
Barrow Patient Benefits From Rapid, Coordinated Stroke Care
Babbi Longo isn’t much of a morning person, so she tends to start her work day with a caffeinated drink. On Friday, March 31, she poured herself a glass of iced tea, expecting a routine start to her shift.
“I love Southern sweet tea. If you can see through it, it’s not strong enough,” said Babbi. She was raised in Arizona but grew up on Southern fare, thanks to her grandparents’ roots in Texas and Arkansas.
If it hadn’t been for Barrow Neurological Institute, I probably wouldn’t be sitting here doing this good right now.
Babbi Longo, Barrow Patient
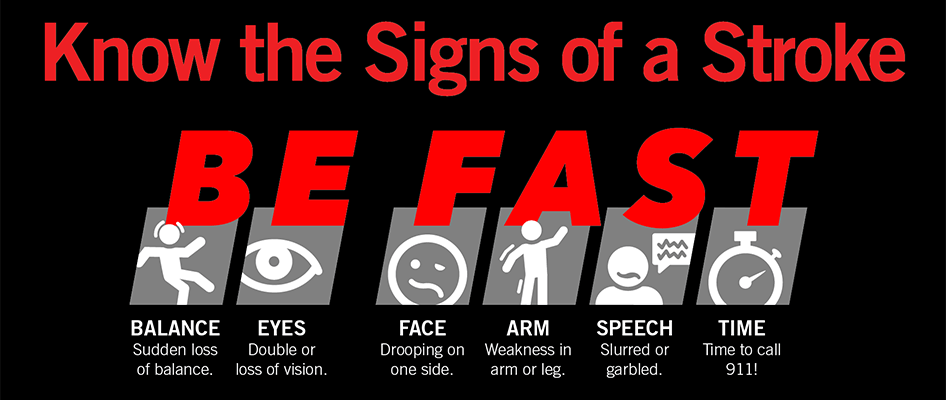
She sat down at her desk in the Phoenix home she shares with her adult son, ready for her remote job as a team lead at a call center. At 63 years old, Babbi has been assisting some of her clients for more than 30 years. She didn’t think much of it when she tried to sip her tea and spilled on herself. Then, she knocked an item off her desk—possibly her computer mouse, though she doesn’t remember for sure. She recalls leaning over to retrieve the item, struggling to sit back up, and hearing her son tell a 911 dispatcher that his mother might be having a stroke. It turns out Babbi was displaying several telltale symptoms, including facial drooping, arm weakness, and slurred speech.
Her memory from that morning is hazy and fragmented, but she is certain of one thing: “If it hadn’t been for Barrow Neurological Institute, I probably wouldn’t be sitting here doing this good right now,” she said during a visit to the Institute just a few months later.
Busting Clots Curbside with the Mobile Stroke Unit
Since Babbi’s home was within the 20-minute response radius of the Barrow Emergency Stroke Treatment Unit, the Phoenix Fire Department dispatched the Institute’s unit along with one of its ambulances.
A stroke-dedicated emergency room on wheels, the 11-ton unit is equipped with a computed tomography (CT) scanner and stocked with clot-busting medication. Barrow staffs the unit with a CT technologist and stroke-certified nurses, who consult with an on-call vascular neurologist from the Institute’s Petznick Stroke Center via telemedicine. When the Barrow Emergency Stroke Treatment Unit hit the roads in 2017 in partnership with Phoenix Fire, it became the first of its kind in Arizona and only the 10th in the United States.
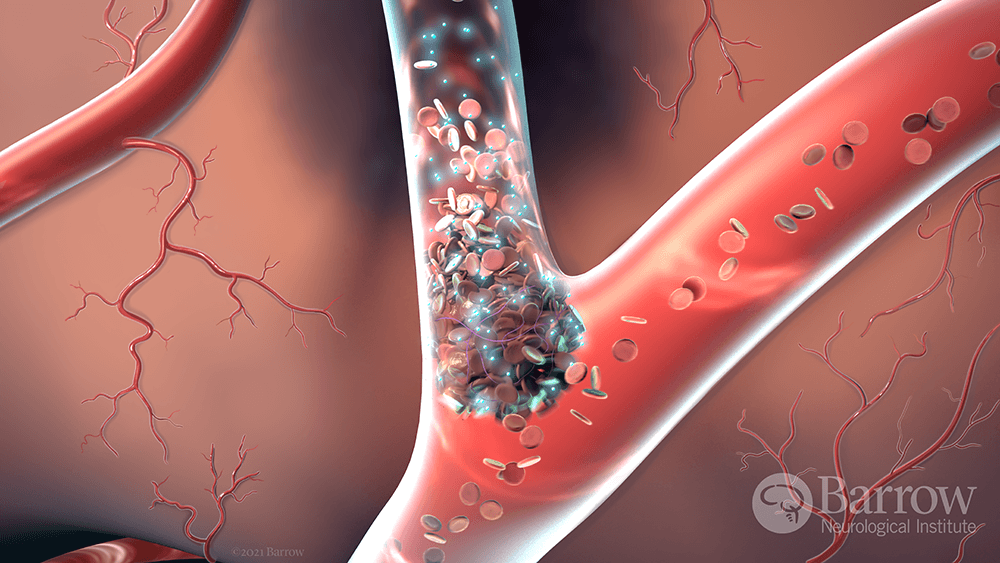
The CT images taken aboard the unit showed Babbi was experiencing an ischemic stroke, meaning her stroke was caused by a blockage rather than a bleed. The mobile stroke team rapidly administered tenecteplase (TNK), a new clot-busting drug derived from tissue plasminogen activator (tPA). Phoenix Fire personnel transported Babbi by ambulance to Barrow, where she received a prompt evaluation by the vascular neurology team and was identified as a candidate for endovascular neurosurgery. This minimally invasive subspecialty of neurosurgery involves the use of catheters and imaging to treat blood vessel problems without the need for open surgery.
These interventions happened seamlessly and within a truncated timeline thanks to the experienced multidisciplinary team at the Petznick Stroke Center. The Center cares for more individuals with stroke than any other in the southwestern U.S. Additionally, it has met the rigorous standards for Comprehensive Stroke Center certification by The Joint Commission in partnership with the American Heart Association and American Stroke Association.

A Life-Saving Procedure
Endovascular neurosurgeon Andrew Ducruet, MD, said Babbi arrived with profound symptoms caused by the blockage in her middle cerebral artery—the largest branch of the internal carotid artery, thus a critical supplier of oxygen and nutrients to the brain.
Dr. Ducruet and his team performed a thrombectomy, which involved inserting a catheter into Babbi’s radial artery in her wrist and navigating the flexible tube through her network of blood vessels to the site of the clot. Within 15 minutes of accessing the radial artery, Dr. Ducruet successfully removed the clot through the catheter using specialized instruments and restored blood flow.
“She improved dramatically while still on the table, and her NIH stroke scale was measured at zero within 30 minutes of the procedure,” Dr. Ducruet said, referencing a widely used method for assessing acute strokes. Scores in this scale range from zero to 42. “This case highlights the tremendous efficacy of a thrombectomy procedure, as well as our team’s ability to provide this therapy for patients with stroke.”
During a Stroke, ‘Time is Brain’
Babbi awoke from the anesthesia and looked into the masked face of a medical professional. “When’s lunch?” she asked, having missed breakfast.
She remembers the wide-eyed expressions of the hospital staff surrounding her bed in the Neuro-Intensive Care Unit. As she continued to speak, they seemed amazed at her level of awareness and function. Babbi tearfully reunited with her son, whom she calls her hero. He wasn’t supposed to be home that day, Babbi said, but he had a last-minute change of plans. She then spent the next two nights in the hospital waiting for her blood pressure to stabilize. “I was in and out like boom,” Babbi said. “I can’t think of many other places that would take care of business that quick.”
When it comes to stroke treatment, experts often say “time is brain.” Research suggests that every hour a stroke goes untreated, the brain loses 120 million neurons—equivalent to the number lost in 3.6 years of normal brain aging. Stroke is the No. 5 cause of death and a leading cause of disability in the U.S.
Recovering and Refocusing
Soon after her discharge from the hospital, Babbi learned she has atrial fibrillation. Also known as A-fib, the condition causes an irregular heart rhythm and can lead to blood clots. She now takes a blood thinner to reduce her risk of another ischemic stroke.
Babbi underwent physical therapy at home for about a month, learning how to use a walker for bouts of dizziness and practicing exercises to strengthen her dominant hand.
“I can do everything I did before,” she said. “It was like taking a cork out of a bottle; everything went back to normal, except for the fact that now I’m not so razor sharp.”
Multitasking doesn’t come as easily for Babbi as it did before her stroke, nor do words. She describes feeling at times like a word is on the tip of her tongue, but she can’t quite find it. She also experiences blood-pressure spikes when she gets overwhelmed.
Scaling back at work is unfamiliar to Babbi. After a cervical cancer diagnosis in 2001, she continued to work throughout her treatment. In the midst of her stroke, she was adamant that she return to her desk to complete her shift. She describes herself as “laser-focused” and dedicated to helping her clients, even when it has meant working late or skipping breaks.
“My boss would always say, ‘You’re going to die at your desk,’” Babbi recalled, confessing that in addition to working long hours, she often prioritized convenience over nutrition with her meals. “I always thought it would be a heart attack.”
Babbi is now trying to apply her customer-care mindset to her own self-care. In addition to taking blood-thinning medication, she’s now more mindful about her diet and stress levels. She finds comfort in her faith and leans on her family for support, including her son, sister, and cat Ozzy.
Babbi’s son was relieved to see his mother acting like her usual self when the two of them were watching an old Superman cartoon and she recounted what was about to happen between the hero and his nemesis Brainiac.
“My son said, ‘OK, Mom, you’re getting better; you’re being your nerdy self again,” she recalled.
Sharing Her Story
When asked why she finds it important to share her story, Babbi answers the question by telling a different story—one about a neighbor of many years. Every morning, the neighbor went outside to check her mail and let her dog play in the front yard.
“One day she didn’t come out, and the porch light was still on from the morning,” Babbi remembered. The neighbor was found inside her home, needing medical attention. She made it to the hospital but died shortly after. Her diagnosis? A stroke.
Babbi has thought about that neighbor a lot since the end of March. She feels fortunate that her son was not only home, but that he promptly recognized the signs of a stroke. She now takes every opportunity to raise awareness about stroke and its symptoms. She’s also grateful she had access to Barrow for her treatment. In addition to the stroke team’s efficiency, Babbi praised their compassion. She explained that they made her feel safe, comfortable, and supported.
“I can’t give enough thanks for how fast and how professional and caring they were,” Babbi said of the Barrow staff. “Everybody—the doctors, the nurses, the referral department—it feels like they care.”
Minding What Matters Most
The Petznick Stroke Center can make the difference between an outcome like Babbi’s and one like her neighbor’s. Ms. Longo’s care exemplifies the stroke system of care that Barrow has spent years developing, implementing, and refining.
This system begins with outreach and education so that the community can spot the signs of a stroke and call for help, like Babbi’s son did. At its core is rapid, coordinated, and expert evaluation and treatment with access to advanced care when needed—no matter the time of day. This was demonstrated in every step of Babbi’s acute care, from boarding the mobile stroke unit to waking up in the Neuro-Intensive Care Unit with disease specialist nurses at her bedside. And the Petznick Stroke Center’s continuum of care doesn’t end at discharge. Next steps may include neuro-rehabilitation or, as in Babbi’s case, outpatient follow-up with the vascular neurology team. That follow-up care is what led to her diagnosis of A-fib and a treatment plan to reduce her risk of future strokes.

