Awards & Recognitions – September 2024
HRSA Grant
Barrow Chair of Neurology and Senior Vice President Brad Racette, MD, FAAN, and his team at the Barrow Neuro Analytics Center have received a grant from the Health Resources and Services Administration (HRSA) to support expansion of the Center’s high performance compute research network. This award adds to the substantial investment already made by the state of Arizona. With this network, researchers in the Barrow Neuro Analytics Center leverage vast data resources to accelerate cures for neurologic disease.
AZBio Researcher of the Year
Nader Sanai, MD, chief of neurosurgical oncology and director of the Ivy Brain Tumor Center at Barrow, was named Arizona Bioscience Researcher of the Year by the Arizona Bioindustry Association. He formally received the award at the 20th Annual AZBio Awards. The award recognizes Dr. Sanai’s pioneering spirit and commitment to push beyond the status quo to discover new therapies for patients with brain tumors. He is pictured at the awards ceremony with Barrow Emeritus President and CEO Robert F. Spetzler, MD, and Arizona Bioindustry Association President and CEO Joan Koerber-Walker.
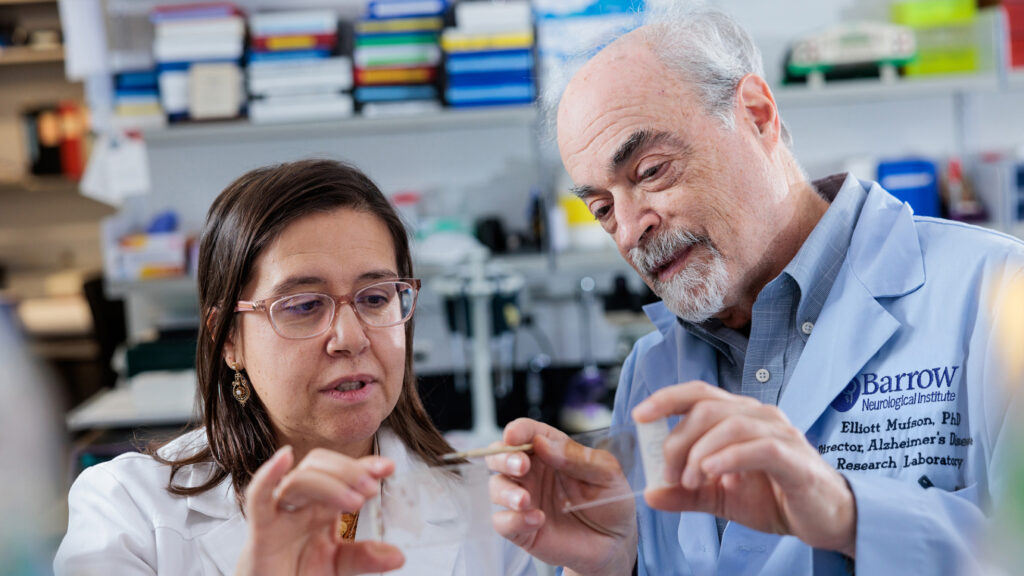
Arizona Alzheimer’s Consortium Grants
Elliott Mufson, PhD, a professor in the Department of Translational Neuroscience at Barrow, have received a grant to support his laboratory as they continue to investigate the effects of the SARS-CoV-2 (COVID-19) virus on brain function, particularly in individuals with Alzheimer’s disease and Down syndrome.
Although invasion into the brain by SARS-CoV-2 viral particles is still under debate, this virus is associated with significant and long-lasting neurologic symptoms in many patients. Additionally, people with Alzheimer’s disease and/or Down syndrome are more likely to die of COVID-19 than people without Alzheimer’s and/or Down syndrome.
Dr. Mufson and his team recently published a preliminary report in Acta Neuropathologica on this topic, thanks to funding from Barrow Neurological Foundation.
Marwan Sabbagh, MD, FAAN, a behavioral neurologist and the Vice Chair of Research in the Barrow Department of Neurology, and Anna D. Burke, MD, a neuropsychiatrist and the director of the Barrow Alzheimer’s and Memory Disorders Program, have received another year of funding for their Hispanic Enrollment in Alzheimer’s Research Trials (HEART) Program.
Hispanics with Alzheimer’s disease represent an underserved and understudied population in the United States. The Alzheimer’s and Memory Disorders Program launched the HEART Program to engage this community in clinical research efforts with the goal of understanding the unique factors affecting their cognitive health.
Specific efforts of the HEART Program include attending events and partnering with organizations dedicated to the Hispanic community, identifying and addressing barriers to research participation, developing culturally sensitive educational materials, offering memory screenings and other outreach events in Spanish, and supporting bilingual staff members.
Rita Sattler, PhD, MSc, a professor in the Department of Translational Neuroscience at Barrow, has received a grant to support her and her team as they continue to investigate the role of TDP-43 protein aggregates in neurodegenerative diseases including Alzheimer’s—an important step toward the development of new treatments.
The TDP-43 protein is normally found in the nucleus of most cells in the human body, where it plays a key role in the function and survival of the cells. However, this protein can somehow exit the nucleus and build up in the surrounding cytoplasm within the cell. This mislocation and accumulation of the protein was first associated with frontotemporal dementia (FTD) more than 15 years ago and has more recently been linked to Alzheimer’s disease and related dementias.
Two main questions still elude the scientific community: How does TDP-43 get transported outside of a cell’s nucleus? And, once in the cytoplasm, how does it contribute to the deterioration and death of nerve cells?
In an effort to answer these questions, the Sattler Laboratory analyzed postmortem autopsy brain tissue donated by individuals with Alzheimer’s disease and mild cognitive impairment. The researchers compared neurons affected by TDP-43 protein aggregates with neurons that were not affected, and they found significant differences in gene expression and mRNA processing events.
Using the funds from the Arizona Alzheimer’s Consortium, the lab is now using their “brain-in-a-dish” model to try to understand how these changes observed in Alzheimer’s differ from those identified in FTD, as published in a recent manuscript from the Sattler Lab (Gittings et al 2023, Acta Neuropathologica, PMID 37466726). A better understanding of these mechanisms is critically important for the development of biomarkers and therapeutics specific for Alzheimer’s.
Barrow neuroimaging scientist Ashley Stokes, PhD, is collaborating with Arizona State University neurodegeneration scientist Ramon Velazquez, PhD, to better understand how Alzheimer’s disease leads to changes in functional connectivity, the term for how different regions of the brain interact with each other.
Functional connectivity can be mapped with advanced imaging methods, such as functional magnetic resonance imaging (fMRI). Using such methods, numerous studies have shown impaired brain networks in Alzheimer’s disease. This association, however, is not well understood.
Drs. Stokes and Velazquez hope to advance our understanding of this relationship by applying a novel imaging modality in preclinical models that mimic what we already know about the stages of Alzheimer’s progression. This project will build upon the researchers’ previous findings of both gray matter atrophy and white matter microstructural changes in a preclinical model of Alzheimer’s, particularly in brain regions that play an important role in memory.
This project could provide much-needed context for numerous clinical studies that have shown widespread changes in the functional connectome in patients with Alzheimer’s, potentially bringing us closer to new therapies for the disease.
Yonas E. Geda, MD, MSc, a behavioral neurologist and neuropsychiatrist in the Alzheimer’s and Memory Disorders Program, has received a grant for a pilot project wherein patients with mild cognitive impairment (MCI) will undergo working memory training using the Cogmed technology developed at Karolinska University in Sweden.
To Dr. Geda’s knowledge, there has been little to no systematic investigation of the Cogmed intervention targeting working memory in MCI in the United States. There is substantial skepticism regarding various technologies that are being advertised for “brain training,” prompting the Association for Psychological Science (APS) to assemble more than 40 scientists to critically review existing brain-exercise programs. They identified three programs with some evidence of efficacy (Simons D, 2016), with Cogmed at the top of the list. The panel acknowledged that a person may improve on a specific cognitive task. However, the scientists did express reservations as to the potential transfer of the gain into other domains.
After Dr. Geda and his team made the web-based technology available to brain health clinic participants at Barrow, they observed promising results. From baseline to three months, nine participants demonstrated not only an improvement in working memory and executive function after but also a decrease in perceived stress. Dr. Geda hypothesized that the Cogmed intervention might have led to a transfer from a cognitive domain to a neurobehavioral construct of stress.
These early findings led the team to apply for grant funding from the Arizona Alzheimer’s Consortium to gather additional preliminary data, which could pave the way for future clinical trials of the Cogmed intervention in the U.S.

David Medina, PhD, an assistant professor in Dr. Robert Bowser’s laboratory within the Department of Translational Neuroscience at Barrow, has received a grant for a project he is leading that aims to understand how the Matrin 3 protein, which is found in the nucleus of cells, is involved in different neurodegenerative diseases.
This project builds on previous work performed in the Bowser Laboratory, which associated Matrin 3 dysfunction and accumulation with familial ALS. The team also recently discovered that Matrin 3 pathology is a semifrequent occurrence in other neurodegenerative diseases, including Alzheimer’s disease.
Dr. Medina and his team will focus on three overarching questions: How is Matrin 3 dysfunction/pathology caused, what are its consequences, and can those consequences be reversed? A better understanding of Matrin 3’s role in neurodegenerative diseases could reveal new potential targets for therapeutic development.
Brain Aneurysm Foundation Grant
Takuma Maeda, MD, PhD, a postdoctoral research fellow in the Barrow Aneurysm and AVM Research Center, has been awarded the 2024 Austen L. Dunn Chair of Research grant from the Brain Aneurysm Foundation. The $40,000 prize will support his project titled: “The Effect of Novel Brain Penetrant Manganese Porphyrin-Based SOD Mimic on the Long-Term Outcomes of Subarachnoid Hemorrhage.” This project is a step toward Dr. Maeda’s long-term goal of developing pharmacological interventions to prevent the rupture of brain aneurysms and improve outcomes for patients with subarachnoid hemorrhage. He is pictured with Brain Aneurysm Foundation Executive Director Christopher S. Ogilvy, MD, (left) and National Institute of Neurological Disorders and Stroke (NINDS) Director Walter J. Koroshetz, MD.
Newsweek World’s Best Specialized Hospitals
Newsweek has released its 2025 list of the World’s Best Specialized Hospitals for Neurosurgery, naming Barrow Neurological Institute as No. 14. Since launching this global ranking for neurosurgery in 2022, the media company has consistently recognized Barrow as a top-tier hospital. The Institute, based in Phoenix, Arizona, has held the No. 10 spot nationally for three consecutive years and the No. 1 spot in the Southwestern United States for all four years. The list highlights 125 hospitals total.
Department of Defense Grant
Chia-Ling Phuah, MD, MMSc, a neurocritical care physician-scientist and co-director of the Barrow Neuro Analytics Center, has received a grant from the United States Department of Defense (DoD). The Fiscal Year 2023 Peer-Reviewed Alzheimer’s Research Program Transforming Diagnosis Award will provide Dr. Phuah and her team with $2.5 million to study the intersection of traumatic brain injury (TBI) and Alzheimer’s disease. The researchers will examine whether having a genetic risk of Alzheimer’s disease can help predict an individual’s cognitive outcome if they experience a TBI. They also aim to identify factors that may protect TBI patients from changes to their thinking abilities.
‘Neuron’ Cover
Cell Press selected an illustration created by Hannah Koffman and Dani VanBrabant of the Barrow Neuroscience Publications team for the cover of a recent issue of its journal “Neuron.”
Inspired by the vision of Barrow Neurocritical Care Program Director Ruchira Jha, MD, MSc, the cover depicts a forest of brain cells amid a lightning storm. The focus is on the heterogeneity of cells within the forest, including types of immune and other brain cells measured in a study led by Dr. Jha, which was published in this issue.
The trail going through the image serves as both a metaphor for the identification of final molecular pathways and a tribute to the first-of-its-kind atlas created in the study. The vast, interactive atlas includes 334,376 cells and information about how they responded to traumatic brain injury, which could eventually help doctors use precision medicine to target treatments for TBI.
The trail leads to a lightning strike, which is an ode to TBI. The different emissive colors on the trees and shrubs in the “forest” light up brighter the closer they are to the TBI lightning strike. These emissive colors are taken from the UMAP created in the study and are shown as a reference to the biomarkers and therapeutic targets found in the study for future successful translation of therapies in the field.
SMoCA Exhibit

“Beauty is in the brain of the beholder,” announced Scottsdale mayor David Ortega at the fall opening of Brains + Beauty, a first-of-its-kind exhibition at the Scottsdale Museum of Contemporary Art (SMoCA) where illustrations from Barrow Neuroscience Publications will be displayed through Jan. 19.
The exhibit investigates neuroaesthetics, a cognitive neuroscience that studies the biological mechanisms behind aesthetic experiences. The illustrations from Barrow are based on the “aesthetic triad,” which comprises the brain’s sensory-motor, knowledge-meaning, and emotion-valuation systems.
Contributors (from left):
- Benjamin Dveirin – Content Producer, Barrow Neurological Foundation
- Hannah Koffman – Medical Animator/Illustrator, Barrow Neuropub
- Michael Hickman – Senior Technical Artist, Barrow Neuropub
- Dani VanBrabant – Senior Medical Modeler/Animator, Barrow Neuropub
- Ann Q. Mai – Medical Animator/Illustrator, Barrow Neuropub
- Kristen Larson Keil – Manager, Barrow Neuropub
Special thanks to curator Laura Ramon Hales of Scottsdale Arts for including Barrow in this exhibition.