Herniated Disc
Herniated Disc Overview
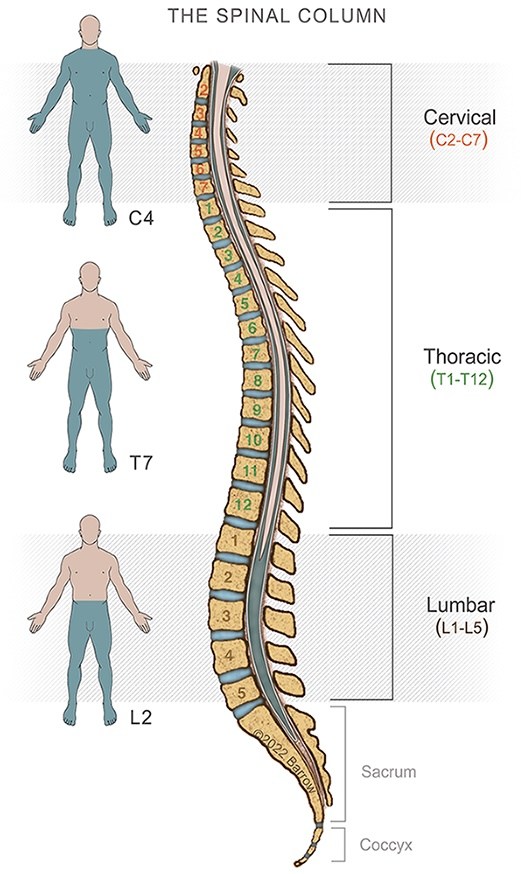
Made up of 24 bones called vertebrae, the adult spine is also home to 23 discs between each vertebra that act as shock absorbers when the spine moves and bends. Inside each disc is a soft, jelly-like center called the nucleus pulposus, while on the outside, a tough layer called the annulus fibrosus protects the spongy center.
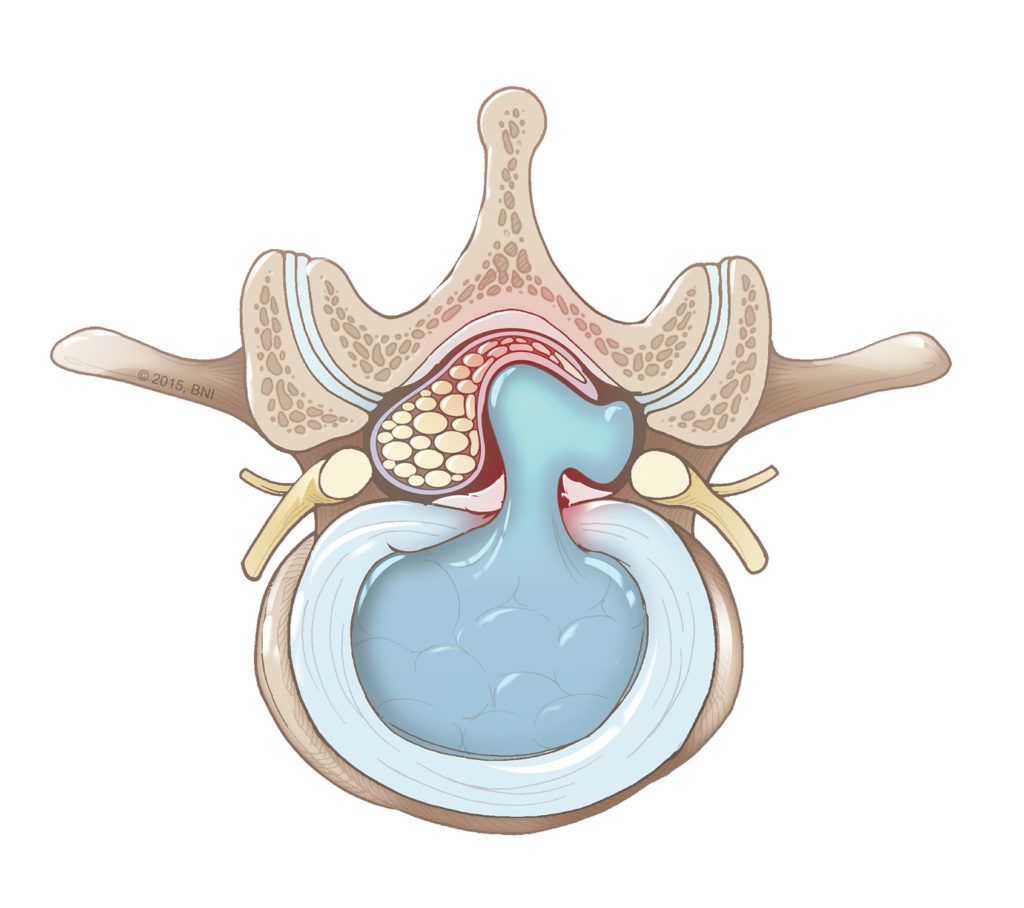
When the soft center of a disc pushes through a tear in the outer layer, a herniated disc occurs. If the protruding disc fragment then puts pressure on the spinal cord (cervical or thoracic herniation), it can cause back pain and spinal cord dysfunction. If it’s in the lumbar spine, it can cause nerve root compression and sciatica. The disc fragment also releases chemical irritants that can lead to inflammation.
Also known as a slipped disc or ruptured disc, a herniated disc can happen in any part of the spine. Discs can tear due to injury, degeneration due to aging, or a combination of the two. A herniated disc is most common in the lower back or lumbar spine, followed by the neck or cervical spine. Herniated discs are least common in the middle part of your back, known as the thoracic spine.
The size of the herniated disc does not necessarily correlate to the intensity of symptoms. For example, a large herniation may not cause much pain if a nerve root is unaffected. Meanwhile, a small disc herniation can cause significant discomfort if a nerve root is severely compressed or inflamed.

Herniated Disc Causes
Numerous factors can contribute to a herniated disc, including:
- Age-related changes: As people age, the discs in the spine naturally lose water content, becoming less flexible and more prone to tearing or rupturing with even minor stress or strain.
- Genetic predisposition: Some people are more prone to disc herniation due to inherited disc traits or spine anatomy. Genes involved in collagen formation, disc degeneration processes, and inflammatory response have also been linked to an increased risk.
- Traumatic injury: Sudden trauma from accidents, falls, or blows to the back can cause a disc to rupture or herniate.
- Physical activity and occupational hazards: Heavy lifting or repetitive motion can strain or stress the spine, increasing the risk of a herniated disc. So, too, can jobs that involve heavy lifting, repetitive motions, and prolonged sitting.
- Lifestyle factors: A sedentary lifestyle can weaken the muscles that support the spine, making it more susceptible to injury. Being categorically obese also puts extra stress on the spine, and smoking reduces blood flow to spinal discs, leading to degeneration and susceptibility to herniation.
- Poor posture: Sitting or standing with poor posture can place extra pressure on the spine, leading to disc degeneration and herniation.
Herniated Disc Symptoms
The symptoms of a herniated disc vary. If the disc isn’t pressing on a nerve, symptoms might be limited to a minor aches or no symptoms at all. If the disc is pressing on a nerve, there’s often pain, numbness, or weakness in the area of the body where the nerve travels.
The symptoms you might notice if you or someone you know has a herniated disc in the lower back or lumbar spine may include:
- Lower back pain: Pain at the site of the herniated disc happens due to the displaced disc fragment pressing on spinal nerves and causing pain.
- Sciatic nerve pain: A sharp, shooting pain that radiates from your buttocks down the leg that can occur due to pressure on the spinal nerve.
- Weakness in the leg or foot: This results from the herniated disc pressing on a nerve that travels down to one leg or foot.
- Bowel and bladder dysfunction: Though rare, compression of the spinal nerve roots can cause bowel and bladder issues and calls for prompt medical attention.
Symptoms of a herniated disc in the neck or cervical spine can include:
- Dull or sharp pain in the neck or between the shoulder blades: Herniated discs in the neck can extend to the shoulder and arm, and the resulting pain can feel sharp or burning.
- Neck pain that increases with movement: Movements involving the extension or rotation of the neck can aggravate nerve compression because they change the position of the vertebrae and discs, potentially increasing pressure on the area.
- Neck pain that radiates down the arm to the hand: Nerve root irritation in the cervical spine can produce referred pain or pain felt in the areas served by the affected nerves, such as the shoulders, arms, or hands.
- Numbness or tingling in a shoulder or arm: A herniated disc in this part of the spine can induce numbness and tingling that radiates to a nearby limb.
Symptoms of a herniated thoracic disc may include:
- Difficulty walking: The compression of the spinal cord in the thoracic spine can lead to motor and sensory deficits, manifesting as leg weakness, balance issues, and pain, impairing walking ability.
- Pain in the mid back, which may wrap around the chest: The pain from a compressed spinal nerve in the thoracic spine may be more severe, as the spinal canal in this part of the spine is smaller than the other two regions.
- Progressive weakness and numbness in lower extremities: A herniated disc in the thoracic spine can cause progressive weakness and numbness due to the compression of the spinal cord and the nerves that branch off from it.
- Bowel and bladder dysfunction: Compression of the spinal cord or nerve roots can disrupt the nerves that control bladder and bowel functions.
Discomfort from a herniated disk usually worsens when you’re active and lessens when you’re resting. Certain positions or activities, like twisting your spine, bending forward at your waist, sitting for a prolonged time, or lifting too-heavy objects, can cause additional inflammation or compression of the affected nerve.
To help alleviate your symptoms, the following positions can help:
- Sitting in a reclined position
- Lying on your side or back with a pillow between or under your knees
- Lying flat on your back with your hips and knees at 90 degrees
For some people, continuing to engage in non-strenuous activity or taking short walks can reduce the likelihood of pain.

Herniated Disc Diagnosis
A physical exam can be sufficient to diagnose a herniated disc. More detailed diagnostics, such as MRI, are necessary to identify the precise location and the structures affected and to aid in surgical planning.
Your doctor may use some or all of the following:
- Medical review and neurological exam: First, your healthcare provider will ask about your symptoms, overall health, and family history. Next, they’ll test your reflexes, muscle strength, walking ability, and response to sensory stimuli.
- Physical exam: A simple straight leg raise test can often indicate a herniated disc. While on your back, your provider will help you raise your symptomatic leg without bending it. If this triggers pain in the raised leg or increases pain, irritation or sciatic nerve compression is inferred.
- Crossed straight leg test. Also called the “well leg” raise test, this is a variation of the straight leg raise test that involves raising the leg without painful symptoms. If raising this leg creates pain in the non-raised leg, it can indicate irritation or compression of a sciatic nerve root.
- Lumbar spine exam. This involves a range of motion testing while bending backward, forward, and in a spinal rotation. Your standing and sitting postures are also evaluated.
- Magnetic Resonance Imaging (MRI): Imaging studies are crucial in visualizing the spinal cord or spinal nerves and identifying abnormalities. An MRI provides images that can locate the position of the herniated disc and determine which nerves are affected. An MRI can also help rule out non-spine-related causes of pain.
- Computed Tomography (CT) scan: A CT scan takes multiple X-rays from different angles and combines them to create images of your spine and its surrounding structures. However, CT scans aren’t relied on as heavily in diagnosis since disc herniation isn’t visible on an X-ray.
- Electrodiagnostic tests: Although less common, your doctor may enlist these tests to determine if any nerves in your spine are damaged or compressed. Electromyography (EMG) involves a small needle electrode inserted into the muscle to record the electrical activity of your muscles at rest and while they contract. A Nerve Conduction Study (NCS) evaluates a nerve’s ability to send signals along the nerve or to the muscles.
Using simple tests, combined with diagnostic tools when needed, leads to the proper diagnosis and helps your healthcare team create a tailored treatment plan for you.
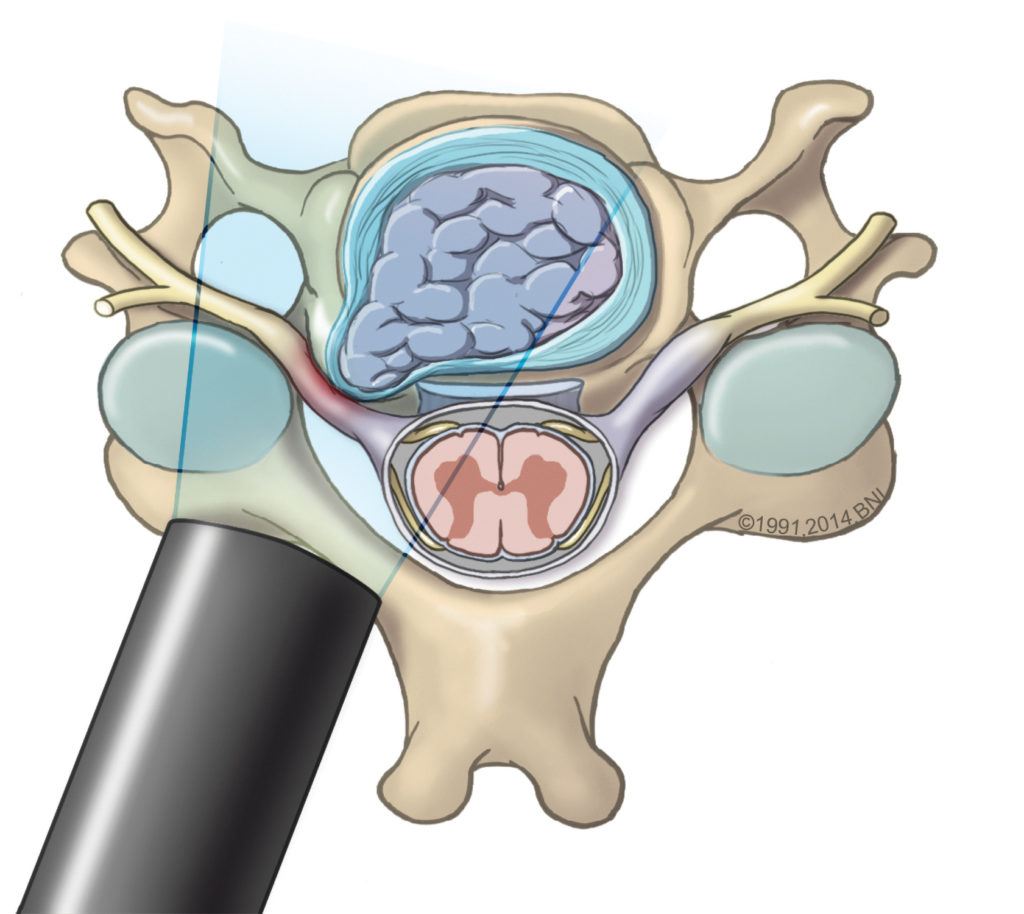
This illustration depicts a herniated disc in the cervical spine putting pressure on a spinal nerve root. It also shows the placement of a tube used during minimally invasive spine surgery.
Herniated Disc Treatments
Herniated disc treatment typically involves a combination of self-care, medications, decreased activity, and physical therapy. If these more conservative treatments fail, your doctor might prescribe epidural blocks. In some cases, you may need spine surgery.
Your specific treatment plan will depend on your symptoms’ severity and overall health. That said, most treatments involve lifestyle changes and incorporating exercise-based therapies to maximize healing and minimize the odds of reoccurrence.
Non-Surgical Treatment
The good news is that most herniated discs don’t require surgery. After diagnosis, doctors will often prescribe a conservative treatment plan of rest and a reduced activity level, anti-inflammatory medication, and physical therapy.
One to two days of bed rest can help relieve back and leg pain. However, it’s not recommended to rest longer than that—prolonged bed rest can lead to muscle stiffness and weakness.
As activity is gradually resumed, it’s best to take the following precautions:
- Be mindful of resting throughout the day, but avoid sitting for long periods
- Keep physical activity slow and steady, especially when bending or lifting
- Avoid movements that may cause further pain
In addition to initial rest and caution with movements, the following therapies are often recommended:
- Physical therapy: Generally focused on movements and stabilization to reduce nerve compression, physical therapy can include exercises to increase flexibility and strengthen the muscles supporting the spine, ultrasound techniques, and electrical muscle stimulation. Pain medication and muscle relaxants can be combined with physical therapy to minimize discomfort.
- Massage therapy: Deep tissue or neuromuscular massage therapy can help relieve muscle spasms, relax tight muscles, and promote healing. A bonus is the pain-relieving endorphins released during and after massage.
- Spinal manipulation: Chiropractic adjustments or osteopathic manipulations can relieve pain and improve function in the back or leg in the event of sciatica.
- Hot and cold therapy: While heat relaxes tight muscles, increases blood flow, and reduces spasms, applying ice or cold packs will reduce inflammation and relieve pain.
- Acupuncture: Inserting hair-thin needles into specific areas of the skin stimulates the nerves affected by a herniated disc, reducing symptoms.
- Injection treatments: If rest, pain relievers, and physical therapy aren’t providing relief, your doctor might suggest an injectable steroid like cortisone. Known as an epidural injection, the steroid injected into the space around your spinal nerve can help ease pain and help bring down swelling, which leads to greater mobility.
If your herniated disc symptoms persist for more than four weeks, your doctor may refer you to a spine surgeon.

Surgical Treatment
If herniated disc pain continues to affect your quality of life and is not relieved by therapies, your spine surgeon might recommend surgery.
Only a small percentage of patients with a herniated disc require surgery, but your doctor may recommend it if enough time has passed to determine if non-surgical treatments are effective, or if you’re experiencing any of the following:
- Pain is impairing your quality of life
- Progressive leg weakness or numbness develops
- Normal bowel and bladder functions are affected
- Standing or walking remains difficult
The two most common surgical procedures for a herniated disc include a discectomy and a microdiscectomy. While both procedures remove the herniated portion of the disc to relieve pressure on the nerve, they differ in their procedural protocol and recovery time:
- Discectomy: In a traditional discectomy, your neurosurgeon will make a larger incision in the back or neck to access the spine and remove part or all of the herniated disc (cervical spine) part of the disc (lumbar and thoracic). Using direct visualization of your spinal structures, your neurosurgeon will need to retract your muscles and tissues more extensively, and recovery may take longer due to the more extensive tissue manipulation.
- Minimally invasive discectomy (microdiscectomy): A minimally invasive discectomy, or microdiscectomy, is done through a small incision at the site of the disc herniation, frequently through specialized dilation tubes and a microscope. It is usually an outpatient surgery. In this procedure, your neurosurgeon will remove the protruding fragment of the disc that’s compressing the spinal cord or spinal nerves. This minimally invasive approach leads to less tissue damage, less blood loss, and fewer cases of postoperative infection at the surgical site.
At Barrow Neurological Institute, our spinal surgeons are leaders in minimally invasive techniques for disc herniation and employ highly specialized instruments to operate through smaller incisions. Benefits of minimally invasive surgery at Barrow include:
- A shorter hospital stay
- Less postoperative pain
- Reduced blood loss
- Faster recovery
It’s important to discuss the advantages of surgical and non-surgical treatments with your healthcare provider, as every surgical procedure carries risks. Known risks for herniated disc surgical treatment include bleeding, infection, nerve injury, or a tear in the sac covering the nerves (known as a dural tear).
Common Questions
How common are herniated discs?
Herniated discs are relatively common, especially as people age. Studies suggest that two to three percent of the general adult population will experience the symptoms of a herniated disc at some point.
The most common cause of disc herniation is disc degeneration, a natural effect of aging. Degeneration reduces the disc’s ability to act as a shock absorber, making the outer ring, known as the annulus fibrosis, more likely to tear under pressure.
The second most common cause is a sudden injury to the disc, such as improperly lifting a heavy object or excessively twisting the lower back. This causes an immediate tear in the outer layer (annulus fibrosis) and a herniation of the disc’s inner core (nucleus pulposus).
The vast majority of herniated discs, about 95 percent, occur in the lumbar spine. Roughly five percent occur in the cervical spine, and less than one percent occur in the thoracic spine.
Who gets herniated discs?
While a herniated disc can happen to anyone, people between 30 and 50 are most likely to experience one due to the spine’s natural aging process. As we age, our intervertebral discs can lose their cushioning and become more susceptible to rupture.
Additionally, herniated discs happen more often in men than women. Research has also shown that herniated discs can run in families, meaning a genetic predisposition may leave certain parts of the population more vulnerable than others.
What is the prognosis for people with a herniated disc?
The prognosis for people with a herniated disc is good, as most heal with time, rest, and over-the-counter anti-inflammatory medicine. Pain and related symptoms typically improve as the inflammation from the injury decreases and the body begins to heal the herniation.
Other factors that will influence prognosis include:
- Overall age and general health: Being younger and in good health usually predicts a quicker and more comprehensive recovery.
- Severity and location: A herniation without significant nerve compression generally has a better prognosis, while a herniation in the lumbar spine often improves faster than one in the cervical spine.
- Response to treatment: Patients who respond well to more conservative treatments typically have a better prognosis.
Physical therapy can also reduce pain, improve alignment and posture, and build supportive muscles around the injury. When pain from a herniated disc does not resolve, more potent pain relief medications and muscle relaxants may be prescribed, or a steroid shot may be administered to help bring down swelling and ease pain.
For severe disc herniation cases where daily movement is severely restricted or there’s a concern of spinal compression, your doctor may advise surgery.
Can herniated discs be prevented?
While it’s not always possible to prevent a herniated disc—primarily due to factors like aging and genetics—there are several steps you can take to reduce your risk. They include:
- Engaging in regular exercise, including strengthening exercises, flexibility exercises, and aerobic activities, like walking, jogging, swimming, and cycling.
- Maintaining good posture, whether sitting or standing, and using ergonomic furniture to support your spine.
- Maintaining a healthy weight through a balanced diet will reduce the strain on your spine and lower back.
- Regularly stretching, changing positions, or walking briefly to avoid being sedentary for too long.
- Using supported postures when bending, lifting, pulling, or twisting.
- Avoiding or quitting smoking, as smoking can reduce blood flow to discs and lead to degeneration.
Together, these measures protect the integrity of your spinal discs while encouraging the flow of healthy nutrients into them.
Resources
References
- Farber SH, Walker CT, Zhou JJ, Godzik J, Gandhi SV, de Andrada Pereira B, Koffie RM, Xu DS, Sciubba DM, Shin JH, Steinmetz MP, Wang MY, Shaffrey CI, Kanter AS, Yen CP, Chou D, Blaskiewicz DJ, Phillips FM, Park P, Mummaneni PV, Fessler RD, Härtl R, Glassman SD, Koski T, Deviren V, Taylor WR, Kakarla UK, Turner JD, Uribe JS. Reliability of a Novel Classification System for Thoracic Disc Herniations. Spine (Phila Pa 1976). 2024 Mar 1;49(5):341-348. doi: 10.1097/BRS.0000000000004701. Epub 2023 May 1. PMID: 37134139.
- Pacult MA, Farber SH, Tumialán LM, Oppenlander ME. Management of cerebrospinal fluid leak after a minimally invasive lumbar decompression procedure: illustrative case. J Neurosurg Case Lessons. 2024 Dec 9;8(24):CASE24497. doi: 10.3171/CASE24497. PMID: 39652849; PMCID: PMC11633019.
- Alan N, Lee KE, Leal Isaza JP, Giraldo JP, Dugan RK, Zhou JJ, Farber SH, O’Neill LK, Uribe JS. Outpatient lateral lumbar interbody fusion: single-institution consecutive case series. J Neurosurg Spine. 2024 Nov 29:1-7. doi: 10.3171/2024.7.SPINE231041. Epub ahead of print. PMID: 39612502.