Brain Tumors
Brain Tumors Overview
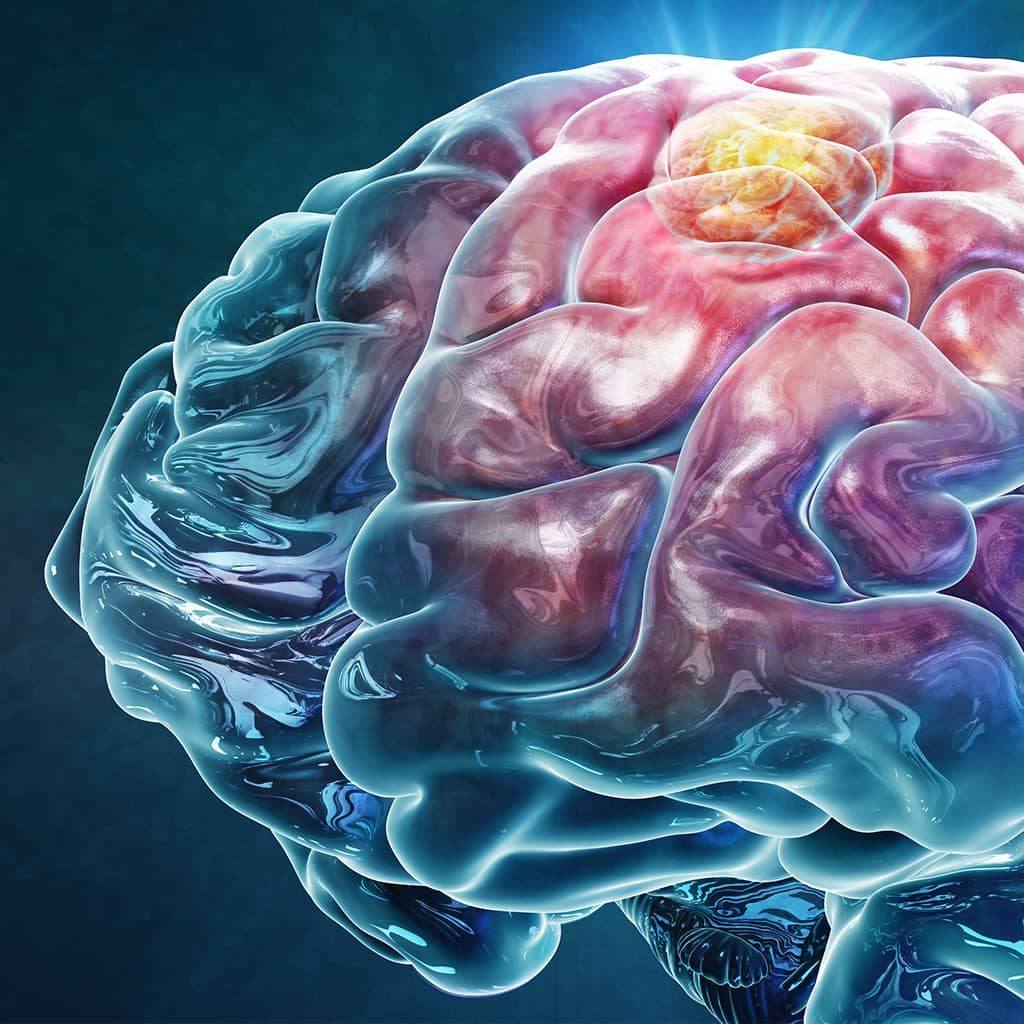
A brain tumor is a mass of abnormal cells that are caused by uncontrolled cell growth in the brain or as a result of cancer spreading from another part of the body to the brain.
While all tumors are either benign (noncancerous) or malignant (cancerous), they’re also categorized as either primary or secondary, known as metastatic:
- Primary brain tumors start in the brain or the tissues near it, like the membranes covering the brain called the meninges or the pituitary gland. These types of tumors happen when mutations occur in the DNA of normal cells, causing the cells to multiply abnormally and survive in conditions normal cells wouldn’t.
- Secondary brain tumors come from cancer that starts somewhere else in the body and then spreads or metastasizes to the brain. Sometimes, a secondary brain tumor is the first sign of a cancer that’s started in another location.
There are more than 100 different types of brain and intracranial tumors, which are
tumors within the skull that may not be a part of the brain itself. They get their name
from the kind of cell in which they first form—for example, astrocytomas arise from
astrocyte cells. Common brain and intracranial tumors found in adults include:
- Gliomas: These are brain tumors that start in the glial cells, which help keep nerves healthy. There are many categories of gliomas, and they’re the brain tumors that are most likely to be malignant or cancerous. Some examples of gliomas include glioblastomas, astrocytomas, and oligodendrogliomas. Glioblastoma is the most common and aggressive type of primary brain cancer in adults. Doctors frequently treat these tumors with a combination of surgery, radiation, and chemotherapy.
- Meningiomas: A meningioma is a tumor that starts in the meninges, the protective coverings of your brain and spinal cord. Most meningiomas are slow-growing and are often benign, meaning they don’t invade nearby tissue or metastasize to other body parts. However, some meningiomas exhibit locally aggressive behavior, invading and weakening nearby bones or other structures. Surgery can cure most meningiomas, although optimal treatment for some includes both surgery and radiation.
- Schwannomas: These tumors originate from the Schwann cells that create the protective, insulating sheath surrounding neurons. Schwannomas tend to grow slowly and are generally benign. However, in rare cases, they can be malignant. Many schwannomas can be treated and cured through surgery, while sometimes, radiation therapy after the surgery is recommended.
- Pituitary adenomas: Pituitary adenomas are intracranial tumors that grow on the pituitary gland. While they are usually not cancerous, they can cause issues by releasing excess hormones produced by the pituitary gland. Even adenomas that don’t release hormones (nonfunctioning adenomas) can create symptoms by putting pressure on nearby structures, such as the optic nerve or internal carotid arteries. When successfully treated, pituitary tumors often improve and can go away altogether.
What causes a brain or intracranial tumor?
In most cases, it’s not known what, exactly, causes the genetic mutations that lead to primary brain tumors or intracranial tumors. However, there are some known risk factors which include:
- Age: People between 65 and 79 are most likely to be diagnosed with a brain tumor.
- Genetic syndromes: Rare genetic conditions, such as neurofibromatosis type I, NF2-related schwannomatosis (previously known as neurofibromatosis type 2), Li-Fraumeni syndrome, and Lynch syndrome, can cause brain and intracranial tumors.
- Viral infections: There are rare types of brain tumors, like primary central nervous system lymphomas, that may be associated with viral infections like the Epstein-Barr virus (EBV) or HIV.
- Radiation exposure: Children who receive radiation to the head have an elevated risk of brain tumor development compared to adults.
- Hormonal factors: Hormonal imbalances or exposure to hormones like estrogen or progesterone may influence the development of certain types of brain tumors that contain hormone receptors.
- Environmental factors: Although there isn’t a conclusive link, exposure to certain chemicals, like pesticides, solvents, and industrial pollutants, has been investigated as a potential risk factor for brain tumor growth.

Brain Tumor Symptoms
Brain tumor symptoms vary widely depending on the type, location, and size of the tumor. In other words, there are no specific symptoms that only occur as a result of a brain tumor. Some tumors won’t present symptoms until they have reached a specific size, then cause a rapid decline in health. Meanwhile, others will develop very slowly over time with minimal symptoms.
That said, symptoms you might notice if you or someone you know has a brain tumor can include:
- New onset or change in the pattern of headaches: These include headaches that aren’t improving with typical headache remedies, or you’re experiencing them more often, or they’re growing in intensity or worsening with activity.
- New onset of seizures: A brain tumor can cause seizures because it disrupts the brain’s regular electrical activity. Seizures can range from muscle jerks and spasms to a loss of consciousness and body functions. Changes in vision, smell, or sensation without losing consciousness can also denote a seizure.
- Difficulty with balance: The cerebellum is a portion of the brain in the back of the head that controls motor functions like balance for walking or standing. A tumor here can cause problems with these functions.
- Difficulty speaking or confusion: This can look like a change in speech, hearing, or memory, like problems understanding or retrieving words.
- Gradual loss of sensation or movement in an arm or a leg: This gradual loss of sensation or movement in the body happens when a tumor affects areas of the brain in charge of motor functions.
- Unexplained nausea or vomiting: Increased pressure inside the skull from the tumor can result in nausea and vomiting.
- Personality or behavior changes: These can manifest as new or unusual emotional states, such as changes in judgment, aggressiveness, loss of initiative, and even sluggishness. Depression and anxiety, mainly if either develops suddenly, can be an early symptom of a tumor in the brain.
- Blurred vision, double vision, or loss of peripheral vision: Vision changes, such as partial vision loss or even double vision, can result from a tumor in the temporal lobe, occipital lobe, or brain stem.
- Hearing problems: A brain tumor can exert pressure on nearby auditory pathways or influence the structures involved in auditory information processing.
- Fatigue or drowsiness: Brain tumors interfere with normal brain functions, including those regulating wakefulness. They can also cause an increase in the pressure in the skull, which leads to symptoms like fatigue, drowsiness, and lethargy.
If you’re concerned about experiencing new or persistent symptoms that align with these descriptions, it’s critical you talk to your healthcare provider as soon as possible.
Brain Tumor Diagnosis
Multiple steps are involved in accurately diagnosing the tumor’s location, type, and extent.
Your doctor might recommend the following exams and imaging tests to diagnose a brain tumor:
- Physical and neurological exam: First, your healthcare provider will ask about your symptoms, overall health, and family history of brain tumors or genetic conditions. Next, they’ll complete a neurological examination to assess neurological function, including reflexes, coordination, strength, and sensation.
- Magnetic Resonance Imaging (MRI): Imaging studies are crucial in visualizing the brain and identifying abnormalities. An MRI provides detailed brain images and can help determine a tumor’s location, size, and characteristics.
- Computed Tomography (CT): CT scans rely on X-rays to create detailed cross-sectional images of the brain and can help detect tumors while evaluating their size and location.
- Positron Emission Tomography (PET) scan: PET scans can evaluate the metabolic activity of brain tumors and determine their aggressiveness. Instead of only mapping brain infrastructure, a PET scan shows how your brain works.
- CT Angiography (CTA) and Magnetic Resonance Angiography (MRA): These scans, often completed with a contrast dye, locate blood vessels in the brain that can help your neurosurgeon better plan for removal.
- Biopsy: A biopsy establishes an exact tumor diagnosis by removing a small tissue sample from the tumor surgically or through stereotactic biopsy. Specialized neuropathologists examine the tissue under a microscope to determine the type of cells present, whether they’re cancerous or noncancerous, and other important characteristics that guide treatment decisions.
Additional tests, like cognitive or visual field testing, may be done to evaluate the tumor’s impact on overall brain function. Your doctor might also schedule you for electroencephalography (EEG) to assess the electrical activity in the brain to determine seizure risk.
Finally, genetic testing of tumor tissue can identify genetic mutations or alterations that can help predict the tumor’s behavior and response to treatment and identify people who can participate in personalized clinical trials based on unique tumor genetics. At Barrow Neurological Institute, our Ivy Brain Tumor Center can help oversee more detailed testing to identify a patient’s brain tumor subtype. This additional information helps our neurosurgeons, radiation oncologists, and neuro-oncologists to be even more precise in selecting treatments and clinical trials.
Brain Tumor Treatment
As with all other facets of a brain tumor, optimal treatment depends on the brain tumor’s type, location, size, growth rate, and your overall health. There is no single treatment that works best—each brain tumor is as unique as the person diagnosed with one. Often, a combination of treatments is used, and personalized approaches, like tumor profiling to look for specific gene mutations, can help determine the best treatments.
Optimal tumor treatment will involve a collaborative approach between neurosurgeons, neuro-oncologists, medical oncologists, radiation oncologists, and other specialists who work together to achieve the best possible outcome.

Brain Tumor Surgery
Surgery is often the primary treatment for brain lesions that are safe to remove without causing too much damage to the surrounding neurological tissue. The goal of surgery is to remove as much of the tumor as possible while preserving neurological function. Complete removal of a benign or noncancerous tumor can be curative. However, in the case of malignant or cancerous tumors, surgery is often followed by chemotherapy or radiation therapy.
The following are some of the general approaches used for brain tumor surgery:
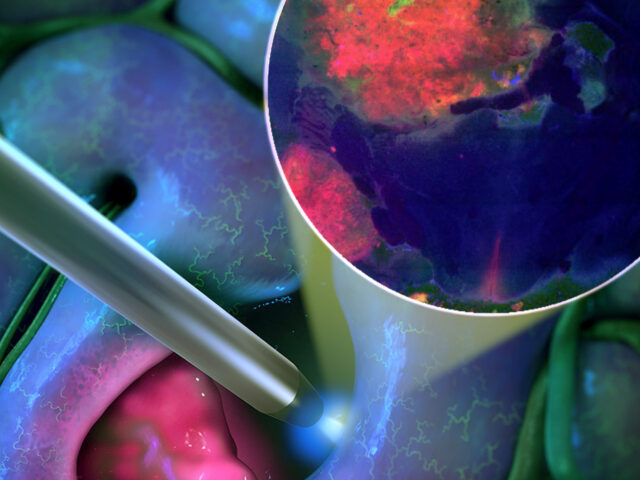
- Craniotomy: A craniotomy is the most common surgery for a brain tumor. During a craniotomy, a neurosurgeon will make an incision in the scalp, remove a portion of the skull, and access the brain to remove the tumor. Neurosurgeons use intraoperative imaging and highly specialized tools to visualize tumor tissue and remove it safely.
- Awake Craniotomy: Awake brain surgery, or awake craniotomy, is a specialized surgery for brain tumors in areas that control critical functions, like speech or movement. During awake brain surgery, you will be awake and alert while your surgeon removes the tumor, allowing the surgical team to monitor brain function in real-time and avoid damaging critical anatomy.
- Minimally invasive techniques: In some cases, your neurosurgeon might suggest minimally invasive surgical techniques to remove brain tumors. Minimally invasive brain tumor surgery uses smaller incisions and specialized instruments to access and remove the tumor, like endoscopic surgery and laser interstitial thermal therapy (LITT). These techniques can offer shorter recovery times, reduced risk of complications, and more minor scars.

Radiation Oncology
Radiation Therapy uses precisely aimed beams of radiation to destroy tumors. While it doesn’t remove the tumor, radiation therapy damages the nucleus of the tumor cells, which then lose their ability to reproduce and eventually die.
- Radiosurgery: This treatment focuses radiation at the site of the lesion while minimizing the radiation dose to the surrounding brain. Radiosurgery is often used for tumor recurrence but rarely used in initial treatment for glioblastoma, and the two most common forms are:
- Gamma Knife radiosurgery: This option destroys abnormal tissue through radiation beams focused on a precise tissue area. It is only lethal to cells within the immediate vicinity. Gamma Knife radiosurgery can only be used to treat lesions in the head and involves attaching a metal frame to the skull to focus radiation beams accurately.
- CyberKnife radiosurgery: This technique uses targeted energy beams to destroy tumor tissue while sparing healthy tissue. It uses image-guided robotics to deliver surgically precise radiation to help destroy tumors.
Chemotherapy, Targeted Therapy, and Immunotherapy
Your oncology treatment team might recommend using these treatments on their own or in conjunction with surgery and radiation therapy:
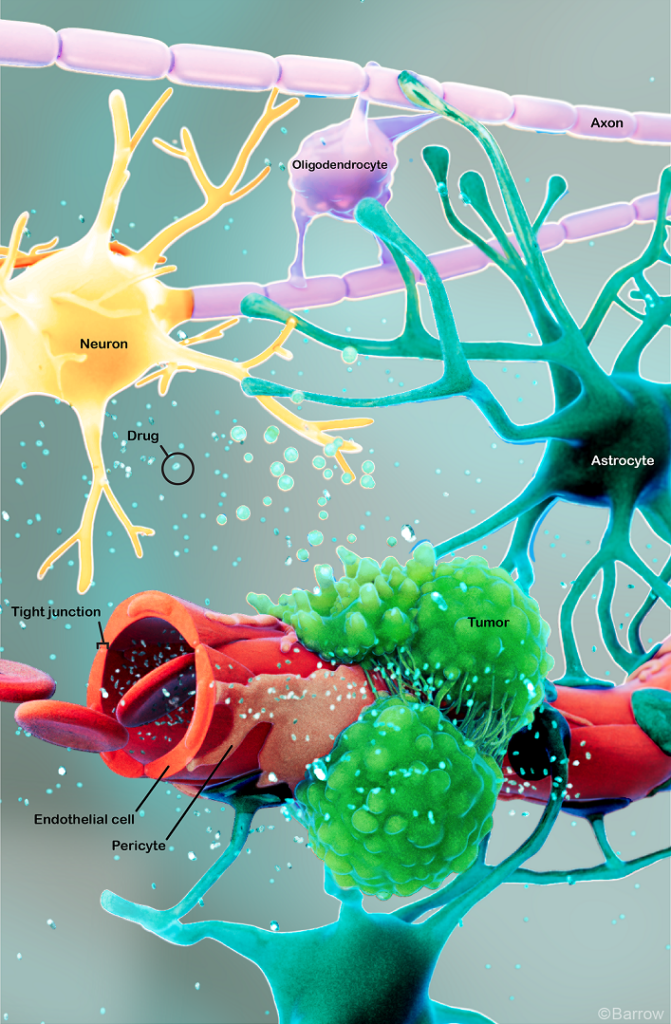
- Chemotherapy: Your oncologist can give chemotherapy drugs orally or intravenously to inhibit the growth of cancer cells, but it can be challenging for them to reach the brain due to the blood-brain barrier, which acts as a shield against chemotherapy drugs. For this reason, chemotherapy drugs are sometimes administered intrathecally, meaning they are injected directly into the cerebrospinal fluid (CSF). Chemotherapy is often combined with surgery or radiation therapy, especially with tumors that are difficult to remove surgically.
- Targeted Therapy: Targeted therapy uses compounds to target specific molecules vital to cancer cells’ metabolism and reproduction.
- Immunotherapy: Immunotherapy works via a series of drugs that boost the body’s immune system to recognize and attack cancer cells.
Supportive care is also essential to brain tumor treatment. It can look like medications to manage symptoms like pain, seizures, and swelling in the brain, as well as access to physical and occupational therapy as well as counseling for patients and their families.
Clinical Trials
Many clinical trials evaluating potential drugs for treating brain tumors are ongoing. Though the treatments are experimental and not yet FDA-approved, clinical trials can be the best option for those with difficult-to-treat tumors to improve the odds of finding an effective treatment for them and for future patients.
As home to the Ivy Brain Tumor Center, Barrow Neurological Institute is proud to be one of the country’s largest sites for brain tumor clinical trials.
Neuro-Rehabilitation for Quality of Life
At Barrow Neurological Institute, we give our patients access to various neuro-rehabilitation specialists to maximize independence. Neuro-rehabilitation can include physical therapy to help you regain strength and balance, speech therapy to support speaking, expressing thoughts, or swallowing, and occupational therapy to aid you in managing daily activities like bathing, dressing, and using the bathroom. Treating a brain tumor is about more than extending your life—it’s also equally focused on enhancing your quality of life.
One Central Location with Multiple Treatment Options
At Barrow Neurological Institute’s world-class Brain and Spine Tumor Program, we treat people with complex tumors in one robust, full-service location. Our sophisticated multidisciplinary team—neurosurgeons, head and neck surgeons, neuropathologists, neuro-oncologists, medical oncologists, and radiation oncologists, to name a few—can offer patients the latest treatments for head and neck cancers, including neurological and metastatic cancers.
Finally, we also offer a Brain Cancer Survivorship Program to foster relationships between families affected by brain tumors and provide ongoing support.
Common Questions about Brain Tumors
How common are brain tumors?
An estimated 1 million people in the U.S. are living with a brain tumor. Approximately 72 percent of all brain tumors are benign, while 28% are malignant.
Who gets brain tumors?
Anyone can develop a brain tumor. While it’s unclear what causes cells to grow abnormally, genetics may play a role.
Approximately 59 percent of brain tumors occur in women, while the other 41 percent happen in men. That said, malignant primary brain tumors—or tumors that begin in the brain—are found more often in men than women.
Experts estimate that in 2023, 94,390 people will receive a new primary brain tumor diagnosis, and of those, an estimated 67,440 will be benign, while an estimated 26,940 will be malignant.
What is the most common type of brain or intracranial tumor?
Metastatic, or secondary brain tumors, are the most common type of tumor that affects the brain. Meningiomas are the next most common, followed by glioblastomas.
The most common type of brain tumor in children under the age of 18 is medulloblastoma, which is most often diagnosed between the ages of 3 and 8. Medulloblastomas are malignant tumors that tend to develop in the cerebellum at the base of the brain near the brainstem.
Primary brain tumors are more common in children and older adults. In contrast, secondary or metastatic brain tumors are more common in adults than in children.
What is the prognosis for those with a brain tumor?
The prognosis for people diagnosed with a brain tumor truly depends on the type of tumor, its location, and how early it’s diagnosed and treated. The age and overall health of the patient, as well as how well the lesion responds to treatment, will also influence the overall prognosis. Benign brain tumors generally have a better prognosis than malignant ones.
While a prognosis provides an estimate of the likely course of the disease, it’s not a guarantee—each person’s brain tumor experience is unique. At the same time, elements like resilience, social support, and access to quality healthcare also play a role in determining outcomes. Additionally, ongoing research and advancements in treatment continue to improve outcomes and quality of life for those living with a brain tumor.
Can a brain tumor be prevented?
While there’s no fail-proof way to prevent brain tumors entirely, there are always steps a person can take to help reduce their risk. They include:
- Protecting against radiation: Minimizing exposure to ionizing radiation, like radiation therapy or medical imaging procedures, may decrease the risk of brain tumors later in life. However, this risk is generally considered low, and balancing the benefits of medical imaging or radiation therapy with the risks of having none is critical.
- Maintaining a healthy lifestyle: Regular exercise, a balanced diet, and avoiding tobacco and excessive alcohol consumption can reduce the risk of certain cancers.
- Protect against sunburns: Reducing UV radiation exposure from the sun with protective clothing and sunscreen helps prevent skin cancers, such as melanoma, which frequently can spread to the brain.
- Protecting against environmental toxins: Reducing exposure to environmental toxins and carcinogens that increase the risk of certain cancers is instrumental in protecting against brain tumors.
- Screening and early detection: For those with genetic predispositions, regular screenings and monitoring by healthcare professionals may help detect brain tumors at an early, more treatable stage.
Brain Tumor Resources
References
- Johnson KC, Tien AC, Jiang J, McNamara J, Chang YW, Montgomery C, DeSantis A, Elena-Sanchez L, Fujita Y, Kim S, Spitzer A, Gabriel P, Flynn WF, Courtois ET, Hong A, Harmon J, Umemura Y, Tovmasyan A, Li J, Mehta S, Verhaak R, Sanai N. Single nucleus transcriptomics, pharmacokinetics, and pharmacodynamics of combined CDK4/6 and mTOR inhibition in a phase 0/1 trial of recurrent high-grade glioma. medRxiv [Preprint]. 2024 Jun 7:2024.06.07.24308439. doi: 10.1101/2024.06.07.24308439. PMID: 38883740; PMCID: PMC11178017.
- Wang D, Geng H, Gondi V, Lee NY, Tsien CI, Xia P, Chenevert TL, Michalski JM, Gilbert MR, Le QT, Omuro AM, Men K, Aldape KD, Cao Y, Srinivasan A, Barani IJ, Sachdev S, Huang J, Choi S, Shi W, Battiste JD, Wardak Z, Chan MD, Mehta MP, Xiao Y. Radiotherapy Plan Quality Assurance in NRG Oncology Trials for Brain and Head/Neck Cancers: An AI-Enhanced Knowledge-Based Approach. Cancers (Basel). 2024 May 25;16(11):2007. doi: 10.3390/cancers16112007. PMID: 38893130; PMCID: PMC11171017.
- Duffau H, Berger M, Brastianos PK, Sanai N, Mandonnet E, McKhann GM. Introduction: Contemporary management of low-grade gliomas: from tumor biology to the patient’s quality of life. Neurosurg Focus. 2024 Feb;56(2):E1. doi: 10.3171/2023.11.FOCUS23731. PMID: 38301253.