Brain Arteriovenous Malformation (AVM)
Arteriovenous Malformation Overview
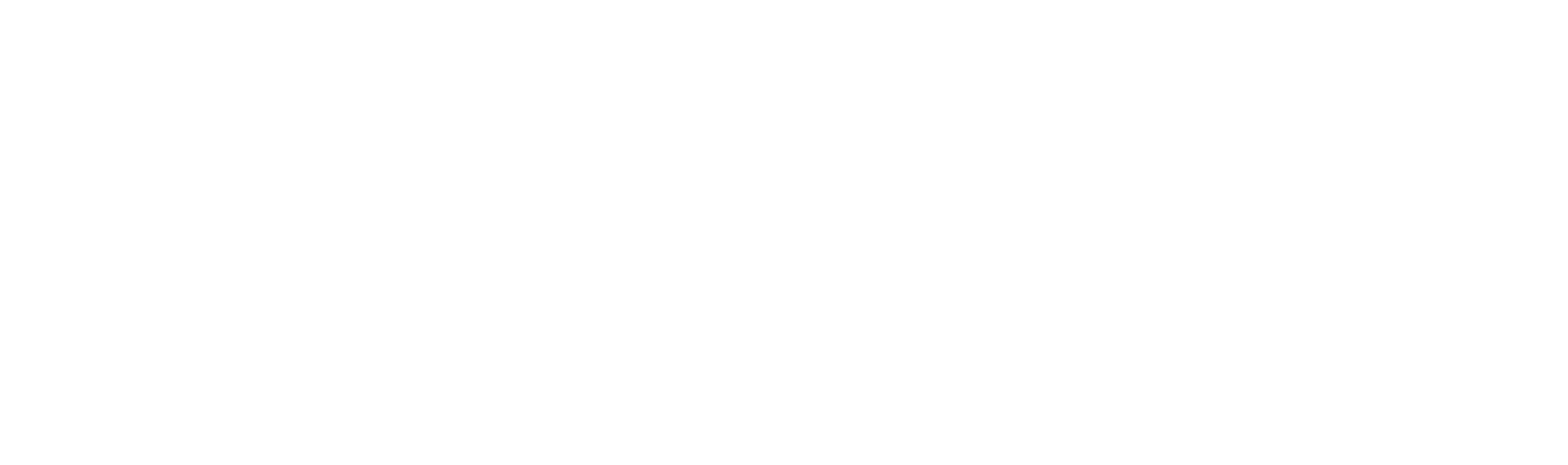
A brain arteriovenous malformation (AVM) is an abnormal tangle of blood vessels in the brain. This defect, which can occur anywhere in the central nervous system, causes blood to flow directly from arteries to veins through an abnormal passageway called a fistula instead of through capillaries. Generally speaking, there are three ways an AVM can damage the brain:
- Arteries and veins in an AVM can rupture, causing bleeding in the brain (hemorrhage)
- The amount of oxygen delivered to adjacent brain tissues is reduced, causing them to deteriorate or malfunction, producing seizures or neurological deficits
- An AVM can compress or displace parts of the brain
Anatomy of the Cerebrovascular System
The cerebrovascular system is the network of blood vessels that supply your brain with oxygen and nutrients. The system includes the internal carotid arteries, vertebral arteries, and their branches, which bring blood into the brain, and the veins that carry blood out of the brain.
The carotid arteries are located in the neck and provide blood to the front part of the brain (known as the anterior circulation). The vertebral arteries are located at the back of the neck and provide blood to the back part of the brain (the posterior circulation). These arteries branch off into smaller blood vessels, which then supply different areas of the brain.
Within the brain, the smallest blood vessels are called capillaries, which have thin walls that allow for the exchange of oxygen and nutrients with brain cells. The capillaries then join together to form larger blood vessels called veins, which carry the blood back to the heart to be reoxygenated via the internal jugular veins. As mentioned above, arteriovenous malformations in the brain bypass this capillary network, causing oxygenated and deoxygenated blood to mix via fistulas that directly connect arteries and veins in an area of the AVM known as the nidus.
The cerebrovascular system is essential for the proper functioning of the brain. Any disruption of blood flow to the brain can cause serious health problems, such as stroke or cognitive impairment. Therefore, maintaining a healthy lifestyle and managing risk factors such as high blood pressure or diabetes is important for maintaining the health of the cerebrovascular system.

Arteriovenous Malformation Symptoms
Symptoms can vary depending on the severity and location of the arteriovenous malformation, or they may never appear at all.
Symptoms of a brain AVM may include:
- Headaches
- Seizures
- Muscle weakness or paralysis
- Problems with balance and coordination (ataxia)
- Pain or unusual sensations throughout your body, such as tingling or numbness
- Dizziness
- Visual disturbances such as loss of part of the visual field
- Inability to control eye movement
- Problems understanding language (aphasia)
- Memory deficits
- Mental confusion, hallucinations, or dementia
Most AVMs cause few symptoms, if any.
AVMs can share symptoms with other conditions. Imaging tests by a medical professional are needed to diagnose an AVM.
Arteriovenous Malformation (AVM) Treatments
Treatment depends on the size, location, and symptoms of the arteriovenous malformation. Your doctor may recommend one or a combination of the following treatments:
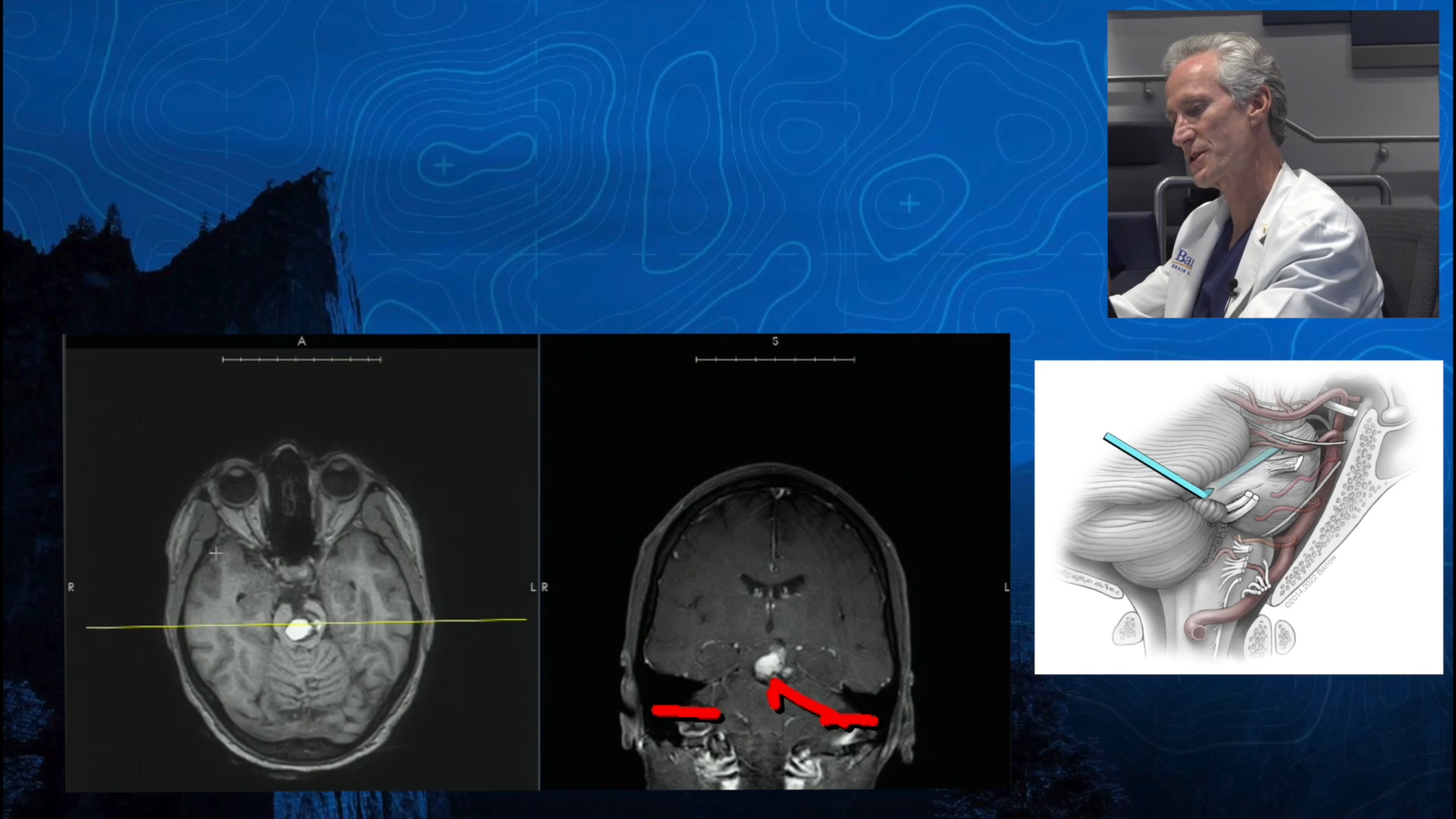
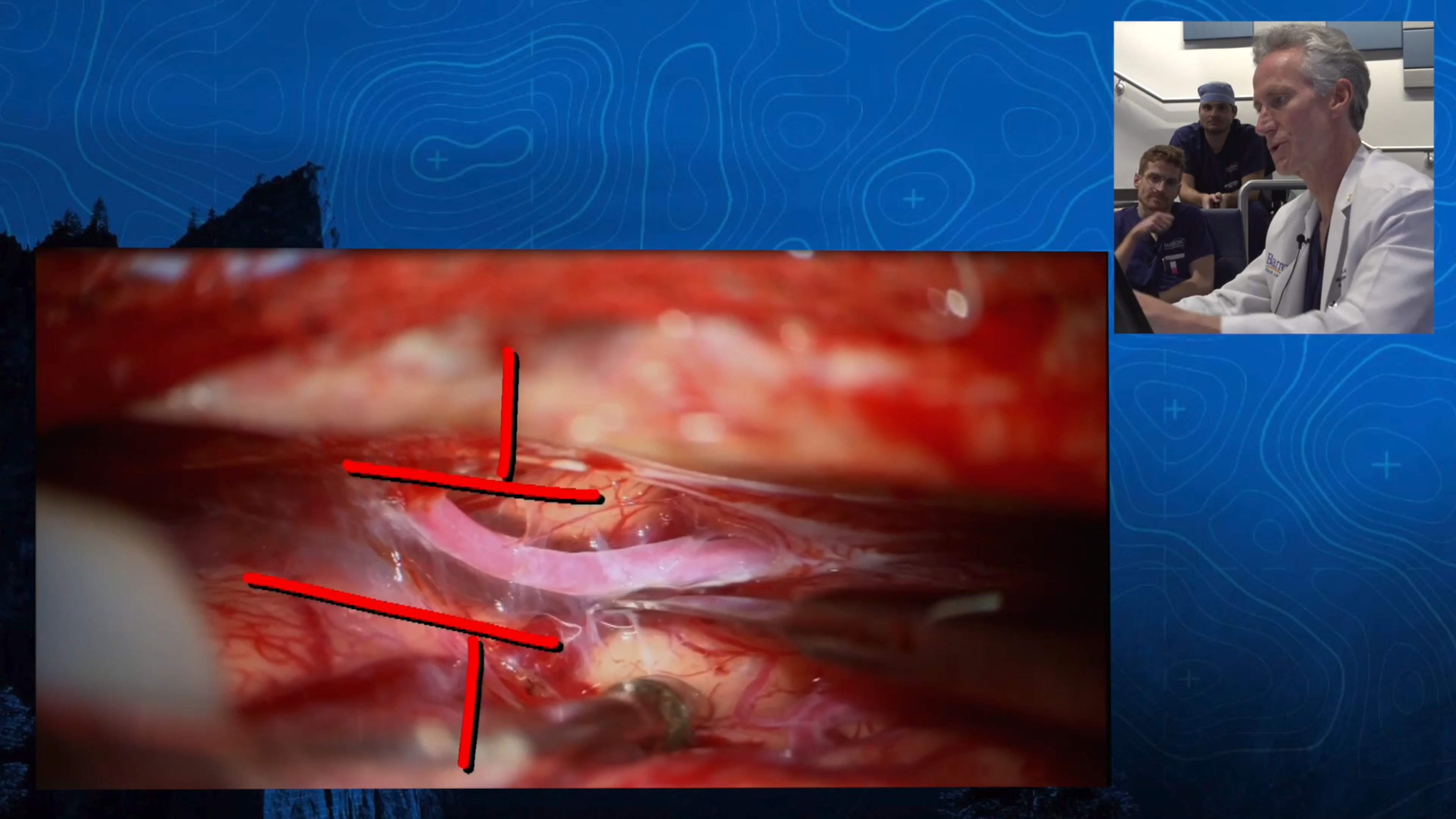
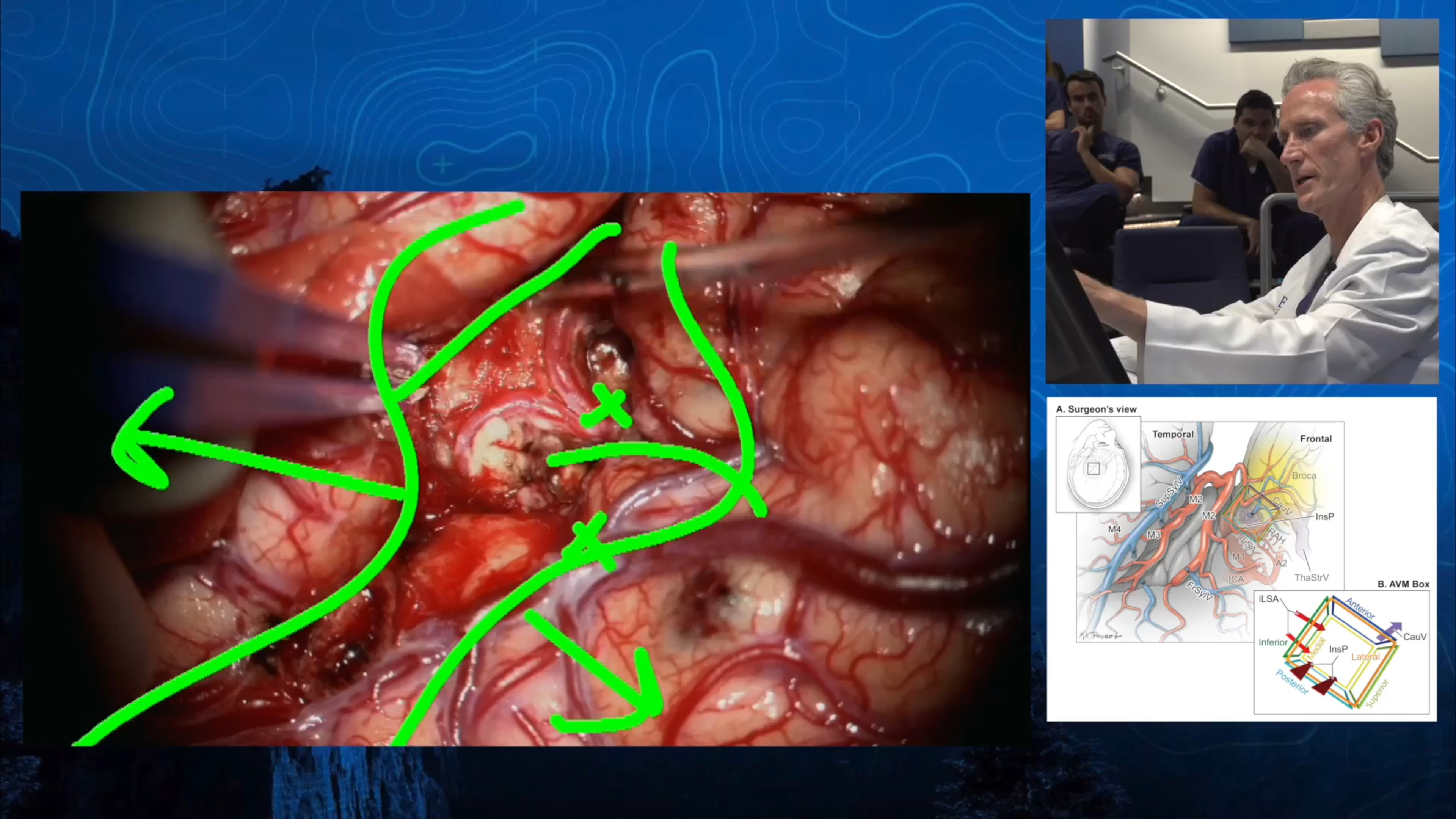
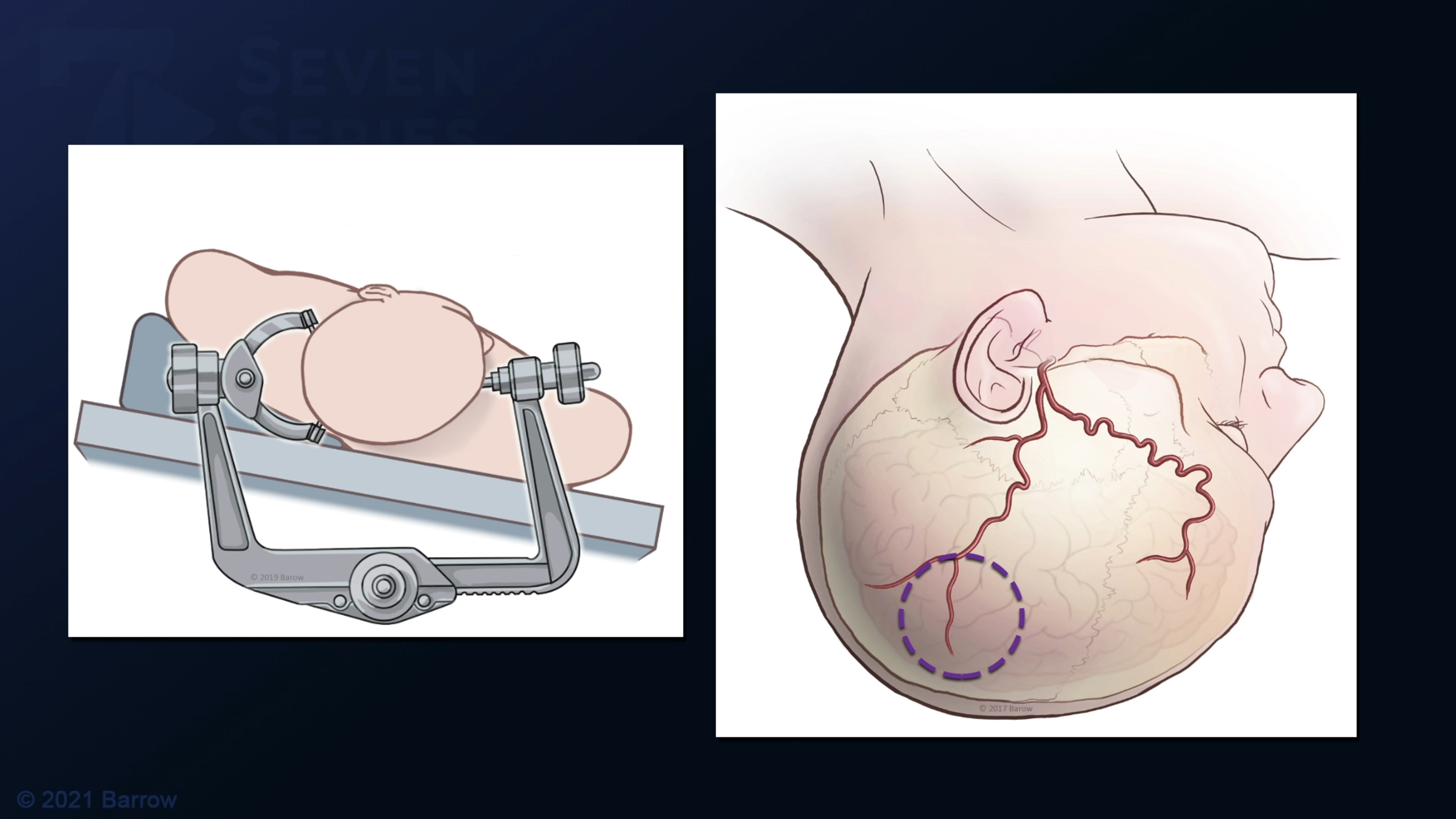
- Surgery – The arteriovenous malformation is removed from the brain using microsurgical techniques that close the abnormal feeding arteries, separate the tangle from the adjacent brain, and cut the veins draining the AVM.
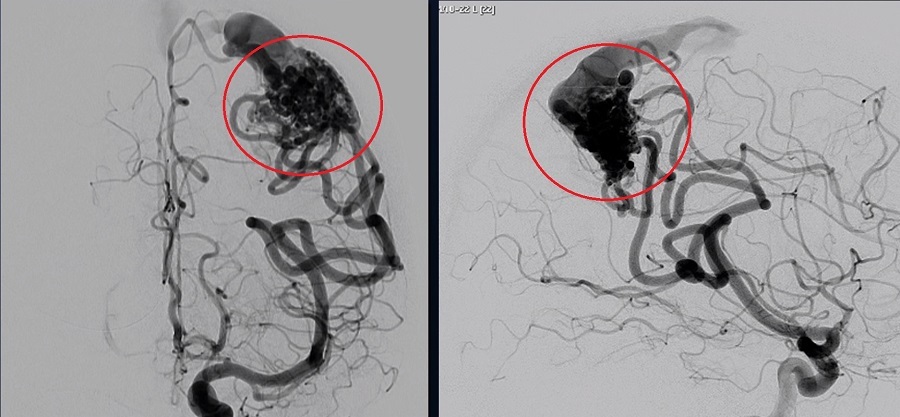
- Endovascular embolization – In this minimally invasive technique, a catheter is guided through the network of arteries until the tip reaches the site of the AVM. Various branches of the AVM are then plugged with a material such as glue or polymer cast. Embolization is usually used as a precursor to surgery to reduce the blood flow through the AVM, but can be used as a stand-alone treatment in some cases.
- Radiosurgery – In this noninvasive procedure, focused beams of radiation are targeted at the AVM and, over the course of 2-3 years, the arteries respond by scarring and closing down. Radiosurgery can be curative or can shrink an AVM down to a size that is more favorable for surgery. Gamma Knife and Cyberknife radiosurgeries are offered at Barrow.
Prognosis and Life Expectancy
A patient’s overall survival with an AVM depends on the bleeding behaviors of the lesion. There is about a 2-4% hemorrhage risk from an AVM annually. If an AVM does rupture, the survival rate is about 90%. The morbidity rate is about another 25% and includes patients who survive but then have some kind of brain damage or neurologic deficit. All statistics considered, the risk of dying annually if you have an AVM is relatively low.
An AVM can be completely cured by surgical resection. If the entire AVM is successfully removed by surgery, then it is considered cured. An AVM can also be completely obliterated by radiosurgery over time (2-3 years), but efficacy rates are lower (50-80% depending on its size). Embolization can cure a smaller number of carefully selected AVMs.
An AVM can slightly decrease life expectancy. But, by and large, you can expect to return to a normal life and have a normal life expectancy if your AVM is cured by complete surgical removal. This is especially true for young people.
Brain AVM Recurrence
An AVM that has been successfully treated can come back in children, adolescents, and young adults, because of their hormonal state and the continual growth that stimulates blood vessels in these patients (the growth of blood vessels is called angiogenesis). Recurrence of AVM is rare, occurring in less than 2% of patients whose AVMs were completely removed and more frequently in patients whose AVMs ruptured initially.
However, this is incredibly rare. Dr. Lawton, the most experienced brain AVM surgeon at Barrow and one of the most experienced in the world, has operated on more than 1,000 AVMs and has only seen five recur.
Grading Brain Arteriovenous Malformations
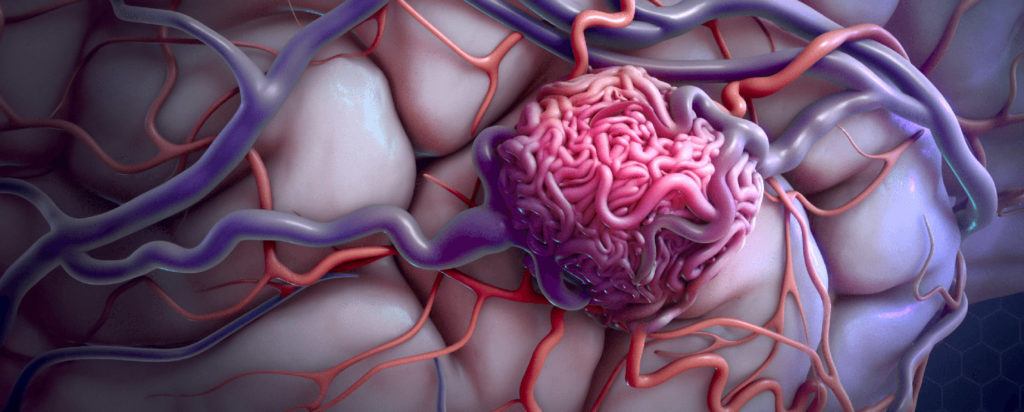
Both of the seminal grading scales that are used to rate and classify brain AVMs were developed by current faculty at Barrow Neurological Institute, Robert F. Spetzler, MD, and Michael T. Lawton, MD. These systems are used to predict the risks of open brain surgery to treat an AVM, with higher grades being associated with more risk of complications.
The Spetzler-Martin AVM Grading System
Under the Spetzler-Martin grading system, introduced in 1986, an arteriovenous malformation is assigned points based on the following criteria:
- Size of the AVM nidus, which is the part of the lesion that is supplied by the feeding arteries and draining veins
- Small, or less than 3 cm (1 point)
- Medium, or 3-6 cm (2 points)
- Large, or greater than 6 cm (3 points)
- Eloquence of the surrounding brain, meaning the proximity of the AVM to structures that control sensory processing, language and communication, and movement
- Non-eloquent (0 points)
- Eloquent (1 point)
- Venous drainage, which describes where the vein(s) that drain the AVM are located
- Superficial veins only (0 points)
- Deep draining vein(s) (1 point)
Adding up the points from each section results in an AVM grade between I and V, with lower-grade AVMs being less risky to treat with open neurosurgical approaches and higher grade AVMs more likely to result in neurological complications after surgery.
The Lawton-Young Supplementary AVM Grading System
The Lawton-Young grading system for brain arteriovenous malformations was developed in 2010 as a supplement to the Spetzler-Martin system, which was well established by this time. In combination with the Spetzler-Martin system, it provides a better prediction of the risk of surgery than does the Spetzler-Martin system on its own.
Under the Lawton-Young system, a brain arteriovenous malformation is assigned points based on the following criteria:
- The age of the patient
- Less than 20 years old (1 point)
- Between 20 and 40 years old (2 points)
- More than 40 years old (3 points)
- Whether or not the AVM has bled in the past
- Yes, has bled previously (0 points)
- No, has not bled previously (1 point)
- The compactness of the AVM, with compact AVMs being less likely to have brain tissue interspersed within the nidus than diffuse AVMs
- Compact (0 points)
- Diffuse (1 point)
As with the Spetzler-Martin scale, the points are added up and a grade between I and V is assigned. Then, the score is added to Spetzler-Martin grade to create a supplemental grade on a 10-point scale, with a score of one having the least risk of complications from surgery and a score of 10 having the most risk of complications from surgery.
Brain AVM Frequently Asked Questions
How common are arteriovenous malformations?
An AVM is very rare and affects less than one percent of the population, or about 10 per 100,000 people.
An estimated 300,000 Americans are affected by arteriovenous malformations of the brain and spinal cord (neurological AVMs), but only about 12 percent of the affected population will have symptoms.
Who gets arteriovenous malformations?
Arteriovenous malformations are equally common among men and women of all races and ethnicities. They are believed to be congenital (existing at birth), but they can enlarge over time and cause symptoms at any age.
Pregnancy can sometimes cause a sudden onset or worsening of symptoms because of cardiovascular changes, such as increases in blood volume and blood pressure.
Can you live with a brain AVM?
Many people do live with a brain AVM: Some are too big, too dangerous, and too risky to take out or treat with radiosurgery or other methods. These individuals live with their AVM, and can do well. However, if a non-bleeding AVM converts to a bleeding AVM, the resulting complications and neurological deficits that might require treatment.
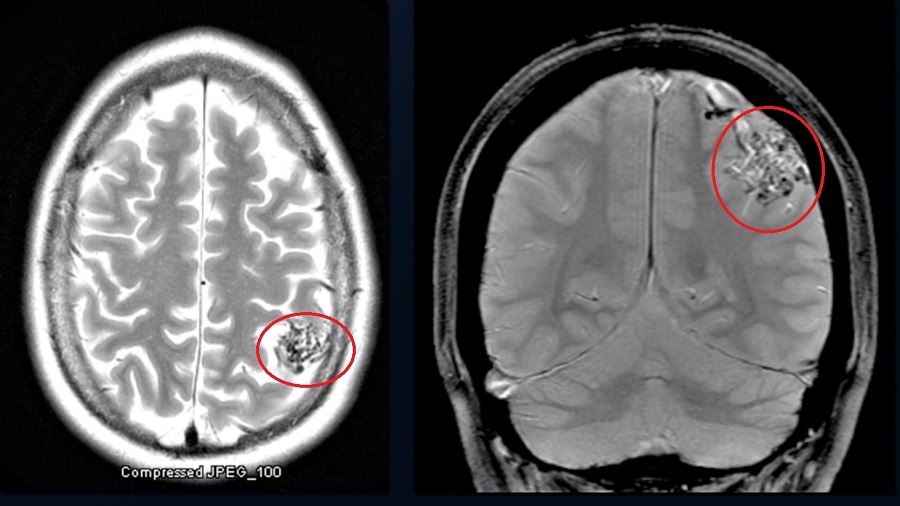
How are arteriovenous malformations diagnosed?
Most arteriovenous malformations are detected through diagnostic imaging, such as a CT or MRI scan. Angiography, an imaging technique that involves the injection of a special dye, may be used to get a better look at the AVM.
Because most people with AVMs experience few symptoms, they are often discovered during treatment for an unrelated disorder.
Can a cerebral arteriovenous malformation cause personality changes?
An AVM does not necessarily cause personality changes, unless it has bled and damaged the brain.
Is an AVM serious?
Yes, being diagnosed with a brain AVM is serious. If you’ve been given the diagnosis of having an AVM, you should make an appointment with a neurosurgeon who is an expert in treating these lesions. Your neurosurgeon will then recommend a care plan that could include observation, treatment, and multimodality intervention.
What causes an arteriovenous malformation to bleed?
In AVMs, blood flows directly from arteries to veins without the buffer of capillaries. Arterial pressure is too high for veins to accommodate due to their thinner walls, which can weaken the blood vessels and cause rupture. Researchers are studying other possible factors in AVM rupture.
An AVM is not a stroke, but an AVM can cause a hemorrhagic stroke if it ruptures and bleeds into the brain. This is called an intracerebral hemorrhage, or occasionally a subarachnoid hemorrhage.
Can an arteriovenous malformation cause dementia?
No, the presence of an AVM does not cause dementia. However, a hemorrhagic stroke caused by an AVM can cause problems with memory.
Can an arteriovenous malformation go away on its own?
No, an AVM cannot go away on its own. However, it can be removed with surgery, sealed off with endovascular embolization, or reduced in size with radiosurgery.
What is the difference between an AVM and a brain aneurysm?
An AVM is an abnormal connection between arteries and veins without intervening capillaries with blood flowing through vessels at a high speed and high pressure. An aneurysm is an outpouching of the arterial wall that forms a balloon, or bulge, which can burst. There’s no arteriovenous shunting with an aneurysm, meaning there is no “short circuit” of blood flow. This arteriovenous shunting is the hallmark of AVMs.
Is an AVM a birth defect?
Whether or not an AVM is a birth defect is controversial, with members of the medical and scientific community taking both sides. It once was assumed to be a birth defect but, more recently, AVMs have been produced in mice through genetic manipulation. In light of this, the tide is shifting toward viewing an AVM as a disease that progresses through a genetic mutation that occurs early in life, in combination with some angiogenic stimulus or event.
Can an AVM get worse?
Yes, an AVM can get worse over time if it enlarges, bleeds, or develops other features, like feeding artery aneurysms or venous varices that indicate that the tissues are getting weaker and more prone to bleeding.
Additional Resources
The Aneurysm and AVM Foundation
Videos
Note: These videos contain surgical footage. Viewer discretion is advised.
References
- Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg. 1986 Oct;65(4):476-83. doi: 10.3171/jns.1986.65.4.0476. PMID: 3760956.Mar;16(3):264-79. doi: 10.3171/2011.10.SPINE11291. Epub 2011 Dec 16. PMID: 22176427.
- Lawton MT, Kim H, McCulloch CE, Mikhak B, Young WL. A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Neurosurgery. 2010 Apr;66(4):702-13; discussion 713. doi: 10.1227/01.NEU.0000367555.16733.E1. PMID: 20190666; PMCID: PMC2847513.
- Park MT, Essibayi MA, Srinivasan VM, Catapano JS, Graffeo CS, Lawton MT. Surgical management outcomes of intracranial arteriovenous malformations after preoperative embolization: a systematic review and meta-analysis. Neurosurg Rev. 2022 Dec;45(6):3499-3510. doi: 10.1007/s10143-022-01860-x. Epub 2022 Sep 27. PMID: 36168072.
- Lawton M, Rutledge W, Kim H. et al. Brain arteriovenous malformations. Nat Rev Dis Primers 1, 15008 (2015). https://doi.org/10.1038/nrdp.2015.8