
Prolactinoma
Overview
A prolactinoma is a benign or noncancerous tumor of the pituitary gland, a pea-sized gland at the base of the brain that makes hormones.
Prolactinomas increase the production of prolactin, which is responsible for milk production, lactation, and certain breast tissue development. As the tumor grows, it can cause very high levels of prolactin in your blood.
Prolactinomas are the most common type of hormone-producing pituitary tumors. Doctors can often treat them with prescription medicines alone. These medications, called cabergoline and bromocriptine, effectively lower prolactin levels and can, in most cases, shrink the tumor. In some exceptional cases, your care team may recommend surgery, radiation therapy, or both.
What causes prolactinoma?
The exact cause of prolactinomas is unknown, but there are several possible causes, like:
- Genetic conditions can increase the risk of developing a prolactinoma, including multiple endocrine neoplasia types one and four and familial isolated pituitary adenomas (FIPAs)
- Mutations in the cells of the pituitary gland, resulting in a large number of cells and causing the production of too much prolactin
Producing too much prolactin (hyperprolactinemia) can also occur for reasons other than a prolactinoma, including:
- Chest wall injuries
- Medications
- Other types of pituitary tumors
- Kidney and liver disease
- Underactive thyroid gland
- Pregnancy and breastfeeding

Prolactinoma Symptoms
In women, prolactinoma symptoms can look like:
- Disruption of menstrual cycle or complete loss of menstruation (amenorrhea)
- Infertility from lack of follicle-stimulating hormone (FSH) and luteinizing hormone
- Milk production not caused by pregnancy or nursing (galactorrhea)
- Breast tenderness
- Headache
- Vision changes (severe cases only)
In men, prolactinoma symptoms can look like:
- Impotence
- Decreased size of testicles
- Decreased beard growth
- Muscle weakness
- Breast enlargement
- Milk production and secretion (galactorrhea)
- Infertility
- Headache
- Vision changes (severe cases only)
It’s possible to have a prolactinoma but not to show any symptoms. Between 5 to 10 percent of adults will fall into this category, although asymptomatic prolactinomas are more common in men than in women.
As a whole, women tend to report their symptoms earlier than men because their symptoms are more outwardly observable—abrupt changes to their menstrual cycle or discharge from their breasts when they’re not pregnant or breastfeeding. But for women who are on hormonal birth control, hormone therapy, or are post-menopausal, these same symptoms might not occur, thus making the reporting of these symptoms less likely.
Prolactinoma Diagnosis
Diagnosing a prolactinoma can be challenging because prolactin levels can be high for reasons besides a tumor—think pregnancy, stress, or a thyroid disorder.
The most common diagnostic tools for prolactinoma involve two procedures:
- Blood Testing. Your doctor can perform a blood test to determine if abnormally high prolactin levels are present. A standard level of prolactin is less than 20 nanograms per milliliter. In comparison, a level of more than 150-200 nanograms per milliliter strongly suggests a prolactinoma.
- Imaging. If your blood test shows elevated levels of prolactin, your doctor will order a magnetic resonance imaging (MRI) scan to determine the location of the tumor in your pituitary region.
After these two procedures, other diagnostic tests may be enlisted, like a visual field test to check for optic nerve compression or a bone densitometry scan to look for evidence of osteoporosis.
Doctors classify prolactinomas by their size. A microprolactinoma is a tumor less than 1 cm in diameter that generally responds to treatment. A macroprolactinoma is a tumor greater than 1 cm in diameter that responds to treatment but may require more aggressive therapy.
What if I’m pregnant and diagnosed with a prolactinoma?
If you’re pregnant and are diagnosed with a prolactinoma, your doctor will carefully monitor the tumor to observe any changes in size. Regular vision tests will also be performed during your pregnancy, as the size of the tumor may increase and impinge on the optic nerves, which connect the eye to the brain, causing visual field defects.
For women who wish to become pregnant and already have a prolactinoma, we encourage you to talk with your provider. Those with a small prolactinoma, or microprolactinoma, can expect a healthy pregnancy. Those with larger prolactinomas, or macroprolactinomas, may need to be treated medically first and followed up closely. In rare cases, it may be advisable to consider surgery before becoming pregnant.
Prolactinoma Treatments
Generally, the first line of treatment for prolactinoma is medical rather than surgical. Whichever treatment your medical team recommends, it will be important to regularly monitor your prolactin levels and the size of your prolactinoma.

Pharmacological Treatment
Prolactinomas are most often treated successfully with prescription medicines alone.
- Cabergoline is a dopamine receptor agonist. It works by inhibiting the cells that produce prolactin and the growth of abnormal prolactinoma cells. Cabergoline is the drug of choice for treating prolactinomas because it causes fewer and less severe side effects than bromocriptine.
- Bromocriptine blocks the production of prolactin by the pituitary gland and may cause your tumor to stop growing or shrink. This medicine is an option if treatment with cabergoline fails, if you don’t tolerate cabergoline, or if cabergoline is not advisable for other reasons.

Neurosurgery
Neurosurgery is the appropriate treatment in the rare event your prolactinoma fails to respond to bromocriptine or cabergoline or if you don’t tolerate these medications.
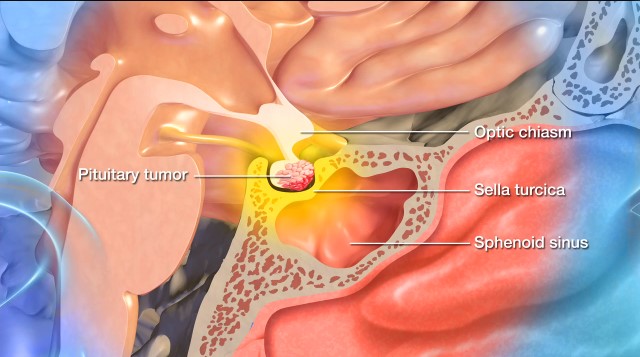
Your neurosurgeon will access the pituitary gland using the transsphenoidal approach through one of your nostrils, so named because the surgeon uses the sphenoid sinus behind the nose for the procedure. This natural opening also makes the procedure less invasive.
Using precise instruments, the neurosurgeon enters the nasal cavity and creates an opening in the sphenoid bone. Further openings create a hole in the sella turcica, the bone that cradles and protects the pituitary gland.
Once the tumor appears in the operative field, removal occurs. Your neurosurgeon will use high magnification to help distinguish the tumor from normal pituitary tissue. After the tumor has been removed, the tumor cavity is cleaned and sealed off.
The surgery aims to minimize pain, discomfort, and trauma to the tissue surrounding your pituitary gland while maximizing your chance for a quick and uneventful recovery. Most prolactinoma patients can return home the day after their surgery.

Radiosurgery
Gamma Knife radiosurgery is a highly advanced form of radiation therapy that can achieve results similar to those in the surgical techniques described above. The ‘knife’ in this surgery consists of many small beams of radiation focused on a single point. Each beam is too weak to damage healthy tissue, but at the point where the beams converge, they deliver a dose of radiation that’s lethal to the tumor.
Pituitary specialists usually reserve the Gamma Knife procedure for prolactinomas that are resistant to medical treatment in people who are not candidates for neurosurgery for reasons like age or other medical conditions. Gamma Knife is an outpatient procedure that does not involve any incisions and requires only brief sedation under general anesthetic. As this form of treatment takes time to work, symptoms can take several years to subside after a person has been treated with Gamma Knife.
Common Questions
How common are prolactinomas?
Small, benign pituitary tumors are relatively common in the general population. Prolactinoma is the most common type of functioning pituitary tumor and makes up nearly 40 percent of all pituitary tumors.
One to three in 10,000 people have a prolactinoma that causes symptoms, and women are five times more likely to experience a prolactinoma than men. However, men are more likely to have a large prolactinoma (macroprolactinoma). In contrast, small prolactinomas (microprolactinomas) are more common in women, as men tend to present themselves to the doctor much later than women.
Prolactinomas most often occur in adults under the age of 40 years, rarely run in families, and are extremely rare in children.
What is the prognosis for those with prolactinomas?
With the proper treatment, the prognosis for those with prolactinoma is very promising.
Medication or surgery generally normalizes prolactin levels, reduces tumor size, and alleviates symptoms. However, to prevent recurrence and monitor for complications, ongoing monitoring of prolactinomas is recommended.
Can a prolactinoma be prevented?
There aren’t any known preventative steps to keep prolactinomas at bay. That said, an early diagnosis, accompanied by appropriate treatment, will always be the most effective tool in treating a condition and reaching an optimal outcome.




















