Dr. Rita Sattler Brings Neurodegeneration Research to Barrow
“ALS is a universal, fatal disease,” she said. “There is only one therapeutic on the market, which marginally increases the life span of patients. So, there is a desperate need to find new therapeutic targets and, consequently, develop therapeutics to make patients’ lives better or maybe even extend their life span.”
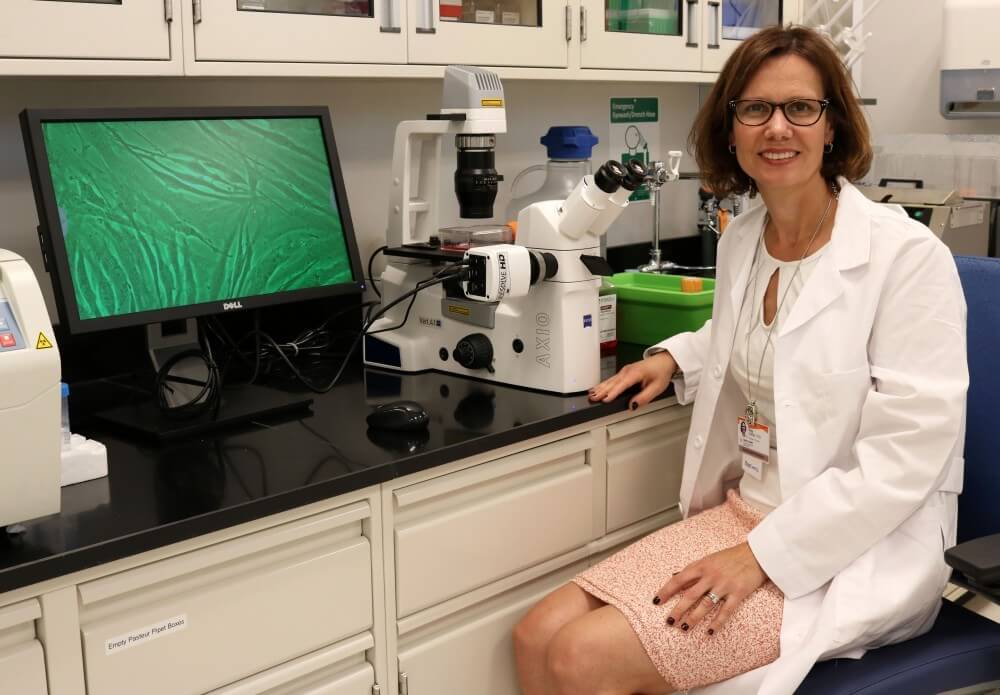
Dr. Sattler, who previously conducted her research at Johns Hopkins University, uses patient-derived human induced pluripotent stem cells to better understand the cellular and molecular aspects of disease pathways. Until recently, ALS had only been studied in mouse models and postmortem patient tissue.
“Animals have been very helpful because they allowed us to see how the disease progresses and what kind of cell types in the brain are involved in ALS, but it was very difficult to translate this into patient therapeutics,” Dr. Sattler said. “When we tested the drugs in mice, they were effective. When we tested them in patients, they failed.”
To make these adult stem cells, blood or skin cells are taken from a patient and reprogrammed. These stem cells can then be made into any cell in the human body, including neurons and glial cells – the two major cell types involved in ALS.
“If we use these patient cells and make them into brain cells, we can very quickly identify some of the disease mechanisms and pathways,” Dr. Sattler said. “If we have a drug that we know may interfere with a particular pathway, we can test very quickly whether it works on the patient-derived cell. If it works, we could then give the drug to the patient.”
However, Dr. Sattler said this is difficult to accomplish because ALS can progress rapidly. The average survival time is three to five years.

Associate Professor of Neurobiology
Despite the uniform fatality of ALS patients, research has shown that the path to disease is very unique for each ALS patient and numerous genes are involved in familial ALS. Patient diversity has made clinical trial designs difficult and led to a trend in stratifying patients.
The use of patient-derived human induced pluripotent stem cells is an approach to this patient diversity. When these stem cells are used to generate brain cells, the brain cells carry not only an individual patient’s mutation but also that patient’s unique genetic background.
“One thought is that we could have a personalized medicine approach for an individual patient and, in addition, it could be a way for us to stratify patients in the long run,” she said. “So, if we have a patient population that carries the same genetic mutation, we can develop potential therapeutics that work for that subset of patients.”
Dr. Sattler is particularly interested in the newly identified C9orf72 mutation and how it affects the function of the synapse, the structure where a neuron passes information to another neuron. This mutation is the most common in ALS.
“The way cells communicate with each other is by converting an electrical signal to a chemical signal and again to an electrical signal which is transmitted onto the next cell,” Dr. Sattler explained. “This chemical can be different types of neurotransmitters, and one of the most common ones that allows for this transmission of information from one neuron to another is the excitatory neurotransmitter glutamate.”
In the 1990s, research showed that ALS patients have increased levels of glutamate in their cerebrospinal fluid. Dr. Sattler said that when too much glutamate accumulates at a receiving nerve cell, it becomes toxic to the cell.
The first and only ALS drug approved by the U.S. Food and Drug Administration, riluzole, works to regulate glutamate so that it does not accumulate. This may slow the process of cell degeneration.
Dr. Sattler said the glutamate pathway is difficult to target because the receptors on the receiving neuron need to remain active to maintain important functions like learning and memory.
“You can’t just block these receptors,” she said. “You have to go one step further and see where there are particular proteins you can target that are activated after the receptors have been activated by glutamate – any target that is not detrimental to normal function.”
Dr. Sattler said that when Dr. Robert Bowser, the director of the ALS Research Center, approached her about bringing her research to Barrow, she thought it would be a perfect fit. One of Dr. Bowser’s research focuses is on biomarker development, which Dr. Sattler said goes hand-in-hand with therapeutic development.
Biomarkers are measurable indicators of a biological state, and they can be used to determine whether or not a patient is responding to a drug. Currently, the only valid readout in ALS clinical trials is survival, which Dr. Sattler said is often unreliable because every ALS patient has a different disease progression.
“If we have a biomarker that shows us the drug is working and we’re seeing improvement in regards to the pathway, we have a much better handle on whether or not the trial is going to be successful,” she said. “Having the ALS clinic here at Barrow, where the trials are actually run, we’re perfectly positioned to support efforts from pharmaceutical companies and within our own labs to initiate clinical trials.”
