing process. Less dense bones have a reduced capacity to repair themselves, which can prolong recovery time and affect the overall success of the surgery.
- Surgical Techniques: Surgeons may need to modify their techniques to accommodate the fragile bones. This might involve using specialized screws or implants designed for osteoporotic bones or employing less invasive surgical methods to minimize trauma to the spine.
- Pre-Surgical Preparation: Patients with osteoporosis may need a pre-surgical evaluation to assess bone density and overall health. Optimizing bone health before surgery can be an essential step.
- Post-Surgical Care: After surgery, careful monitoring and follow-up are crucial. Patients may need to take additional medications to support bone health and should follow a tailored rehabilitation program to aid recovery while minimizing the risk of new fractures.
- Alternative Treatments: Sometimes, your doctor might recommend non-surgical treatments as safer options. These include physical therapy, pain management, and medications to strengthen bones and alleviate symptoms.
Fortunately, spinal osteoporosis is a treatable disease. For people with spine conditions that are not immediately life-threatening or that do not present a risk of imminent paralysis, it may be better to work with an endocrinologist with experience in treating bone diseases to achieve optimal bone health before having surgery.
Ultimately, the decision to proceed with spine surgery if you have osteoporosis requires a thorough evaluation by your healthcare team. They will consider the severity of your osteoporosis, specific spine issues, and overall health. Working closely with your surgeon and a specialist in bone health can help ensure the best possible outcome.
.
Symptoms of Spinal Osteoporosis
Spinal osteoporosis often develops without any noticeable symptoms in the early stages. However, specific symptoms may appear as the condition progresses and bones become more fragile.
Here are the common symptoms of spinal osteoporosis:
- Back Pain: This is often the first noticeable symptom and can range from mild to severe. It is usually caused by fractures or compression in the vertebrae. The pain may worsen when standing, walking, lifting, bending, or twisting.
- Loss of Height: Osteoporosis can cause compression fractures in the spine, leading to a noticeable loss of height over time.
- Stooped Posture: Also known as kyphosis or a dowager’s hump, this condition occurs due to multiple compression fractures, causing a forward curvature of the spine.
- Fractures: The vertebrae in the spine can become so weakened that they fracture easily, even from minor stresses or falls. These fractures can occur without significant trauma.
- Limited Mobility: Pain and fractures in the spine can lead to reduced mobility and difficulty performing daily activities.
If you suspect you have spinal osteoporosis or are experiencing any of these symptoms, it is essential to consult with your healthcare provider for proper diagnosis and treatment. Early detection and management can help prevent further bone loss and reduce the risk of fractures.

Treatments for Spinal Osteoporosis
Treating spinal osteoporosis focuses on strengthening bones, preventing fractures, and managing symptoms. Keep reading below for an overview of the treatment options:
- Medications: Several types of medications can help manage osteoporosis. Bisphosphonates, such as alendronate and risedronate, are commonly prescribed to slow bone loss and reduce fracture risk. Other medications include denosumab, which helps prevent bone breakdown, and teriparatide or abaloparatide, which can stimulate bone growth. Your doctor will determine the best medication based on your condition and overall health.
- Calcium and Vitamin D: Ensuring you get enough calcium and vitamin D is crucial for bone health. Calcium helps build and maintain strong bones, while vitamin D aids calcium absorption. Your doctor may recommend dietary changes or supplements to ensure you get enough nutrients.
- Exercise: Regular physical activity, especially weight-bearing exercises like walking, dancing, or resistance training, can help strengthen bones and improve balance, reducing the risk of falls and fractures. Your doctor or a physical therapist can help design a safe and effective exercise program tailored to your needs.
- Lifestyle Changes: Lifestyle changes can significantly impact bone health. Quitting smoking and reducing alcohol consumption can help improve bone density. Eating a balanced diet rich in calcium and vitamin D, including dairy products, leafy greens, and fortified foods, is also important.
- Fall Prevention: Since fractures often occur due to falls, taking steps to prevent falls is essential. This might include making your home safer by removing tripping hazards, using non-slip mats, installing grab bars in bathrooms, and ensuring good lighting throughout. Wearing supportive shoes and using assistive devices like canes or walkers if needed can also help.
- Pain Management: If you experience pain due to spinal fractures, pain management strategies can help. These might include over-the-counter pain relievers, prescription medications, physical therapy, and heat or cold therapy techniques.
- Monitoring and Follow-Up: Regular check-ups with your healthcare provider are important to monitor your bone health and adjust treatments as needed. Bone density tests may be done periodically to assess the effectiveness of your treatment plan.
By combining these treatments and working closely with your healthcare team, you can effectively manage spinal osteoporosis, reduce the risk of fractures, and maintain a healthy, active lifestyle. If you have any questions or concerns about your treatment plan, don’t hesitate to discuss them with your doctor.
Common Questions
How long does osteoporosis treatment take?
The treatment of spinal osteoporosis is an ongoing process rather than a condition with a definitive endpoint. The duration and intensity of treatment can vary based on several factors, including the severity of the osteoporosis, your overall health, and your response to treatment.
Concerning spine surgery, there is not a definitive answer. Your endocrinologist and spine surgeon will communicate to ensure that your treatment has progressed so that surgical complications are less likely and that the potential benefits of surgery outweigh the risks.
What are the risks of spine surgery for people with osteoporosis?
Spine surgery for people with osteoporosis involves several specific risks due to the weakened state of their bones. These risks need to be carefully considered by both the patient and the healthcare provider. Here are the primary risks:
- Increased Fracture Risk: Osteoporotic bones are more fragile, making them more susceptible to fractures during surgery. Even minor stress during the procedure can cause fractures in the vertebrae or surrounding bones.
- Hardware Complications: Weakened bones may not hold screws, rods, or other surgical hardware as securely as healthy bones would. This can lead to hardware loosening, migration, or failure, which may require additional surgeries to correct.
- Delayed Healing: Osteoporosis can slow down the bone healing process. This can prolong the recovery period and increase the risk of complications such as non-union (where the bones do not heal properly).
- Infection: As with any surgery, there is a risk of infection. However, the compromised healing ability in osteoporotic patients can make infections more difficult to treat and can prolong recovery.
- Increased Pain: Postoperative pain can be more intense or prolonged in patients with osteoporosis due to the fragility of their bones and the potential for additional microfractures or hardware issues.
- Loss of Correction: In spinal surgeries, maintaining the proper alignment and correction achieved during the procedure can be challenging in osteoporotic bones. Due to the fragility of the bones, the spine may lose the correction achieved over time.
- Adjacent Segment Disease: Surgery on one part of the spine can sometimes lead to accelerated degeneration of the adjacent spinal segments. This risk may be higher in osteoporotic patients due to their bone weakness.
- Complications from Anesthesia: Older patients or those with severe osteoporosis often have other health conditions that can increase the risk of complications from anesthesia.
- Neurological Complications: Although rare, nerve damage is a risk during spinal surgery. This risk may be slightly higher in osteoporotic patients due to the difficulty of stabilizing the spine.
Given these risks, a thorough preoperative assessment and careful surgical planning are essential. Surgeons may use specialized techniques and equipment designed for osteoporotic bones to mitigate some of these risks. Additionally, optimizing bone health before surgery through medications and supplements, as described above in the treatments section, can help improve outcomes.
You should discuss spine surgery in detail with your healthcare provider to understand the potential risks and benefits in the context of osteoporosis. This will help you make an informed decision that aligns with your overall health goals and quality of life considerations.
Resources
International Osteoporosis Foundation



