Arizona Father Overcomes Oropharyngeal Cancer at Barrow
John Burroughs shares how the head and neck cancer experts at Barrow, alongside his faith and his love for family, helped him battle—and defeat—throat cancer.
John Burroughs opened the refrigerator in the garage of his home in Chandler, Arizona and began guzzling protein drinks, despite his complete lack of appetite. He screamed as he drank them—the pain was both physical and emotional. He powered through several bottles, dedicating each one to a member of his family: his wife, his two sons, his now-daughters-in-law, and even his sons’ pets.
John then went to have his blood work redone, hoping his white blood cell count would budge just enough so that he could complete his third and final chemotherapy infusion. He was determined to stay on track so that he could spend Thanksgiving in South Carolina with his kids.
The now-63-year-old father still becomes teary-eyed at the memory. “That trip was kind of my—”
“Carrot,” said his wife of almost 32 years, Elizabeth, finishing his sentence.
As John underwent treatment for oropharyngeal cancer in the Head and Neck Cancer Program at Barrow Neurological Institute in Phoenix, he kept his sights on that family vacation—arriving punctually for every appointment and marking off his progress on a calendar.
Sounding the Alarm
It all started with a scratchy throat in July 2022. John suspected he’d picked up a virus, maybe COVID-19, or that he had some irritation from inhaling wildfire smoke. He and Elizabeth had been staying at their cabin in Idaho, near where John grew up. The scratchy throat subsided, and John didn’t think much more of it—until it returned two weeks later. Elizabeth, a longtime operating room nurse at Barrow, noticed swelling of the right lymph node in John’s neck.
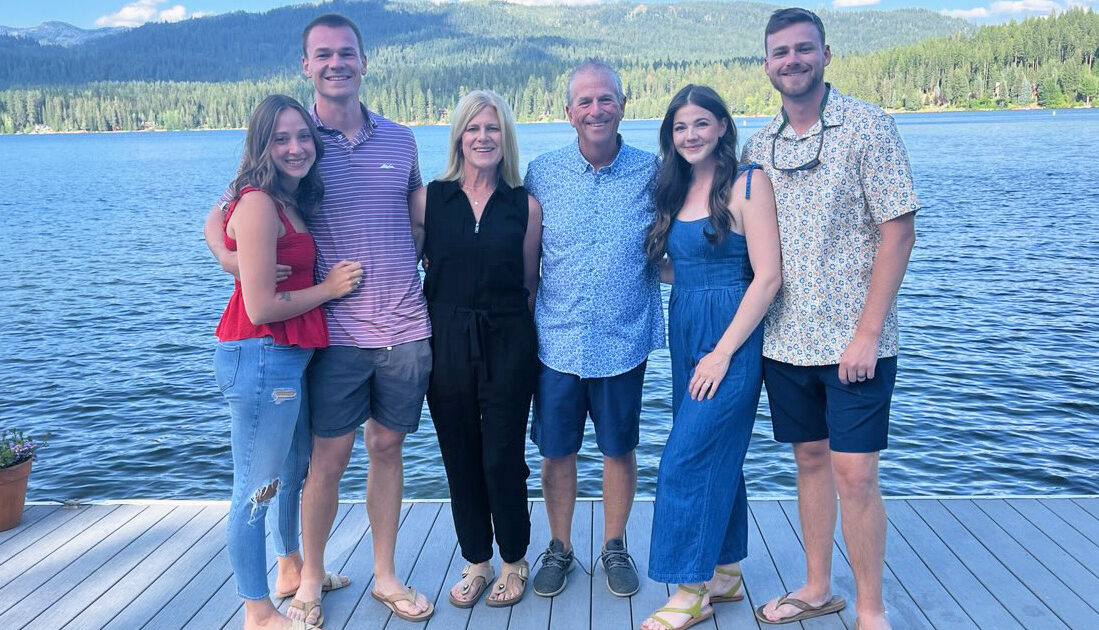
Wanting to ensure he was healthy for his son’s August wedding, John returned to Arizona to see his primary care physician. The doctor ordered a computed tomography (CT) scan and referred John to an ear, nose, and throat (ENT) specialist.
While the CT image did show an enlarged lymph node in John’s neck, the doctor seemed more concerned with an incidental finding: a prickly looking mass on John’s lung. Oftentimes, cancerous tumors can have this “spiculated” appearance.
John and Elizabeth agreed to keep the news quiet until after the wedding, both because the diagnosis wasn’t certain and because they didn’t want to overshadow their son and future daughter-in-law’s big day.
Fuel for the Fight Ahead
Within a few days of returning from the out-of-town wedding, John visited the Department of ENT and Skull Base Surgery at Barrow. He met with otolaryngologist Griffin Santarelli, MD, who examined John’s throat with a tiny camera called an endoscope. The ENT specialist then ordered a biopsy and additional imaging scans.
When John received the diagnosis of oropharyngeal cancer, which affects the middle part of the throat, he felt shocked, overwhelmed, and afraid. But Dr. Santarelli delivered some promising news: If they began treatment as soon as possible, John had about an 85 to 90 percent chance of beating his cancer.
“I thought, man, I’ve had it too good and am way too blessed to, at the first curveball, at the first big bump in the road, say: Why me?” John recalled. “My faith, life’s blessings, and everything I had to fight for pushed me very quickly to: Let’s get on with the treatment and trying to get better.”
But John and Elizabeth still had to share the diagnosis with their sons, ages 25 and 27 at the time, and their sons’ significant others. John describes breaking the news to them over FaceTime as the most challenging part of his entire oropharyngeal cancer journey.
“We did our best to balance the notion that it was serious with what the doctors said about how treatable, how curable, this was,” John remembered. “They both reacted a little differently, but I’ll forever remember their reactions. In a strange kind of way, that moment served as a big catalyst for me to keep fighting. I knew I had to.”
The Dream Team Trifecta
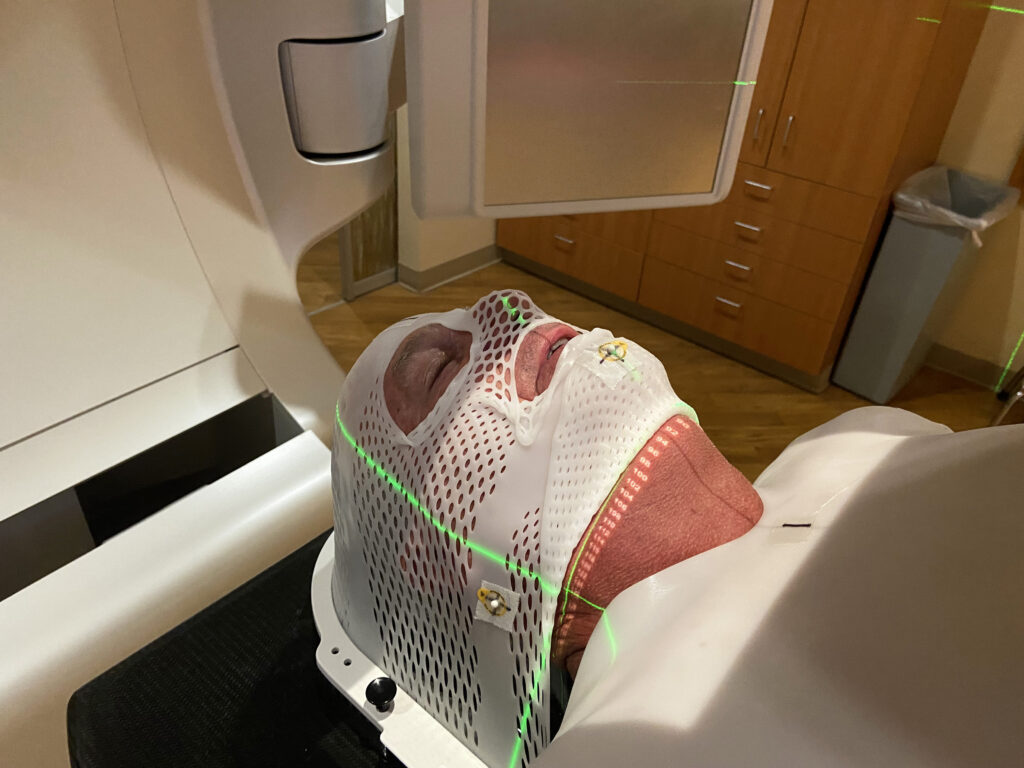
John’s treatment plan consisted of a seven-week course of radiation therapy, five times per week, combined with three total chemotherapy infusions spaced out between the beginning, middle, and end of that timeframe. His medical team did not recommend surgery for his case; considering the specifics of his tumor—namely, its size and location—they felt the benefits did not outweigh the risks.
At the Head and Neck Cancer Program at Barrow, patients like John have access to various specialists who closely collaborate on each case. John benefitted not only from the expertise of Dr. Santarelli, but also medical oncologist Robert Yoo, MD, and radiation oncologist William Kennedy, MD.
“The three modalities—between ENT, medical oncology, and radiation oncology—it is a well-oiled machine,” Elizabeth said. “It’s so impressive how these three doctors communicate.”
John agreed wholeheartedly. “The interactions between the three teams, their personalities, and the folks that are on their teams was nothing short of phenomenal,” he added.
John took doses of humor wherever he could find them, and he laughed as he remembered a time when Dr. Kennedy referred to Dr. Yoo as “Rob.” “Who are you talking about? I don’t have a doctor named ‘Rob,’” John thought. “I can remember leaving that day thinking, man, these guys are tight.”
This emphasis on teamwork is one of the reasons Dr. Kennedy feels proud to be part of Barrow. “It’s not one physician,” he said. “It’s really dozens of people working together for patients.”
Blood, Sweat, and Fear of Needles
After undergoing a fitting for his customized thermoplastic mask, which would keep his head still during radiation therapy, John arrived for his first day of both radiation and intravenous (IV) chemotherapy.
“He’s not good with needles,” Elizabeth said.
“That’s probably an understatement,” added John, explaining that he fainted when they tried to start his IV for the infusion.
Elizabeth briefly wondered if her husband was pulling a prank, explaining that it wouldn’t be out of character for him. But then she saw that his heart rate had dropped, and he was beginning to sweat profusely. Elizabeth found some levity in the irony: Her husband fears needles while she thrives in the operating room.
It marked the first of several times that John experienced vasovagal syncope following a needle stick, which he also had to endure for hydration therapies and blood draws. The fainting episodes would put John behind schedule, sending him into a spiral of worry. Between the retired businessman’s organized personality and his determination to travel to South Carolina, he had to stay on track. Chemotherapy also brought another challenge for John mentally: accepting that the treatment was both “the cure and the poison,” he said.
The radiation therapy sessions, which took less than 10 minutes each, were less eventful. While the restrictive thermoplastic mask can trigger claustrophobia for some patients, it didn’t bother John. He curated a playlist of his favorite songs to listen to during his treatments, and he enjoyed seeing familiar faces—both patients and staff—at each visit. “It truly felt like Dr. Kennedy’s radiation team were my friends, as I was seeing them every day,” he said.
Support from Family, Friends, and… Fifth-Graders?
As expected, though, side effects emerged during the middle of John’s treatment. He developed a metallic taste, sore throat, double earache, fatigue, and nausea. “The medical teams were helpful and very caring in attempting to make the side effects tolerable,” he said.
Still, John mustered every bit of his mental and physical strength and leaned on his faith to push through those three weeks. Because of the side effects, he struggled to eat—no matter how hard he tried—and began losing weight. Elizabeth also tried everything, from accommodating his fleeting cravings to outright begging him to eat, hoping to keep him from needing a feeding tube.
“There was one day where our neighbor, his best friend, was trying to get him to eat,” Elizabeth recalled. “He was over at our house hanging out with John for the day, and he said, ‘He had two bites of white rice today, and that was it.’ And that night, I stayed up all night, just watching him, like, keep breathing, keep breathing.”
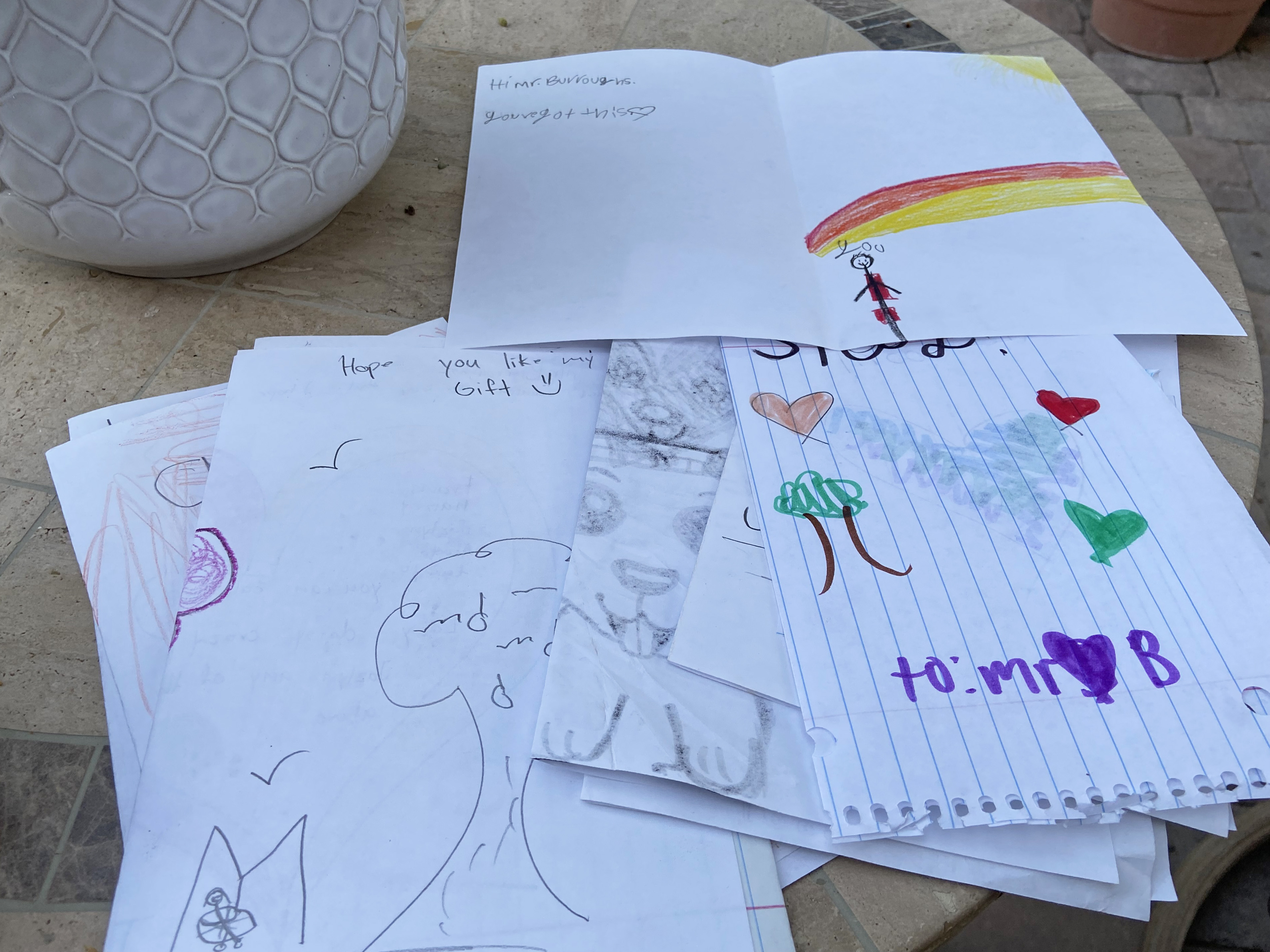
In addition to support from his family, friends, church community, and medical team, John gained a morale boost from an unexpected group: a class of fifth-grade students from an inner-city school in Oklahoma City, where his son’s future wife worked as a teacher.
John opened up a Manila envelope addressed to him and dumped out a pile of cards, feeling like he was back in elementary school on Valentine’s Day. As he read through the uplifting messages from the students, he came across a card secured with layers of tape. Inside, he found a $1 bill and the words: “Sorry, Mr. John, this is all I have, but hopefully it helps pay for your treatment.”
During his final two weeks of treatment, John began to turn a corner, but he wished for some kind of “progress report” on whether it was working. He wouldn’t know until he had his next PET scan 60 days after his final treatment.
Heaven on Earth
On Nov. 14, 2022, John rang the ceremonial completion bell in the Department of Radiation Oncology alongside his treatment team, his wife, and several friends. His sons joined virtually through a video conference coordinated by Elizabeth. And when John took a moment to thank the Oklahoma City students for their words of encouragement, Elizabeth turned her laptop around to reveal a surprise: The class had also joined the video call to celebrate with him.
John received the green light to take his highly anticipated trip to South Carolina. Although things weren’t totally “normal”—John hadn’t fully regained his appetite and had to be cautious about germs due to his weakened immune system—he found joy in simply being there.
He gladly watched the dogs while his family attended a Clemson University football game, which would have been too much for him, and he was grateful to participate in the Thanksgiving meal of which he ate very little. Aside from the football game, the family mostly hunkered down around the house, walking the dogs, putting together puzzles, and just existing together.
“It was heavenly,” Elizabeth said. “It was one of the best trips because we were just so grateful to all be together.”
Getting the ‘All-Clear’
Finally, after the tormenting two-month wait, John received the good news: The treatment had worked. He no longer had oropharyngeal cancer, and the mass on his lungs was benign.
“It’s probably not coincidental that the first scan that showed clear of cancer, there was a huge emotional and mental lift,” John said. “It didn’t mean that I had every bit of energy back, but it gave me motivation.”
Within six months, John was able to bike 20 miles a day. A few months after that, he noticed a resolution of his neuropathy, a common side effect of cancer treatment.
“I am so pleased that our comprehensive head and neck oncology team at Barrow was able to help John identify and overcome his cancer,” Dr. Santarelli said. “A head and neck cancer diagnosis is life-changing, and the treatment journey can be incredibly difficult for both patients and their loved ones. Being able to support John through this fight so that he could get back to enjoying life with his family is why I find my work so fulfilling.”
The Barrow Difference
Whenever Dr. Santarelli asks John if there’s anything he can’t do post-treatment, John can’t think of a single thing. That person-centered approach to care is one of the many things John and Elizabeth appreciated about the Head and Neck Cancer Program at Barrow. “All of the doctors engaged me about things I liked, whether it was golf or hiking or travel,” he said. “They were all very personable in that way.”
He remembered having a long conversation with Dr. Kennedy about faith, a value John described as integral to his cancer fight.
“Receiving a diagnosis of head and neck cancer is often a very vulnerable time for patients and their families,” Dr. Kennedy said. “Alongside the emotional toll it can have, the treatments can be very difficult as well, even with state-of-the-art technology and expertise. My goal is for me and my team to make this journey a little less scary, doing our best to try and help patients along the way.”
John also found comfort in knowing he was in highly skilled hands. “I had a great deal of confidence that I was getting the best treatment possible,” he said. “If I was going to be cured anywhere, it was going to be here.”
In addition to imaging tests, John’s team used a cutting-edge monitoring technology known as circulating tumor DNA to assess John’s response to treatment. This tool allows for the detection of tumor-specific genetic material in a patient’s bloodstream.
“John’s perseverance and the utilization of this advanced monitoring technique resulted in a successful outcome, as he achieved remission,” said Dr. Yoo, who described John’s resilience, strength, and courage as awe-inspiring. “His story serves as a testament to the power of human spirit and the significant advancements in medical technology that contribute to the fight against cancer.”
It’s the possibility of achieving outcomes like John’s that drives the Head and Neck Cancer Program team at Barrow.
“From diagnosis to treatment to surveillance, being part of John’s journey with his family has been an incredible experience, as he is currently cancer free,” Dr. Santarelli said. “This is the standard and goal for all of our patients at Barrow.”
Contemplating Cancer’s Far-Reaching Effects
John’s gravelly voice and scratchy throat serve as physical reminders of his cancer battle, along with a thick, three-ring binder of still-accumulating medical documents—decorated with family photos on the cover and a map of the Barrow campus on the back.
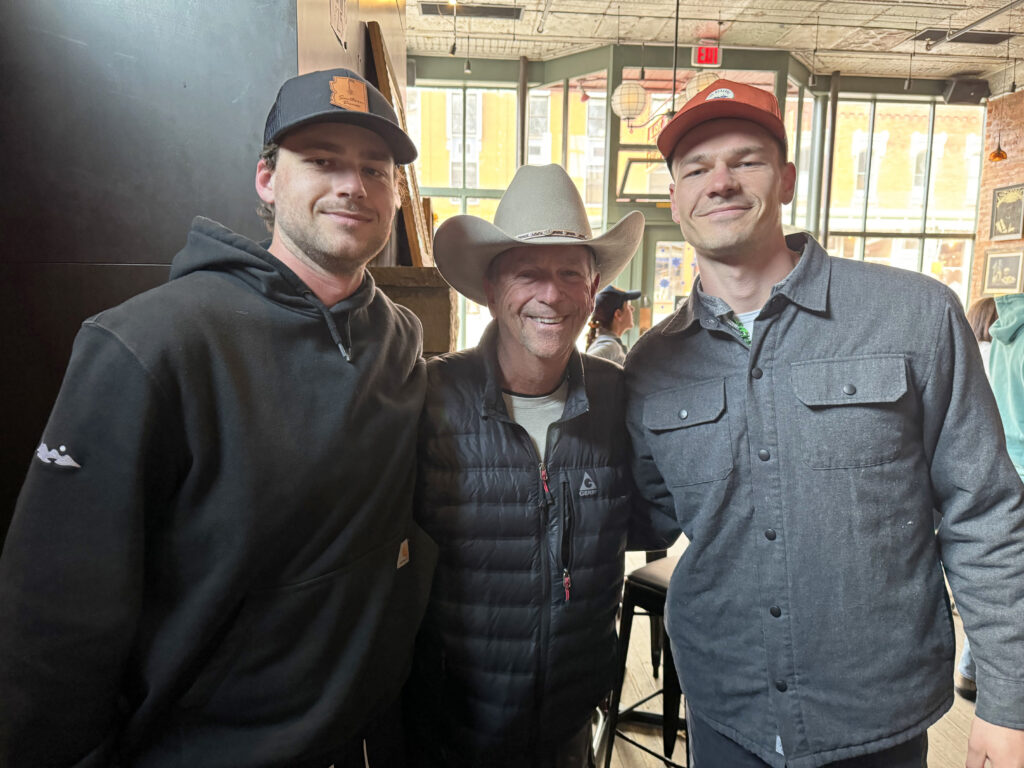
John also still holds onto the cards from the students in Oklahoma City. “Every once in a while, I pull one of those out and look at it. Some of them were hilarious—and motivating,” John said. He even paid a visit to the class in person following his clean bill of health. After asking him how he was doing, the students shifted to other burning questions, such as, “How hot is it really in Arizona?” and “How is your son so tall?”

In addition to the tangible reminders of the journey, John and Elizabeth carry a mix of memories: some painful and terrifying, others moving and heartwarming, and even a few that are humorous. He hasn’t forgotten about the patient who chose to discontinue treatment on the same day John celebrated the completion of his own. And Elizabeth can still picture the young boy in the waiting room who reminded her of her sons. She remembers praying that he wasn’t a patient himself and then feeling heartbroken when the medical team took him back for treatment.
“It can be an example of how you never know what’s going on in somebody’s life, so cut them some slack,” she said.
They also haven’t forgotten the support they received, from loved ones filling their fridge with food and shuttling John to appointments, to simply checking in and lending a listening ear. Elizabeth said accepting help was difficult for her at first, noting her independent nature, but surrendering to that support is now a piece of advice she passes along to others who might be navigating a similar challenge. “Let people help you,” she said. “People want to help.”
“I had a great deal of confidence that I was getting the best treatment possible. If I was going to be cured anywhere, it was going to be here.”
-John Burroughs, Barrow Patient
John’s advice? Lean on your faith, trust your body, trust your loved ones, stay on top of your preventative screenings, and—if you do wind up in a battle with cancer—find the perspective that helps you persevere. For John, that was counting his blessings and remembering what he was fighting for.
“Dr. Santarelli’s words were spot-on,” John remembered. “‘You’re going to be cured, but you won’t be the same.’”