Neurofibromatosis and Schwannomatosis
Overview
Neurofibromatosis (NF) involves three distinct genetic disorders caused by mutations on specific chromosomes. Each disorder affects the development of nerve cells and leads to tumors—called neurofibromas—that grow on nerve tissue throughout the body.
Neurofibromas are most often benign, meaning they’re unlikely to spread. What’s more, neurofibromatosis is not a form of cancer: it’s an autosomal dominant genetic condition, although in some cases, the tumors can eventually become cancerous or lead to other complications.
The three genetic disorders that make up neurofibromatosis are:
- Neurofibromatosis Type 1 (NF1): This is the most common form of NF, affecting about 1 in 3,000 people and accounting for nearly 96 percent of all cases. NF1 often causes skin changes, like light brown patches or “café-au-lait spots” and soft, benign tumors under the skin. An NF1 diagnosis can also include learning disabilities, bone deformities, and an increased risk of certain cancers. Gene inheritance from family members with the same condition is most frequently the cause of NF1.
- Neurofibromatosis Type 2 (NF2) Related Schwannomatosis: This condition is much rarer than NF1 and is a subtype of schwannomatosis that affects about 1 in 25,000 people. People with NF2 develop acoustic neuromas (also called vestibular schwannomas), or tumors on the nerves that carry sound and balance information from the inner ear to the brain, meningiomas, and schwannomas. Because of this, NF2 can lead to hearing loss, balance problems, and problems with vision. Approximately 50 percent of affected people inherit the gene for NF2, while in the other half, a spontaneous genetic mutation is the cause.
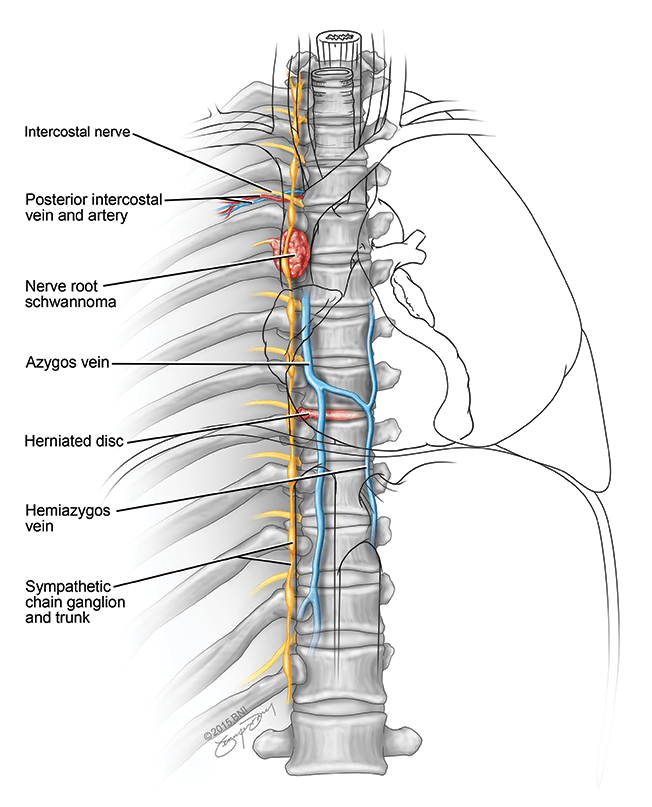
- Schwannomatosis: The rarest form, making up only one percent of overall NF cases, schwannomatosis is genetically distinct from NF1 and NF2. It leads to the development of painful tumors called schwannomas on the peripheral nerves, which relay information between your brain and the rest of your body. Many schwannomatosis cases result from spontaneous mutations without a family history, although some cases can be inherited.
What causes neurofibromatosis?
Mutations in specific genes that control cell growth cause neurofibromatosis. These mutations can be inherited from a parent or occur spontaneously in people without a family history.
In the case of NF1 and NF2, individuals with the disorder have a 50 percent chance of passing it on to their children. About 10 percent of cases are associated with mosaicism, meaning not all cells in the body have a mutation. This occurs due to a mutation in one of (but not all) cells in a dividing embryo. That said, each type of NF is associated with a specific gene mutation, producing different symptoms and tumor growth patterns.
- Neurofibromatosis Type 1 (NF1): NF1 is caused by mutations in the NF1 gene, which produces neurofibromin protein. Neurofibromin helps regulate cell growth and is a tumor suppressor, but its production is disrupted when the NF1 gene is mutated. This leads to an uncontrolled growth of cells along the nerves, creating neurofibromas. If one parent has the NF1 mutation, there’s a 50 percent chance their child will inherit the condition. NF1 can also occur due to a spontaneous mutation in the gene at conception.
- Neurofibromatosis Type 2 (NF2): NF2-related schwannomatosis is caused by mutations in the NF2 gene, which produces a protein called Merlin that helps control cell growth. When the NF2 gene is mutated, the Merlin protein’s ability to regulate cell growth is impaired, leading to tumors on the auditory nerves, as well as tumors along the brain and spinal cord. The most common tumors associated with NF2 include schwannomas, meningiomas, and ependymomas. If one parent has the NF2 mutation, there’s a 50 percent chance their child will inherit the condition. NF2 can also occur due to a spontaneous mutation in the gene, similar to NF1.
- Schwannomatosis: Schwannomatosis is caused by mutations in the SMARCB1 or LZTR1 genes, which are involved in tumor suppression, particularly in the Schwann cells surrounding nerves. When these genes are mutated, Schwann cells can grow abnormally, leading to schwannomas, or tumors that develop on peripheral nerves. Acoustic neuromas—also called vestibular schwannomas—are the most common type of schwannoma and affect the nerves that connect the inner ear to the brain. Meningiomas are also more common in patients with these mutations.

Neurofibromatosis Symptoms
Depending on the type and severity of neurofibromatosis, symptoms can vary greatly. Some people with NF may experience mild symptoms, while others can have serious complications. Ultimately, no two cases of neurofibromatosis are precisely alike.
Some of the symptoms you or someone you know might experience if you have neurofibromatosis type 1 (NF1) can include:
- Skin changes: Light brown patches on the skin called café-au-lait spots, resembling the color of coffee with milk, are present at birth or can appear in childhood. Freckling in skin folds, like the armpits or groin, can also occur.
- Bumps under the skin or skin surface: Neurofibromas can appear as small, soft, skin-colored bumps or larger, deeper lumps that may increase in size over time.
- Eye issues: Lisch nodules, or tiny bumps on the iris, can occur, although they don’t tend to affect vision. However, tumors that grow on the optic nerve can cause vision problems.
- Scoliosis: If you have NF1, scoliosis or the abnormal curvature of your spine is more common and often more severe.
- Cardiovascular complications: Some individuals can develop high blood pressure due to blood vessel narrowing or other complications related to NF1, such as constricted, blocked, or damaged blood vessels.
- Brain tumors: Patients with NF1 have an increased risk of optic and brain gliomas which can cause new neurological symptoms.
- Cognitive challenges: Approximately 50 to 60 percent of children with NF1 experience learning disabilities or cognitive challenges, including difficulties with attention, problem-solving, and executive functioning, along with ADHD (attention deficit hyperactivity disorder).
- Seizures: Due to abnormal activity in the brain, seizures can occur in a small percentage of people with NF1.
Neurofibromas most often appear in children between 10 and 15. However, some signs, like café-au-lait spots, can be present at birth. Children with NF1 are generally shorter than average and can have larger heads.
Some of the symptoms you or someone you know might experience if you have neurofibromatosis type 2 (NF2) can include:
- Tinnitus: The most common symptom of NF2 is ringing in the ears, called tinnitus, due to acoustic neuromas (vestibular schwannomas).
- Hearing loss: Tumors growing on the nerve that sends sound signals to the brain can also affect your hearing ability.
- Balance problems: When a tumor grows on the nerves that control balance and hearing, this can cause problems with coordination, dizziness, or trouble balancing.
- Vision problems: Changes in your retina can affect your vision or cause cataracts to develop earlier, as NF2 tumors can affect the optic nerve.
- Weakness in arms or legs: Peripheral neuropathy can cause numbness or weakness in the arms and legs on one or both sides of the body.
- Bumps under the skin or on the skin surface: Schwannomas, many benign, can also appear as bumps under or on the skin surface.
NF2 symptoms are rare in children and usually appear in those in their late teens or early adulthood.
Some of the symptoms you or someone you know might experience if you have schwannomatosis can include:
- Chronic pain anywhere in the body: Due to the tumors on your nerves, many people with schwannomatosis experience chronic pain.
- Numbness or weakness: In areas where the tumors are pressing on nerves, you can experience numbness, tingling, weakness in your fingers and toes, or even loss of muscle function. Around a third of people with schwannomatosis have tumors limited to a single part of their body, such as an arm, leg, or a segment of the spine.
Schwannomatosis symptoms generally manifest in adulthood, most often after age 30.
Several symptoms of schwannomatosis overlap with those of NF2, as they result from slow-growing schwannomas of the cranial, spinal, and peripheral nerves (and, in some cases, meningiomas in the brain or spinal cord.)
If you or someone you know exhibits persistent or worsening symptoms similar to those outlined above, it is essential to consult with your healthcare provider to discuss the next steps.
Neurofibromatosis Diagnosis
A thorough medical examination, imaging studies, and genetic testing often diagnose neurofibromatosis (NF), although the exact tests and imaging will depend on the specific type of NF.
Doctors often use the following diagnostic tools to diagnose NF:
- Physical and neurological exam: First, your healthcare provider will ask about your symptoms and any risk factors you might have for neurofibromatosis, including family history. Next, they’ll complete a neurological examination to assess your neurological function, including balance, coordination, vision, hearing, and reflexes. Your provider will also examine your skin for symptoms like café-au-lait spots, neurofibromas, and scoliosis.
- Eye exams: In the case of NF1, an eye exam can detect Lisch nodules and optic gliomas. In NF2 diagnoses, they can help identify juvenile cataracts.
- Hearing tests: Audiometry tests may be done to assess hearing loss due to vestibular schwannomas for both NF2 and Schwannomatosis.
- Magnetic Resonance Imaging (MRI): The primary imaging study in neurofibromatosis, an MRI provides detailed images of your brain, spine, and peripheral nerves to help identify tumor location, size, and characteristics.
- Computed Tomography (CT): A CT scan uses X-rays to create detailed cross-sectional images to help evaluate a tumor’s size and location and any possible bone deformities.
- Biopsy: If your imaging results suggest a tumor, a conclusive diagnosis requires a biopsy. A biopsy establishes an exact NF diagnosis by removing a small tissue sample from the tumor; either surgically or through stereotactic biopsy. Then, a neuropathologist examines it under a microscope to determine the type of cells present and whether they’re non-cancerous or cancerous.
- Genetic testing: Genetic testing can help determine the genetic variant causing symptoms. However, genetic testing in schwannomatosis is not always definitive, as not all patients have detectable gene mutations.
- Cancer screening: NF1 increases the chance of breast cancer and women with this condition should start screening by age 30.
An NF1, NF2, or schwannomatosis diagnosis can happen several years after you or your loved one first experience symptoms because symptoms tend to appear gradually. In some cases, a diagnosis is not made until adulthood.

Neurofibromatosis Treatment
While there’s currently no cure for neurofibromatosis (NF), there are numerous treatments to help manage symptoms and possible complications. The best treatment plan for you will depend on the type of NF you’re diagnosed with, the symptoms you’re experiencing, and the severity of your condition.
Surgical Treatments
Surgical removal is typically the primary option for managing neurofibromas, especially when the tumors are quickly progressing, causing structural problems, or unmanageable symptoms. However, not all people diagnosed with NF will need surgery.
For Neurofibromatosis Type 1 (NF1), surgical treatments can include:
- Removal of cutaneous neurofibromas: These benign tumors on or under the skin can be surgically removed for cosmetic reasons or to prevent discomfort. Removal is done under local or general anesthesia, depending on the size and number of tumors. In some cases, laser surgery is a less invasive option for tumor removal.
- Removal of plexiform neurofibromas: These more extensive and complex tumors can grow in deep tissue or around vital structures. Surgical removal aims to reduce tumor size and alleviate symptoms, but complete removal may not be possible.
- Scoliosis surgery: Spinal fusion surgery may be necessary in severe cases of scoliosis to correct spinal deformity. This surgery involves fusing two or more vertebrae to straighten the spine and prevent the curve from worsening, and is especially common in children.
- Tibial dysplasia surgery: In some cases, patients with NF1 develop bone dysplasia, which leads to bone fractures and bowing. Replacing rods or plates to strengthen the bone—or, in severe cases, using bone grafts—can help.
- Orbital or facial bone reconstruction: NF1 can cause abnormal bone development in the face or skull (craniofacial dysplasia), so surgical intervention can prevent complications from bone deformities or correct facial asymmetry.
- Optic pathway glioma (OPG) surgery: While most NF1 optic gliomas are monitored with regular imaging, surgery may be considered if the tumor significantly impacts vision or proliferates. Due to the complexity of the optic nerve, surgery is usually a last resort—treatments like chemotherapy or radiation are often recommended first.
For Neurofibromatosis Type 2 (NF2), surgical treatments can include:
- Acoustic neuroma (vestibular schwannoma surgery): Tumors on the nerve responsible for hearing and balance are a hallmark of NF2, and surgery is often necessary to remove them. Vestibular schwannomas can cause significant hearing loss and balance problems or pose a risk to nearby brain structures. A microsurgical resection is the most common approach, aiming to remove as much of the tumor as possible while preserving facial nerve function and hearing.
- Spinal tumor surgery: Tumors along the spinal cord are common with NF2 and can lead to pain, weakness, or paralysis if they press on your spinal nerves. The most common surgical procedures are tumor resection, laminectomy, or vertebrectomy. A tumor resection aims to remove as much of the tumor as possible while preserving surrounding neurological function; a laminectomy removes part of the vertebral bone, called the lamina, to access and extract the tumor. A vertebrectomy involves spinal fusion to stabilize and reconstruct the spine after removing the vertebra.
- Radiosurgery: This treatment method relies on radiation delivery systems to focus radiation at the site of the tumor while minimizing the radiation dose to the surrounding brain. The two most common forms are:
- Gamma Knife radiosurgery: This option destroys abnormal tissue through radiation beams focused on a precise tissue area and is only lethal to cells within the immediate vicinity. The Gamma Knife can only be used to treat lesions in the head and involves attaching a metal frame to the skull to target beams of radiation accurately.
- CyberKnife radiosurgery: This technique uses targeted energy beams to destroy tumor tissue while sparing healthy tissue. It uses image-guided robotics to deliver surgically precise radiation to help destroy tumors.
- Cochlear implants: If you experience hearing loss after tumor removal, your doctor may recommend cochlear implants.
For Schwannomatosis, surgical treatment includes:
- Schwannoma resection: In schwannomatosis, multiple schwannomas can develop and cause chronic pain, necessitating a surgical resection to remove all or part of the tumor. This peripheral nerve surgery involves careful dissection of the schwannoma from the nerve using microsurgical techniques, and nerve function is monitored using specialized equipment to ensure no nerve damage occurs. Resection typically focuses on areas where the schwannomas are causing significant pain or nerve compression.
Neurofibromatosis is a lifelong condition, and even after surgery, you will likely require follow-up monitoring for recurrence or new growth.
Nonsurgical Treatments
Several nonsurgical treatments are available to help you or your loved one manage symptoms without invasive procedures, particularly in the case of NF1 and NF2.
- Regular monitoring and check-ups: Patients require regular monitoring in all cases of NF. In NF1, regular check-ups help monitor skin growths, bone health, and vision problems. In NF2 or Schwannomatosis, regular MRI scans may be needed to track tumor growth in the brain, spine, and nerves.
- Prescription medications: The U.S. Food and Drug Administration has approved selumetinib as a treatment for people two and older diagnosed with NF1. Selumetinib helps reduce tumor size and alleviate NF1 symptoms such as pain and weakness. For NF2 and other schwannomatosis tumors, bevacizumab inhibits the growth of blood vessels in tumors. It has been shown to reduce the size of vestibular schwannomas and improve hearing. If a tumor is particularly aggressive or has become cancerous, your doctor may recommend more targeted drugs or chemotherapy.
- Pain management: Pain management medications may also be necessary, especially in the case of schwannomatosis. Over-the-counter (OTC) or prescription pain relievers, like nonsteroidal anti-inflammatory drugs (NSAIDs), are used to manage associated pain.
- Blood pressure management: A class of drugs that treats high blood pressure, antihypertensive drugs can be prescribed to manage hypertension in NF1 cases.
- Hearing and vision support: If you’re experiencing hearing loss, hearing aids and other auditory implants may help. Your doctor may also recommend speech therapy or visual aids for vision problems.
- Physical, occupational, and speech therapy: Any of these therapies play a crucial role in managing symptoms related to nerve damage, muscle weakness, or skeletal issues in those with NF.
- Cognitive and behavioral interventions: Many children with NF1 require individualized education plans (IEPs) to address specific learning disabilities. For those with ADHD or other behavioral issues, therapy can help improve attention, focus, and behavior regulation. Meanwhile, cognitive Behavioral Therapy (CBT) can also help manage anxiety or emotional problems related to NF.
Nonsurgical treatments can help improve quality of life, manage symptoms, and even slow the progression of the disease in some cases. Regular follow-up is also essential for long-term care.
One Central Location with Multiple Treatment Options
At Barrow Neurological Institute’s world-class Brain and Spine Tumor Program, we treat people with complex tumors in one robust, full-service location. Our sophisticated multidisciplinary team—neurosurgeons, head and neck surgeons, neuro-oncologists, medical oncologists, and radiation oncologists, to name a few—can offer you the latest treatments for benign and malignant tumors of the head, neck, brain, and spine.
We also give our patients access to various neuro-rehabilitation specialists to enhance their physical abilities, maximize independence, and support their mental health. Neuro-rehabilitation can include physical therapy to help you regain strength and balance, speech therapy to support speaking and expressing thoughts, and occupational therapy to aid in managing daily activities like bathing, dressing, and using the bathroom. Treating a brain or spinal cord tumor is about more than extending your life—it’s also focused on enhancing your quality of life.
Common Questions
How common is neurofibromatosis?
Neurofibromatosis (NF) is one of the most common genetic disorders in the U.S., occurring in about one in every 3,000 births. Collectively, all three types of this genetic disorder affect more than 120,000 Americans.
- Neurofibromatosis Type 1 (NF1): The most common form, NF1, affects around 1 in 3,000 people worldwide.
- Neurofibromatosis Type 2 (NF2): NF2 affects about 1 in 25,000 people globally.
- Schwannomatosis unrelated to NF2: As the rarest form, Schwannomatosis affects around 1 in 40,000 people worldwide.
Who gets neurofibromatosis?
Neurofibromatosis (NF) can affect anyone, regardless of their biological sex, ethnicity, or background. The symptoms often present during childhood, especially for NF1. In contrast, physicians usually diagnose NF2 in young adulthood, typically in the teens or early twenties.
Because genetic mutations cause the disorder, the risk of developing NF depends on whether it’s inherited or occurs due to a new, spontaneous mutation. NF1 is caused by mutations in the NF1 gene on chromosome 17, which helps control cell growth. Mutations in the NF2 gene happen on chromosome 22, which is in charge of a protein called Merlin, which helps regulate nerve cell growth. Although less understood, most cases of schwannomatosis also stem from spontaneous mutations. Some cases are inherited, though the inheritance pattern is believed to differ from both NF1 and NF2
What is the prognosis for those with neurofibromatosis?
The prognosis for neurofibromatosis (NF) depends on the type you have and the severity of your symptoms. While the condition can be unpredictable, an NF1, NF2, or schwannomatosis diagnosis doesn’t usually affect life expectancy.
Many people with NF1 live relatively normal lives through consistent medical care and monitoring. Children do have a higher than average risk of developing a glioma or nervous system tumor. Still, in most cases, these tumors are low-grade and manageable. NF2 and schwannomatosis can be more serious due to the risk of hearing loss, balance issues, and chronic pain, but there are numerous treatments available to help patients manage these symptoms.
Can neurofibromatosis be prevented?
There’s no known way to prevent neurofibromatosis (NF), but you can take the following steps to minimize complications from the condition:
- Genetic counseling: For those with a family history of neurofibromatosis, genetic counseling can be an important preventive step. Since NF is inherited in an autosomal dominant pattern, there’s a 50 percent chance that a parent with NF will pass the gene mutation to their child. Genetic counseling will help you understand the likelihood of passing NF to your children. Prospective parents can also undergo genetic testing to confirm if they carry the NF gene mutation.
- Regular monitoring: Early detection and monitoring of tumors can help manage your symptoms and reduce complications. For example, regular MRI scans, eye exams, and skin evaluations are essential for managing NF1 and NF2.
- Early intervention: Addressing complications like learning disabilities, vision or hearing problems, and bone deformities early can improve quality of life and help manage NF symptoms before they become severe.
- Lifestyle modifications: Prioritizing your well-being through a balanced diet, physical activity, and avoiding prolonged periods of high stress has proven beneficial to a person’s overall health.
Early diagnosis and regular monitoring can help prevent complications associated with neurofibromatosis, improving long-term outcomes.