
Astrocytoma
Astrocytoma Overview
Astrocytomas are a type of glioma, or tumor that forms from the glial cells in the brain or spinal cord. Glial cells are considered nervous system “helpers” because they provide protection and nutrients to the neurons, the cells responsible for sending and receiving messages in the central and peripheral nervous system.
Specifically, astrocytomas come from astrocytes, or the star-shaped glial cells that nourish and support neurons. An astrocytoma consists of mutated or damaged astrocytes that can no longer support neurons and lose their ability to grow in an organized way. This unchecked growth damages the surrounding brain or spinal cord structures and causes symptoms of an astrocytoma.
Astrocytoma Classification
The World Health Organization (WHO) grades astrocytomas on a scale ranging from grade 1, the least aggressive, to grade 4, the most aggressive. Low-grade astrocytomas grow slowly and may not cause many symptoms initially, but they still require monitoring and occasional treatment. High-grade astrocytomas grow quickly and often call for more aggressive treatment.
- Grade 1 astrocytomas usually do not infiltrate or mix with surrounding tissues. Although they’re slow-growing, they can become quite large. The most common Grade 1 type is a pilocytic astrocytoma, and these grades of astrocytomas are most common in children, teens, and young adults.
- Grade 2 astrocytomas are also called low-grade or diffuse astrocytomas. Because they can mix with surrounding structures, it can be challenging to see a clear boundary between the tumor and normal brain tissue. These astrocytomas grow slowly and occur most often in adults between 20 and 40.
- Grade 3 astrocytomas, also known as anaplastic astrocytomas, grow faster than Grade II astrocytomas. They are more challenging to treat because their tentacle-like fingers can develop into nearby brain tissue. Anaplastic astrocytomas are most common in adults between 30 and 50.
- Grade 4 astrocytomas, also called glioblastomas or glioblastoma multiforme (GBM), are the most common. More than 50 percent of astrocytomas are glioblastomas. Of all astrocytomas, these grow the fastest and aggressively invade surrounding tissues. They’re more common in men and most common in adults between 50 and 80, with the average age at diagnosis being 64.
Although diagnostic imaging can suggest the type of tumor you have, only a biopsy of tissue taken from the tumor can conclusively determine your tumor’s classification.
What causes an astrocytoma?
The exact cause of an astrocytoma is not fully understood, but several factors can contribute to their development:
- Cellular processes: Disruptions in normal cellular processes, like cell cycle regulation and DNA repair mechanisms, can contribute to tumor growth. So, too, do changes in the regulation of gene expression, like DNA methylation.
- Genetic mutations: Mutations to specific genes, such as TP53, TERT, EGFR, IDH1, IDH2, and ATRX, have been linked to astrocytoma development. These mutations can disrupt normal cell growth and division, leading to the uncontrolled growth of cancer cells.
- Inherited genetic conditions Some astrocytomas and other types of brain tumors have been linked to rare and inherited genetic conditions, like neurofibromatosis type I, Turcot syndrome, Lynch syndrome, or Li-Fraumeni syndrome.
- Age: Astrocytomas can occur at any age, but pilocytic astrocytomas are more common in children and younger adults. Meanwhile, diffuse astrocytomas and glioblastomas are more common in adults.
- Gender: Glioblastomas are slightly more common in males than females.
- Environmental factors: One of the few established environmental risk factors is exposure to high doses of ionizing radiation, such as radiation therapy from other cancers.
- Cellular processes: Disruptions in normal cellular processes, like cell cycle regulation and DNA repair mechanisms, can contribute to tumor growth. So, too, do changes in the regulation of gene expression, like DNA methylation.

Astrocytoma Symptoms
The symptoms of an astrocytoma depend on the location and size of the tumor. Symptoms of grade 1 and grade 2 astrocytomas are usually subtle, as the brain is temporarily able to adapt to the slow-growing tumor. Symptoms of grade 3 and grade 4 astrocytomas are often the opposite and can be sudden and debilitating.

Symptoms you might notice if you or someone you know has an astrocytoma include:
- Headache: New or worsening headaches that don’t improve with typical remedies or grow in frequency and intensity are a common symptom.
- Nausea and vomiting: Increased pressure inside the skull from the tumor’s aggressive nature can result in nausea and vomiting.
- Vision changes: Vision changes, like partial vision loss or even double vision, can result from an astrocytoma in the temporal lobe, occipital lobe, or brain stem.
- Weakness and coordination problems: A tumor that grows in the brain’s frontal lobe can cause weakness on one side of the body or even paralysis, while those affecting the cerebellum or brainstem can lead to difficulties with coordination or balance.
- Seizure: Seizures can be one of the first signs of an astrocytoma, as the tumor begins to disrupt the brain’s regular electrical activity. Seizures can range from muscle jerks and spasms to a loss of consciousness and body functions. They can also resemble a vision, smell, or sensation change without losing consciousness.

- Cognitive impairment: Changes inmental clarity, alertness, and consciousness, or a change in speech, hearing, or memory, like problems understanding or retrieving words, can be indications of an astrocytoma.
- Fatigue and lethargy: An astrocytoma can cause an increase in the pressure in the skull, which disrupts normal brain tissue and leads to symptoms like fatigue, drowsiness, and lethargy.
- Sensory changes: If the astrocytoma affects sensory pathways in the brain, numbness or tingling sensations can occur in various body parts.
- Personality or behavior changes: These can manifest as new or unusual emotional states, like changes in judgment, aggressiveness, loss of initiative, and even sluggishness. Depression and anxiety, especially sudden onset, can be an early symptom of a brain tumor like an astrocytoma.
Remember that an astrocytoma cannot be diagnosed based on symptoms alone. However, if you or someone you know is experiencing any of these symptoms—especially if they’re persistent or severe—it’s critical to consult a healthcare professional for evaluation. With brain tumors, early detection can improve outcomes.
Diagnosis
Doctors use the following exams and imaging options to diagnose astrocytoma. Generally speaking, magnetic resonance imaging (MRI) is the best method for locating and understanding a brain tumor like astrocytoma. That said, a definitive diagnosis requires the evaluation of a sample of the tumor from a biopsy.
- Physical and neurological exam: First, your healthcare provider will ask about your symptoms, overall health, and any risk factors you might have for an astrocytoma. Next, they’ll complete a neurological examination to assess neurological function, including reflexes, coordination, strength, and sensation.
- Magnetic Resonance Imaging (MRI): An MRI is the primary imaging test to diagnose an astrocytoma. It provides detailed images of the brain and helps identify the tumor’s location, size, and characteristics.
- Computed Tomography (CT): Although an MRI is often the first choice in neuroimaging, a CT scan can help evaluate tumor size and location by relying on X-rays to create detailed cross-sectional brain images.
- Biopsy: Though an astrocytoma may be suspected based on imaging studies alone, a tissue biopsy is needed to determine the tumor type accurately. A biopsy establishes an exact diagnosis by removing a small tissue sample from the tumor surgically or through stereotactic biopsy. Then, pathologists examine the tissue under a microscope to determine the type of cells present, whether they’re cancerous or non-cancerous, and other important characteristics that guide treatment decisions, like grade and genetic mutations.
Specific to Barrow Neurological Institute, our Ivy Brain Tumor Center can help oversee more detailed testing to identify your primary astrocytoma’s subtype—especially if you’ve been diagnosed with glioblastoma. This additional information helps our neurosurgeons and neuro-oncologists be even more precise in selecting treatments and clinical trials.

Astrocytoma Treatments
As with all other facets of a brain tumor, optimal treatment depends on the classification of your astrocytoma, its location, and the severity of your symptoms. The timing of therapy also influences your prognosis—an early diagnosis and surgical intervention are often associated with a better outcome.
Surgical Treatment
The goal of surgery for an astrocytoma is to remove as much cancerous tissue as possible while minimizing damage to surrounding healthy tissue. However, the infiltrative nature of astrocytomas—especially high-grade ones—can make this challenging.
That said, the most common surgical procedures for astrocytomas include:
- Craniotomy: A craniotomy is the most common surgery for a brain tumor. During a craniotomy, a neurosurgeon will make an incision in the scalp, remove a portion of the skull, and access the brain to remove as much of the tumor as safely possible while using intraoperative imaging and highly specialized tools. After the surgical wound has healed, a supplemental treatment—like radiation therapy—can begin.
- Awake Craniotomy: Awake brain surgery, or awake craniotomy, is a specialized surgery for brain tumors in areas that control critical functions, like speech or movement. During awake brain surgery, the patient is awake and alert while the surgeon removes the tumor, allowing the surgical team to monitor brain function in real time and avoid damaging critical anatomy.
At Barrow Neurological Institute, we’ve been early adopters of a surgical method that involves injecting a special dye into the tumor. This dye causes parts of the tumor to glow when placed under fluorescent lighting, increasing the total amount of tumor removed.
Nonsurgical Treatment
Radiation Therapy
Radiation therapy uses precisely aimed beams of radiation to destroy tumors in the body. While it doesn’t remove the tumor, radiation therapy damages the DNA of the tumor cells, which then lose their ability to reproduce and eventually die. It’s typically administered after surgery to target any remaining cancer cells in the brain.

Radiosurgery
Radiosurgery treatment relies on radiation delivery systems to focus radiation at the site of the tumor while minimizing the radiation dose to the rest of the brain. Radiosurgery is often used for tumor recurrence but rarely in initial treatment. The two most common forms are:
Gamma Knife radiosurgery: Using precise and focused radiation beams, this technique destroys abnormal tissue and is only lethal to cells within the immediate vicinity. Gamma Knife is an outpatient procedure that doesn’t involve incisions and requires only brief sedation under general anesthetic.
CyberKnife radiosurgery: This technique uses targeted energy beams to destroy tumor tissue while sparing healthy tissue. It uses image-guided robotics to deliver surgically precise radiation to help destroy tumors.
Chemotherapy
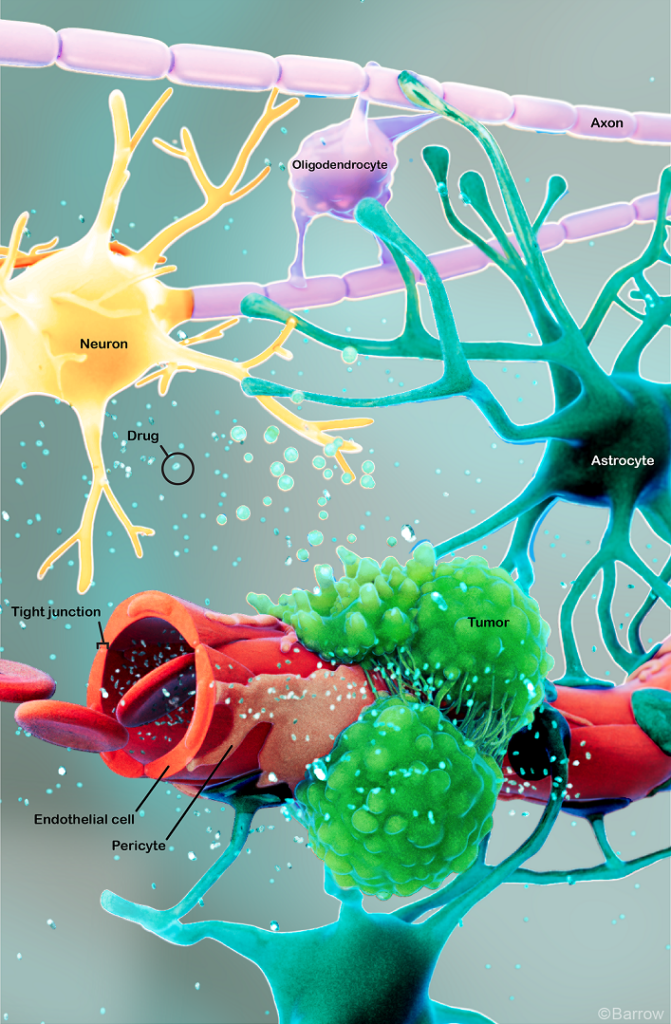
Chemotherapy is often a treatment option for anaplastic astrocytomas (Grade 3) and glioblastomas (Grade 4). It uses drugs given orally or intravenously to stop cancer cells from growing and dividing. For example, glioblastomas (grade 4 astrocytomas) are usually treated with the drug temozolomide. However, it can be challenging for drugs to reach the brain due to the blood-brain barrier, which protects the brain from harmful substances but can also interfere with medicines reaching the brain.
Targeted Therapy
Targeted therapy drugs specifically target cancer cells by interfering with the molecules involved in tumor growth. These drugs can include those that work to target the genetic mutations commonly found in glioma tumor cells, such as BRAF and IDH mutations.
Clinical Trials
Scientists and medical professionals constantly seek new ways to mount better odds against brain tumors, including astrocytomas. In partnership with the Ivy Brain Tumor Center, Barrow Neurological Institute is proud to be one of the country’s largest sites for neurological clinical trials, with a large and active assortment of glioblastoma clinical trials.
One Central Location with Multiple Treatment Options
Surgery for an astrocytoma is most successful when a highly-skilled neurosurgeon does it—and at Barrow Neurological Institute’s world-class Brain and Spine Tumor Program, we treat people with complex tumors in one robust, full-service location. Our sophisticated multidisciplinary team—neurosurgeons, head and neck surgeons, neuro-oncologists, medical oncologists, and radiation oncologists, to name a few—can offer you the latest treatments for head and neck cancers, including neurological and metastatic cancers.
Finally, we also offer a Brain Cancer Survivorship Program to foster relationships between families affected by brain tumors and provide ongoing support.
Neuro-Rehabilitation for Quality of Life
At Barrow Neurological Institute, we give our patients access to various neuro-rehabilitation specialists to maximize independence. Neuro-rehabilitation can include physical therapy to help you regain strength and balance, speech therapy to support speaking, expressing thoughts, or swallowing, and occupational therapy to aid you in managing daily activities like bathing, dressing, and using the bathroom. Treating a brain tumor like an astrocytoma is about more than extending your life—it’s also equally focused on enhancing your quality of life.
Common Questions
How common is astrocytoma?
Astrocytomas are the most common tumors that begin in the brain and the central nervous system.
High-grade astrocytomas are much more common than low-grade ones—unless you are a child under the age of 18—and in the U.S. alone, there are approximately 1,500 new diagnoses of adult astrocytomas every year.
Who gets astrocytoma?
Low-grade astrocytomas are more common in children, teens, and young adults. Meanwhile, high-grade astrocytomas, like glioblastomas, are more common in people over the age of 45.
Overall, astrocytomas are more common in men than in women.
What is the prognosis for people diagnosed with astrocytoma?
The most crucial factor in a brain tumor’s prognosis is its grade. Patients with low-grade astrocytomas often have a favorable prognosis, especially if the tumor is completely removed during surgery and does not progress to a higher grade. Younger patients also tend to have a better prognosis because they respond better to treatment and often recover quickly.
The prognosis for high-grade astrocytomas is generally poor, as it’s a highly invasive and difficult-to-treat type of brain tumor. For those diagnosed with glioblastoma, the most aggressive form of astrocytoma, the median survival time is around 12 to 18 months from the time of diagnosis, even with aggressive treatment. The disease’s five-year survival rate is around 10 percent. However, each patient’s situation is unique, and advances in treatment are continually improving outcomes.
Lastly, how much of the tumor can be safely removed during surgery influences prognosis, too—tumors in easier-to-reach areas of the brain will have a better outcome because more of the tumor can be removed.
Additional Resources
References
- Kurokawa R, Umemura Y, Capizzano A, Kurokawa M, Baba A, Holmes A, Kim J, Ota Y, Srinivasan A, Moritani T. Dynamic susceptibility contrast and diffusion-weighted MRI in posterior fossa pilocytic astrocytoma and medulloblastoma. J Neuroimaging. 2022 May;32(3):511-520. doi: 10.1111/jon.12962. Epub 2022 Jan 7. PMID: 34997668.
- Chang EK, Smith-Cohn MA, Tamrazi B, Ji J, Krieger M, Holdhoff M, Eberhart CG, Margol AS, Cotter JA. IDH-mutant brainstem gliomas in adolescent and young adult patients: Report of three cases and review of the literature. Brain Pathol. 2021 Jul;31(4):e12959. doi: 10.1111/bpa.12959. Epub 2021 May 7. PMID: 33960568; PMCID: PMC8412065.













