Patient With Spinal Hemangioma Has Life-Altering Treatment at Barrow
“Be strong and fight.”
Andy Scholl heard those four words from his father before going into surgery, and they became his mantra throughout recovery.
The 37-year-old was active all his life. He played baseball at the University of Kansas and then taught the sport overseas before returning to his hometown in the Southwest to pursue a different career path. But even after he traded his career in baseball for one outside of athletics, Scholl kept moving with activities like running, biking, and hiking.
“I never dreamt of any health issue, especially not in my later 30s,” he said.
In November, Scholl noticed his legs feeling heavier on his runs. Over the next couple of months, he developed burning and pin-pricking sensations in his legs and eventually his abdomen and chest.
In mid-January, Scholl consulted with a friend who works as a physical therapist. At his friend’s recommendation, Scholl made an appointment with his primary care physician. He had X-rays taken, but the images offered no explanation for his symptoms.
‘At Some Point, It Would Paralyze Me’
An orthopedic surgeon ordered a lumbar MRI to look at Scholl’s lower back, but the test came back normal. The surgeon then ordered a thoracic MRI to evaluate Scholl’s mid-back, explaining that it would likely rule out anything spine related and Scholl would need to see a neurologist next.
Instead, the MRI revealed a spinal hemangioma—a tumor made up of abnormal blood vessels. The tumor had developed in his seventh thoracic vertebra, a bone of the spine commonly referred to as T7, and was putting pressure on his spinal cord.
Scholl spoke to a local neurosurgeon who had trained at Barrow Neurological Institute in Phoenix. The surgeon recommended Scholl see the Institute’s chief of spine surgery, Dr. Juan Uribe—a renowned minimally invasive spine surgeon who is experienced in thoracic spine surgery.
The thoracic spine is the most difficult region of the spine to access, which increases the risk of complications. Dr. Uribe has developed a minimally invasive approach to reduce that risk, but Scholl’s surgery was too complex to be performed through a small incision.
“The complexity of Andy’s surgery had significant risks, including worsening his ability to walk and even bleeding to death,” Dr. Uribe said.
But monitoring the hemangioma over time was not an option either.
“Dr. Uribe was very clear; at some point, it would paralyze me,” Scholl said.
Many spinal hemangiomas never produce symptoms at all. When they do, they typically fracture the vertebra, Dr. Uribe said. In these cases, a surgeon may treat the fracture by injecting a special cement into the bone in a procedure known as vertebroplasty.
Because Scholl’s hemangioma presented with spinal cord compression rather than a fractured bone, a traditional vertebroplasty would not have helped.
Spinal Hemangioma Surgery: Success Through Teamwork
Scholl submitted his imaging to Barrow and, after a telemedicine consultation, was promptly scheduled for surgery. He traveled to Phoenix with his wife, Cara.
“Everybody I spoke with in the field said, ‘You’re going to the best of the best,’” Scholl recalled. “That was really comforting.”

Spinal Neurosurgeon
On June 11, Scholl underwent the first of two procedures: endovascular embolization to reduce the risk of significant blood loss during the removal of the tumor. This procedure involves guiding a thin, flexible tube called a catheter through the network of blood vessels in the body to the site of the lesion and then inserting materials to seal it off from blood flow.
“I was delighted by the opportunity to participate in Andy’s care,” said endovascular neurosurgeon Dr. Felipe Albuquerque. “I was not only impressed by Andy’s courage but by his kind demeanor and trust in Barrow. These things are so important to us as caregivers and remind us of the honor bestowed upon us when we take care of patients like Andy.”
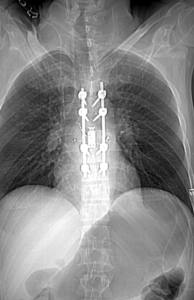
The following day, Scholl underwent a seven-hour surgery with Dr. Uribe to remove the tumor and stabilize his spine. Dr. Uribe removed part of the T7 vertebra, from which the tumor had grown, and inserted a bone graft and cage to fuse the adjacent vertebrae together. To further stabilize the spine and support bone fusion, Dr. Uribe placed two titanium rods from T5 to T9 and anchored them with eight screws.

Endovascular Neurosurgeon
“It was a fine line between eliminating compression of the neural elements and not destabilizing the spine too much, because we wanted to bring it back as stable as possible,” Dr. Uribe said.
Scholl began walking around the intensive-care unit the next day and left the hospital a few days after that, without needing any neuro-rehabilitation. “Surgery was successful because at Barrow we treat with a multidisciplinary approach,” Dr. Uribe said. “The successful embolization helped to make this surgery more feasible in terms of decreasing the amount of bleeding. Without it, it probably would have been impossible to do the surgery.”
The Other Side of Surgery
Scholl expressed immense gratitude for everyone involved in his care, from the office staff to the surgical teams to the intensive-care nurses.
“It was the little things and just the way they delivered their care,” he said. “I get choked up. It was a really hard time, but those people—I owe an incredible debt of gratitude to everybody there.”
Scholl is not yet able to do any bending, lifting, or twisting movements, which has been challenging as a father of two young kids. It’ll also be a while before he’s back to his usual physical activity. But, Scholl feels mostly gratitude.
“It’s been an interesting journey, because while I would love to be out hiking and biking, and it’s frustrating I can’t, there’s a reality that sets in and I think, well, there’s a very good chance this could have never happened again period,” he said.
So, for now, Scholl continues to walk around his neighborhood with the support of a brace and trekking poles. But Dr. Uribe expects Scholl to be able to return to his normal activities once his vertebrae have fused together.
“Not only is it our goal to stop the tumor but to also bring people back to their normal life,” Dr. Uribe said. “Andy had amazing results. Now he can get his life back on track.”
Like his father had offered him, Scholl has some words of his own for people preparing to undergo neurosurgery.
“Not to sugarcoat it, but there’s another side to this,” he said. “Being on the recovery side, it’s just a wonderful place to be.”