Acromegaly
Acromegaly Overview
Acromegaly is a rare chronic condition defined by excess growth hormone (GH) and insulin-like growth factor-1 (IGF-1) in the blood as an adult. These heightened GH and IGF-1 levels eventually cause bones and soft tissues to grow larger than would be expected if the body were producing normal levels of GH.
By definition, acromegaly can only occur after your bones and other organs have stopped growing—in other words, around age 18 for women and slightly older for men. When too much GH is produced in people under 18 the condition is called gigantism.
Because GH and IGF-1 receptors are found everywhere in the body, acromegaly affects numerous organs, bones, and tissues. These include:
- Skin
- Liver
- Kidneys
- Thyroid
- Heart
- Joints
- Spine
While this condition can develop at any age after puberty, it’s most commonly diagnosed during middle age.
When successfully treated, acromegaly symptoms generally improve and some symptoms can go away altogether. When untreated, acromegaly can lead to serious health problems and even early death.
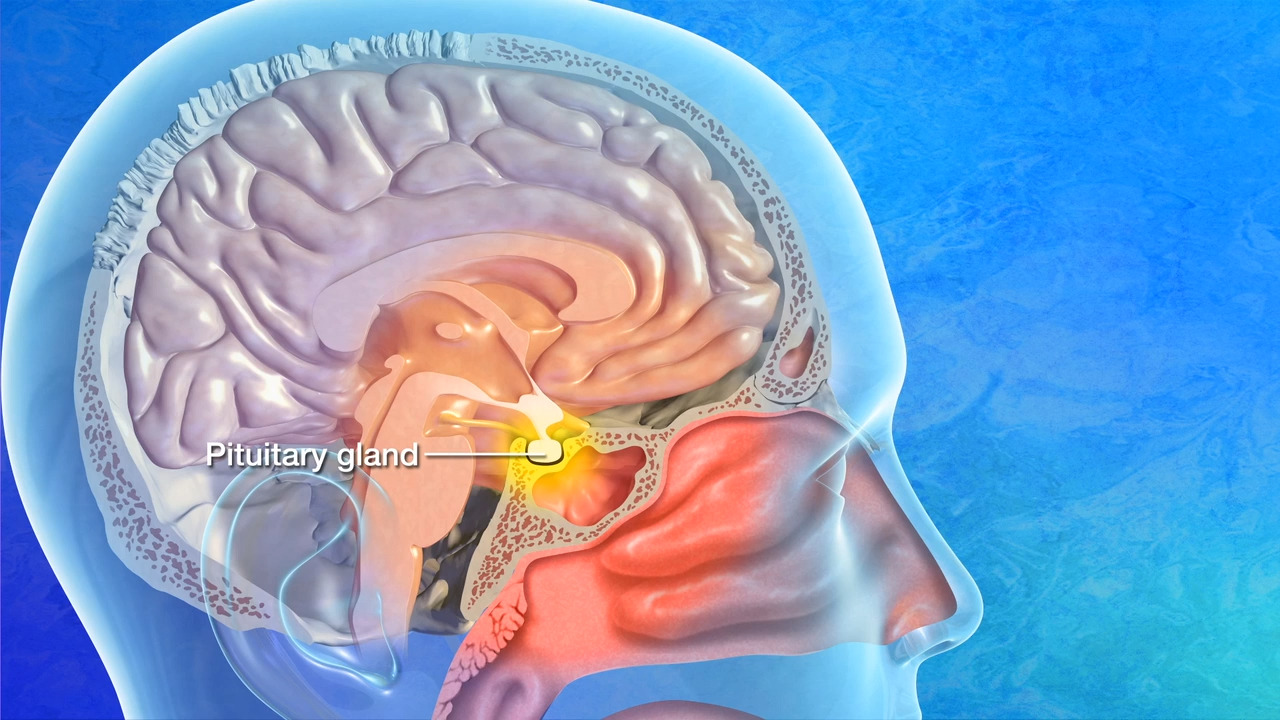
Causes of Acromegaly
Acromegaly is most commonly caused by a benign tumor on the pituitary gland called a GH-secreting pituitary adenoma. These tumors cause the pituitary gland to secrete a surplus of GH, which stimulates the liver to produce excessive IGF-1.
As an adult, too much GH and IGF-1 can lead to irregularly shaped bones, increased organ size, high blood pressure, and elevated blood sugar levels, among other symptoms. Although rare, acromegaly can also be caused by tumors of the pancreas, lungs, or other parts of the brain stimulating the pituitary gland. Once the growth plates in your bones have fused as an adult, your body still needs your pituitary gland to produce growth hormone. While its release no longer increases your height, GH helps your body maintain normal bone, brain, cartilage, organ structure, and metabolism.

Acromegaly Symptoms
Acromegaly symptoms can be difficult to pinpoint, because they accumulate slowly over time. For example, people might only notice their hands have grown once the rings they regularly wear feel unusually tight, or their shoe size changes seemingly out of the blue.
If you’re feeling concerned by any of the symptoms below, it’s crucial you reach out to your healthcare provider to seek out an appropriate diagnosis.

These are some of the symptoms you might notice if you or someone you know has acromegaly:
- Enlarged hands and feet: Your hands and feet may grow out of proportion with the rest of your body.
- Thickening of facial features: Your jaw, nose, and lips may become more pronounced.
- Headaches: Due to pressure from the tumor, frequent headaches can occur.
- Oily skin and excessive sweating: The over-secretion of glands as they increase in size and density causes both symptoms.
- Fatigue and depression: An unusual onset of either symptom can point to acromegaly’s hormonal and physical changes.
- Heart disease and heart enlargement: Long-term excess GH and IGF-1 can lead to the development of a heart disorder.
- Vision problems or loss of vision: If the tumor on your pituitary gland presses against nearby nerves, it can affect your vision.
- Hypertension: High blood pressure can also be an indicator of acromegaly.
- Diabetes: New onset of diabetes may also be a cause of acromegaly.
- Impotence and loss of libido
- Interrupted menstrual cycle
- New onset of sleep apnea
- New onset of carpal tunnel syndrome or arthritis
- Chronic headaches and worsening joint pains

Acromegaly Diagnosis
The diagnosis of acromegaly is confirmed with elevated GH and IGF-1 levels in your blood. This is the most common method of diagnosis and typically involves one or two tests done together:
- IGF test. While levels of GH in the blood fluctuate throughout the day, a predictable way to track GH is by measuring the level of IGF-1 in the blood. In most adults, a high IGF-1 level will suggest an acromegaly diagnosis.
- Oral glucose tolerance test. To confirm this diagnosis, an oral glucose tolerance test can be ordered. After an overnight fast, a sugary liquid is ingested, then a medical professional will test your blood every half hour for 2 hours to measure GH levels. Typically, the drink’s high sugar content will cause GH levels to fall, but when too much GH is being made, these levels do not decrease appropriately, which confirms the acromegaly diagnosis.
Acromegaly may also be suspected if you or your healthcare provider notice amplified growth in your body or see abnormal bone growth, disproportionately enlarged organs, or a tumor on the pituitary gland via magnetic resonance imaging (MRI).
Once you’ve been diagnosed with acromegaly, additional tests may be ordered to see if the condition has affected other areas of your body. These tests may include an echocardiogram to check for heart issues, a colonoscopy to determine colon health, a sleep study to check for sleep apnea, and X-rays or a DEXA scan to monitor bone health.
Acromegaly Treatment
Most commonly caused by a noncancerous tumor of the pituitary gland (pituitary adenoma), acromegaly is often cured with surgery. Whether or not the entire tumor can be removed depends on its size and if it’s grown into nearby organ or tissue structures.
The goal of acromegaly treatment is to control tumor size, normalize GH and IGF-1 levels, improve symptoms, and prevent complications.
Neurosurgery
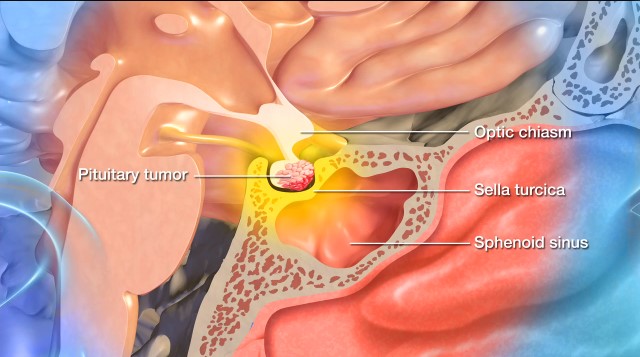
An operation by an experienced pituitary neurosurgeon is the first line of treatment and the only method for reaching a true cure for acromegaly. Your neurosurgeon will access the pituitary gland using the transsphenoidal approach, so named because the neurosurgeon uses the sphenoid sinus behind the nose for the procedure.
Using precise instruments, your neurosurgeon will enter the nasal cavity and create an opening in the sphenoid bone. Further openings will be made until a hole is created in the sella turcica, the bone that cradles and protects the pituitary gland.
Once the tumor appears in the operative field, your neurosurgeon will use high magnification to help distinguish the tumor from normal pituitary tissue. When the tumor has been removed, the tumor cavity is cleaned and sealed off. Barrow neurosurgeons do not make external incisions on the face and bruising is uncommon. In fact, most patients can return home the day after their surgery.
At Barrow Neurological Institute, our surgeons specialize in endoscopic pituitary surgery. Endoscopic pituitary surgery uses a tiny camera to enter the nostrils to remove the tumor. This method of surgery aims to minimize trauma to the tissue surrounding the pituitary gland while facilitating a speedy recovery with as little discomfort or pain as possible.
Pharmacological Treatment and Hormone Therapy
Treatment with prescription medication is possible if surgery does not cause remission in your acromegaly or if surgery is not recommended due to other reasons specific. Medicines are also sometimes prescribed prior to surgery to improve the likelihood of a good outcome.
- Octreotide or lanreotide are the two synthetic forms of the hormone somatostatin that stops GH release. These medications are often effective for the long-term control of acromegaly, but can only be administered by a large injection every four weeks. Due to the side effects of these drugs as well as their expense, surgery is generally preferred.
- Oral octreotide is a recently approved oral medication that can be used after being on injectable octreotide or lanreotide. This medication needs to be taken twice a day without food and has been shown to normalize IGF-1 levels just as effectively as injectable octreotide or lanreotide.
- Bromocriptine and cabergoline are from a class of drugs called dopamine agonists. They can lower IGF-1 and GH levels especially if the IGF-1 level is mildly elevated. Although not as effective as the synthetic hormones octreotide and lanreotide, they’re less expensive and more convenient to administer orally as opposed to an injection. They can be combined with octreotide in some people with no adverse long-term health effects.
- Pegvisomant is a drug that blocks the action of GH at the level of GH receptors in various parts of the body, thereby lowering IGF-1 levels. It must be administered daily by subcutaneous or beneath-the-skin injection. Pegvisomant is an option if you don’t respond to surgery or other medications.
Radiosurgery for Acromegaly
Gamma Knife radiosurgery is a highly advanced form of accurate radiation therapy that achieves results similar to those in the surgical techniques described above.
The ‘knife’ in this surgery is made up of many small beams of radiation focused on a very specific single point at the base of the skull where the pituitary gland resides. Each beam is too weak to damage healthy tissue, but at the point where the beams converge, they deliver a dose of radiation that’s lethal to the tumor.
Gamma Knife is an outpatient procedure, does not involve any incisions, and requires only brief sedation under general anesthetic. However, it can take several years for GH levels to return to normal using the Gamma Knife rather than the days or weeks with traditional surgery. As a result, Gamma Knife is often a last resort treatment for acromegaly after surgery and medications.
Common Questions
How common is acromegaly?
Acromegaly continues to be rare, with an incidence rate of 10 new cases per year for every 1,000,000 people.
The condition affects adults only and most commonly occurs between the ages of 30 and 50 years old, with the average age being 44 years old. Patients who are diagnosed at a younger age tend to experience a more aggressive form of acromegaly. In recent years, there are several genes that have been described to be responsible for the development of acromegaly in younger adults.
What is the difference between gigantism and acromegaly?
Acromegaly and gigantism are both conditions that are a direct result of excess GH. The difference between the two conditions is who they affect: children and adolescents who are still growing develop gigantism, while adults who are finished growing and have their growth plates fused develop acromegaly.
Acromegaly is more common than gigantism.
What is the prognosis for those diagnosed with acromegaly?
Many diagnosed with acromegaly can vastly improve with treatment, even if the condition is not considered cured.
The prognosis for acromegaly depends on whether surgery can remove the entirety of the tumor and whether medications can induce remission if the surgery does not succeed in removing the entire tumor. Patients whose GH and IGF-1 levels fall to normal generally have a normal life expectancy.
Can acromegaly be prevented?
Although early diagnosis is crucial, there aren’t any preventative measures for acromegaly. That said, prompt treatment—generally in the form of surgery—can prevent or slow the excessive growth changes that acromegaly can cause.
Information and Resources
References
- Kimball A, Dichtel LE, Yuen KCJ, Woodmansee WW, Haines MS, Nachtigall LB, Swearingen B, Jones P, Tritos NA, Sharpless JL, Kaiser UB, Gerweck A, Miller KK. Quality of life after long-term biochemical control of acromegaly. Pituitary. 2022 Jun;25(3):531-539. doi: 10.1007/s11102-022-01224-0. Epub 2022 Apr 27. PMID: 35476257; PMCID: PMC10080999.
- Bove I, Cheok SK, Feng JJ, Briggs RG, Ruzevick J, Cote DJ, Shah I, Little A, Laws E, Castro AV, Carmichael J, Shiroishi M, Hurth K, Zada G. Clinical Implications of Pituitary Adenomas Exhibiting Dual Transcription Factor Staining: A Case Series of 27 Patients. World Neurosurg. 2024 Feb;182:e62-e66. doi: 10.1016/j.wneu.2023.11.036. Epub 2023 Nov 14. PMID: 37967742; PMCID: PMC11032010.
- Yuen KCJ, Samson SL. Oral Octreotide: A Review of Recent Clinical Trials and Practical Recommendations for Its Use in the Treatment of Patients With Acromegaly. Endocr Pract. 2022 Jun;28(6):637-645. doi: 10.1016/j.eprac.2022.04.009. Epub 2022 Apr 19. PMID: 35452815.
- Yuen KCJ, Munoz KA, Brook RA, Beren IA, Whalen JD, Rohrbacker NJ, Ribeiro-Oliveira A Jr. Health Benefit Costs and Absenteeism Among Employed Patients With Acromegaly. Endocr Pract. 2021 Oct;27(10):1034-1039. doi: 10.1016/j.eprac.2021.04.412. Epub 2021 May 1. PMID: 33940182.
- Ribeiro-Oliveira A Jr, Brook RA, Munoz KA, Beren IA, Whalen JD, Kleinman NL, Yuen KCJ. Burden of acromegaly in the United States: increased health services utilization, location of care, and costs of care. J Med Econ. 2021 Jan-Dec;24(1):432-439. doi: 10.1080/13696998.2021.1898968. PMID: 33663311.