DoD Funds Study of Neuropsychiatric Symptoms in Parkinson’s
Scientists at Barrow Neurological Institute and other institutions are putting their heads—and skill sets—together to investigate whether a specific network of brain cells contributes to the emotional, behavioral, and cognitive symptoms often seen in Parkinson’s disease. Spoiler alert: We’re not talking about the dopamine circuit.
The United States Department of Defense (DoD) has awarded $3 million to a team of researchers, led by Barrow Neurological Institute, to delve into the underlying cause of neuropsychiatric symptoms in Parkinson’s disease.
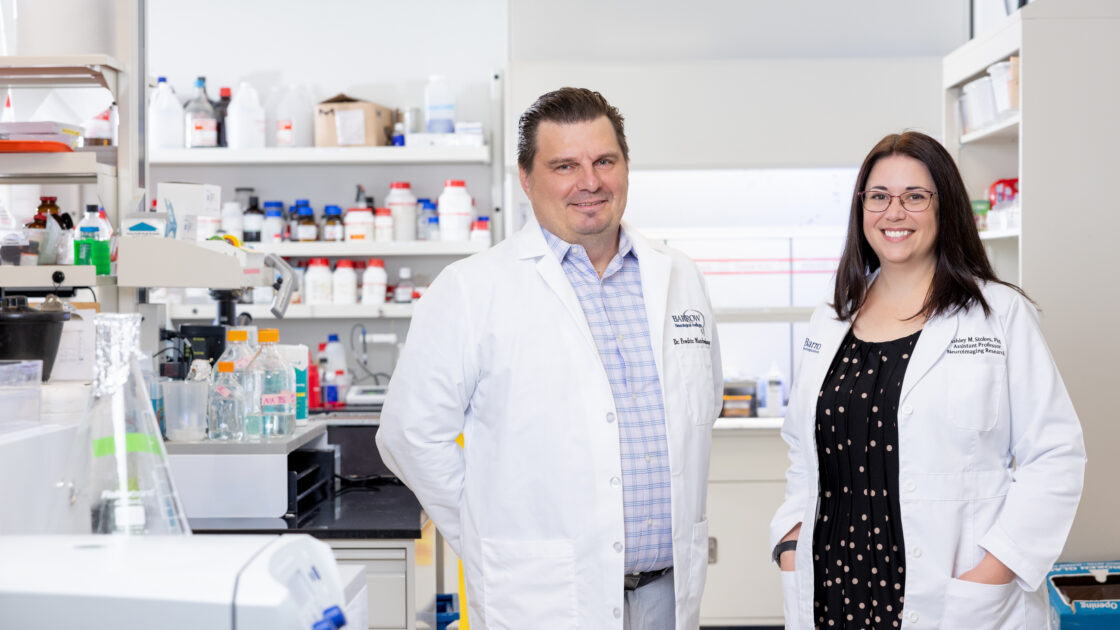
Barrow Associate Professors Fredric Manfredsson, PhD, and Ashley Stokes, PhD, are two of the four principal investigators who received the 2024 Parkinson’s Synergistic Idea Award. This grant fosters multidisciplinary collaboration by encouraging researchers to design individual but complementary experiments all focused on an overarching theme.
The award will provide four years of funding for the team, which also includes University of Illinois Chicago Professor Kuei Tseng, MD, PhD, and Binghamton University Professor Christopher Bishop, PhD. The four investigators will combine their unique skill sets to test their overall hypothesis: that structural and functional changes to serotonin-producing neurons contribute to neuropsychiatric symptoms in Parkinson’s disease.
Parkinson’s Disease: More than Movement Symptoms
While many people recognize Parkinson’s disease by its movement-related symptoms, such as shuffling feet and shaky hands, this progressive neurological disease can also manifest in ways not related to movement. These lesser-known “non-motor” symptoms may include sleep disorders, speech and swallowing difficulties, digestive problems, sensory changes, and—of course—neuropsychiatric symptoms.
“The general public, they see what they see, right? The tremors, the slowness of movement, but they don’t see everything that a patient is actually experiencing,” said Dr. Manfredsson, who is directing the research team.
Broadly speaking, neuropsychiatric symptoms describe emotional, behavioral, and cognitive changes. More specifically, these symptoms may include depression, anxiety, apathy, psychosis, impulse-control disorders, and difficulties with thinking, learning, and remembering.
“Non-motor symptoms, such as cognitive disorders and neuropsychiatric symptoms, have the potential to tremendously impact quality of life in patients living with Parkinson’s disease,” said Muhammad Ali Parkinson Center Director Holly Shill, MD. She is contributing to Dr. Manfredsson’s experiments, along with Barrow biostatistician Wonsuk Yoo, PhD. “This research will help us understand the mechanisms behind these symptoms and, more importantly, identify potential treatments,” she added.
Despite a growing awareness of neuropsychiatric symptoms in Parkinson’s disease, these symptoms remain challenging to manage with existing treatments. Answering the question of what’s causing these symptoms would mark a key milestone in the search for more effective therapies.
Drawing on their previous work, these four investigators suspect that answer lies in the network of brain cells that produce serotonin.
Homing in on Serotonin Neurons
Parkinson’s disease is characterized by the deterioration of a different system of neurons: those that produce dopamine. As a neurotransmitter, dopamine plays a crucial role in communication between nerve cells. While this chemical messenger is often associated with mood, it also facilitates other functions including movement.
Levodopa, a medication that can ease movement-related symptoms by boosting the amount of dopamine in the brain, serves as the first-line treatment for managing Parkinson’s disease. Precisely where that dopamine supply comes from, however, isn’t entirely clear.
While performing separate studies of levodopa-induced dyskinesia, a term for uncontrollable muscle movements linked to the medication, Drs. Manfredsson and Bishop identified the same possible culprit behind the side effect: the serotonergic circuit. They are investigating this further in a collaborative study funded by the National Institutes of Health (NIH).
Like dopamine, serotonin carries messages from one nerve cell to another across a junction called the synapse. Serotonin helps to regulate mood and many bodily functions, such as digestion and sleep. Recent studies have also found that serotonin-producing neurons can convert levodopa to dopamine, possibly accounting for the dopamine boost in patients treated with the medication.
“The problem is: Serotonin neurons are not supposed to release dopamine, so they don’t have that self-regulation,” Dr. Manfredsson explained.
These peaks and valleys in dopamine levels could be responsible for altering the structure of synapses in the brain. In other words, the serotonin circuit may be rewiring itself incorrectly to compensate for the fluctuation of the brain’s dopamine levels. This faulty wiring could be to blame for levodopa-induced dyskinesia and non-motor symptoms, like neuropsychiatric manifestations. The possibility of these side effects often deters people with Parkinson’s from taking levodopa.
“I’ve heard, anecdotally, people say that the motor symptoms aren’t the worst things that they experience; it’s the non-motor symptoms that really have the biggest impact on them,” Dr. Stokes recalled. “Sometimes there are people who don’t want to take the dopamine therapies because they’re so afraid of the side effects.”
Of course, there are changes occurring because of the disease process itself; the brain is degenerating, after all. So could neuropsychiatric symptoms be the result of neurodegeneration, or are they purely a side effect of dopamine therapies?
“It’s probably a combination of both,” Dr. Manfredsson said. “The ultimate goal is really to understand why this is happening, and our hypothesis is that serotonin neurons are modulating this. How, exactly, is what we’re trying to figure out—or determine whether or not it’s actually the serotonin neurons.”
Four Minds Are Better Than One
With this grant, the four researchers will run individual experiments and piece them together in an effort to complete a larger puzzle.
“We’re all working with the same model and generating the model at each site, and then there’s a series of experiments aimed at answering very specific questions around this overall theme,” Dr. Stokes explained.
Dr. Manfredsson will perform histology on brain tissue donated by people who have died with Parkinson’s disease—gathering static, high-resolution, microscopic pictures of how the serotonin neurons are wired. He’ll also generate and provide his co-PIs with tools to study neuronal circuits in isolation in a rat model. To do so, he’ll draw on his gene-therapy expertise, using viral-based vectors that can selectively activate very precise circuits—in this case, the serotonin circuit.
Dr. Tseng, an electrophysiologist, will apply these tools to examine the electrical communication between nerve cells in the rat model. Combining his physiological readouts with Dr. Manfredsson’s histological readouts will allow them to map functional and structural synaptic changes. Dr. Bishop will then assess this data in the context of changes to behavior and brain chemistry.
Dr. Stokes will focus more on the big picture, observing serotonergic circuit changes in relation to other networks in the brain. She’ll perform this work using the 7-Tesla (7T) preclinical scanner, a powerful magnetic resonance imaging (MRI) machine housed in the Barrow Neuroimaging Innovation Center.
“So not really looking at a cellular level, but rather a nodes-and-hubs level within the functional connectome and structural connectome of the brain,” she explained.
Finally, all of the data will go back to Dr. Manfredsson, who will compare the team’s findings in the rat model to his observations in the postmortem human brains.
This combination of neuroanatomy, neuroimaging, neurophysiology, and neurochemistry expertise will equip the team to generate a first-of-its-kind comprehensive map of changes underlying non-motor symptoms in Parkinson’s—a feat one investigator could not accomplish alone.
Not only do the researchers hope to fully characterize these structural and functional changes, but they aim to demonstrate that serotonin neurons significantly contribute to the development of non-motor Parkinson’s symptoms. Furthermore, they intend to develop imaging parameters that can be directly extended to human patients.
Keeping the Patient in Mind
If they prove their hypothesis true, the team will be poised to rapidly translate their findings to clinical trials—between the imaging parameters they’re developing and the existing FDA-approved drugs that could be repurposed to treat serotonin dysfunction in Parkinson’s.
In another parallel study funded by the NIH, Drs. Stokes and Manfredsson are working to develop imaging-based biomarkers of Parkinson’s disease and trying to use these measurable indicators to identify exactly how and where Parkinson’s wreaks havoc on the brain—especially beyond the dopamine circuit.
“Non-motor symptoms, such as cognitive disorders and neuropsychiatric symptoms, have the potential to tremendously impact quality of life in patients living with Parkinson’s disease. This research will help us understand the mechanisms behind these symptoms and, more importantly, identify potential treatments.”
-Holly Shill, MD, Director, Muhammad Ali Parkinson Center
“So it’s been an evolving story,” Dr. Manfredsson said. “We’re building a stronger and stronger body of work.”
Dr. Manfredsson noted another advantage that positions the team for clinical trial development: Barrow is home to the world-renowned Muhammad Ali Parkinson Center. The Center sees a high volume of patients with Parkinson’s disease and boasts extensive clinical trial experience.
“As we start generating more data on proof-of-concept that this circuit is really involved, then we can put more effort into looking into exactly which class of serotonergic drugs might work for this,” Dr. Manfredsson explained. “If we can start figuring out how to treat people with medication without all of these side effects, we can extend their quality of life.”



