Schwannoma
Schwannoma Overview
A schwannoma is a rare type of tumor that develops from cells called Schwann cells.
Nerves carry electrical signals throughout the body. Schwann cells are like the insulation around those wires, keeping them functioning with a fatty substance called myelin. When a schwannoma forms and compresses the nearby nerve, it can cause symptoms ranging from pain, numbness, tingling, weakness, or even loss of muscle function. In short, when a Schwann cell grows uncontrollably, it forms a schwannoma.
Schwannomas only occur on the nerves of the peripheral nervous system, outside of the brain and spinal cord. (Another kind of cell, oligodendrocytes, is responsible for myelin formation in the brain and spinal cord.)
The exact cause of schwannomas is not fully understood. They can sometimes be associated with genetic conditions called neurofibromatosis type 2 (NF2) and schwannomatosis. Vestibular schwannomas, also called acoustic neuromas, are the most common type of schwannoma and affect the nerves that connect your inner ear to your brain.
Schwannomas tend to grow slowly and are generally non-cancerous (benign). However, in rare cases, they can be cancerous (malignant). Most schwannomas can be treated and cured through surgery.

Schwannoma Symptoms
The symptoms of a schwannoma vary depending on its size, location, and associated nerve. For example, if it’s near a nerve in your arm, you may feel pain, weakness, or tingling in that arm.
A visible or palpable lump can develop at the site of the schwannoma, especially if it’s growing near the skin.
Other symptoms include:
- Intermittent or consistent pain in the area where the tumor is located (although not all schwannomas cause pain)
- Numbness and tingling sensations in the area of the affected nerve
- Loss of sensation in the area of the affected nerve
- Muscle weakness or changes in reflexes
- Dizziness or balance problems
- Hearing loss or ringing in ears
Your doctor can’t diagnose a schwannoma based on symptoms alone. Schwannomas grow slowly, can exist for years without symptoms, and can be present in multiple locations. Only a medical professional can give you an accurate diagnosis.
Schwannoma Diagnosis
Diagnostic imaging—typically computed tomography (CT) or magnetic resonance imaging (MRI)—confirms the presence of a schwannoma tumor and looks for indications that it may have spread to other parts of the body.
While a provider may suspect a schwannoma based on CT or MRI images alone, a biopsy is still required to provide a definitive diagnosis. This requires taking a small sample from the tumor with a needle to be studied by a neuropathologist.
Schwannoma Treatments
Schwannoma treatment will depend on various factors, including the size and location of the tumor, the severity of symptoms, and your overall health.
Surgery
The primary treatment is the surgical removal of the schwannoma. The goal of the surgery is to remove the tumor altogether while preserving the function of the affected nerve and relieving any symptoms it’s causing, like pain or numbness. Although schwannomas are typically not cancerous, they can grow and cause more problems if not treated. Some schwannomas can be removed without disturbing surrounding nerve tissue, but more extensive surgery may be required if your tumor is large or deeply embedded.
The specifics of the surgery depend on the location of the schwannoma. Generally, the procedure is done under general anesthesia, which means you’ll be asleep and won’t feel anything during the surgery. The surgeon makes an incision near the site of the tumor to access and remove it. Microsurgical techniques (operating with the assistance of a microscope) are often used to minimize damage to surrounding nerve tissues.
The risks of this surgery include infection, bleeding, and adverse reactions to anesthesia. There’s also the risk of nerve damage, which can lead to weakness, numbness, or paralysis in the affected area. These complications are rare under the care of an experienced neurosurgeon. Your neurosurgeon will discuss these risks with you in detail and the measures taken to minimize them.
Recovery varies depending on the tumor’s location and the complexity of the surgery. You may need to stay in the hospital for a few days after the procedure. Pain and discomfort around the incision site are common but manageable with medication. If the schwannoma or surgery affects your nerve function, your doctor may recommend physical therapy to help you regain strength and mobility. Follow-up visits will be necessary to monitor your recovery and ensure the tumor hasn’t returned
Nonsurgical Treatments
In situations where complete removal of the tumor is not feasible or if a person is not a suitable candidate for surgery, other treatments can be considered. They include:
- Observation: If your schwannoma is small, slow-growing, and not causing significant symptoms, your doctor may recommend regular monitoring through imaging tests to observe any changes over time.
- Radiation therapy: In some cases, radiation therapy may be used to shrink the tumor or prevent growth. This option is typically reserved for patients who are unable to undergo surgery or for schwannoma tumors that have recurred after surgery. However, sometimes it’s used in combination with surgery.
- Stereotactic radiosurgery: With this technique, doctors precisely deliver radiation without making an incision. If the schwannoma is near vital nerves or blood vessels, this treatment may be used to limit damage to healthy tissue.
- Medications: Certain medications, like pain relievers or corticosteroids, may be prescribed to manage pain or inflammation associated with the tumor.
Common Questions about Schwannoma
How common are Schwannomas?
Schwannomas are rare, with less than 200,000 diagnosed cases yearly in the United States. However, they are the most common tumors of peripheral nerves in adults. The exact incidence of schwannomas in the general population is not clearly defined due to their rarity and the fact that they often remain asymptomatic and undiagnosed. However, some general insights can be provided:
- Vestibular Schwannomas (Acoustic Neuromas): These are the most common types of schwannomas arising from the nerve that connects the inner ear to the brain. They account for about 6-8% of all primary brain tumors. The estimated incidence is about 1 per 100,000 individuals per year.
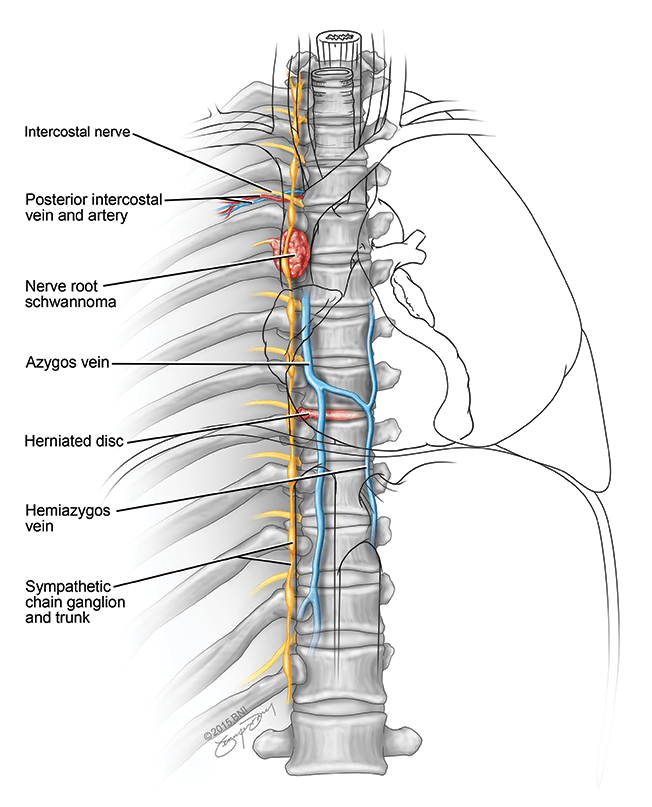
- Spinal Schwannomas: These are less common than vestibular schwannomas. They can occur within the spinal canal and may cause symptoms related to compression of spinal nerves. The incidence rate of spinal schwannomas is not well documented. Still, it is considered to be lower than that of vestibular schwannomas.
- Schwannomatosis: This is a rare disorder characterized by developing multiple schwannomas throughout the nervous system, excluding the vestibular nerve. The incidence of schwannomatosis is estimated to be about 1 in 40,000 individuals.
- Neurofibromatosis Type 2 (NF2): This is a genetic disorder that makes it more likely that people will develop multiple tumors in their nervous system, including schwannomas, particularly on the cranial and spinal nerves. The incidence of NF2 is approximately 1 in 25,000 to 1 in 40,000 births.
Schwannomas can occur at any age but are most commonly diagnosed in adults between 20 and 50. They are slightly more common in women than in men. Most schwannomas are solitary and sporadic, although individuals with certain genetic conditions like NF2 are at a higher risk of developing multiple tumors.
Given their benign nature, schwannomas often grow slowly and may not cause symptoms for many years. As such, some individuals may have schwannomas that remain undetected throughout their lives, potentially making the true incidence of these tumors higher than what is documented.
Who gets Schwannomas?
Schwannoma can occur in people of all ages. However, they are more common in people with the genetic disorders neurofibromatosis type 2 (NF2) and schwannomatosis. Schwannomas rarely run in families, but these same genetic disorders in a family may increase a family member’s risk of schwannoma.
What is the prognosis for those diagnosed with schwannoma?
Schwannomas are typically benign (non-cancerous) tumors that grow on the sheaths of nerves throughout the body. Because they are benign, discussing survival rates in the context often used for cancer patients—such as five-year survival rates—is not entirely applicable. Instead, the focus with schwannomas is usually on successful removal, management of symptoms, and preservation of nerve function.
The prognosis for individuals with schwannomas is generally excellent, especially when the tumors are detected early and are accessible for surgical removal. The outcomes of surgery or other treatments depend on the location of the tumor, its size, and whether it affects critical structures or nerve functions. For most patients, complete removal of the schwannoma is possible, which typically results in a cure of the condition associated with the tumor.
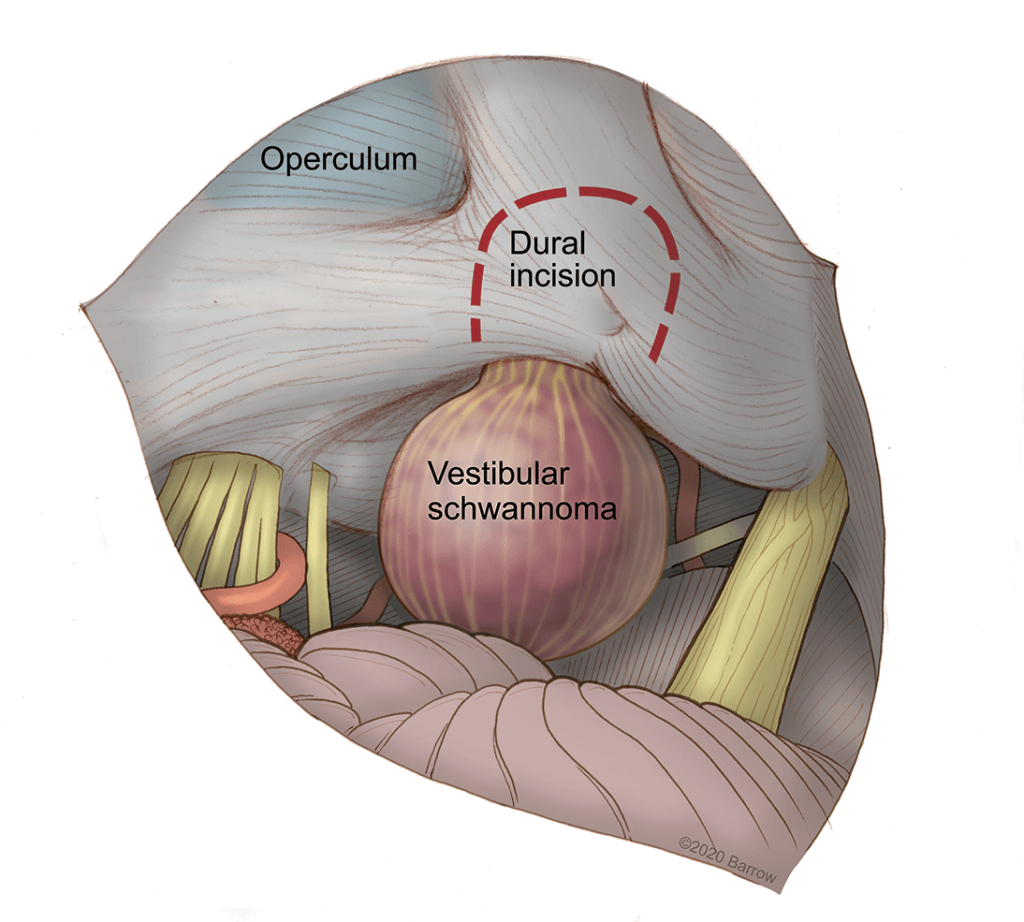
For schwannomas in locations that make surgery more complex, such as vestibular schwannomas (also known as acoustic neuromas) that affect the nerves related to hearing and balance, treatment goals include maximizing tumor removal while minimizing impacts on hearing, balance, and facial nerve function. Even in these more complex cases, modern surgical techniques and other treatment modalities (like stereotactic radiosurgery) have significantly improved outcomes, allowing many patients to maintain a good quality of life.
In cases where schwannomas are associated with genetic conditions, such as Neurofibromatosis Type 2 (NF2), the management might be more complicated due to the presence of multiple tumors. Even then, the focus remains on managing symptoms, reducing tumor size, and preserving nerve function to the greatest extent possible.
Overall, the survival rate for individuals with schwannomas is excellent since these tumors are benign. The key challenges typically revolve around managing symptoms and preventing or addressing functional impairments related to the tumors. Regular follow-ups and monitoring are essential, especially in cases where complete tumor removal isn’t possible or in individuals with conditions that predispose them to develop multiple schwannomas.
What is the most common location for a schwannoma?
The most common location for a schwannoma is on cranial nerve VIII, also known as the vestibular nerve. This nerve is part of the nerve system connecting the inner ear to the brain. Tumors in this location are specifically referred to as vestibular schwannomas or acoustic neuromas. Given the vestibular nerve’s role in these functions, these tumors are notable for affecting hearing and balance.
Other relatively common locations for schwannomas include the spinal nerves, where they can grow within the spinal canal or on nerves that branch out from the spinal cord. These spinal schwannomas can lead to symptoms depending on their size and location, including pain, weakness, or numbness in the limbs or trunk, and issues with bladder or bowel control.
The location of a schwannoma largely determines the approach to treatment and management, as well as the potential impacts on the patient’s health and function.
Where are cancerous schwannomas most likely to form?
Cancerous schwannomas, known as malignant peripheral nerve sheath tumors (MPNSTs), are sporadic. These malignant tumors arise from the nerve sheath cells surrounding peripheral nerves and are more aggressive than their benign counterparts. They can develop anywhere in the body but are most common in the following locations:
- Deep Tissue of the Arms and Legs: MPNSTs often occur in the proximal regions of the limbs, closer to the body. This is partly because the larger peripheral nerves from which these tumors originate are located in these areas.
- Trunk: The trunk of the body, including the chest and abdominal areas, is another common location for these tumors. Here, the tumors can affect the larger nerve plexuses.
- Head and Neck: Though less common than in the limbs or trunk, malignant schwannomas can also occur in the head and neck region, affecting the associated nerves.
- Pelvic Region: MPNSTs can develop in the pelvic region, involving the nerves that supply this area.
These tumors are often associated with genetic conditions, such as neurofibromatosis type 1 (NF1), which significantly increases the risk of developing MPNSTs. In individuals with NF1, these malignant tumors may arise from preexisting benign neurofibromas that undergo malignant transformation.
The prognosis for MPNSTs can be challenging, as these tumors tend to be more aggressive and have a higher risk of recurrence and metastasis compared to benign schwannomas. Treatment typically involves a combination of surgery, radiation therapy, and chemotherapy aimed at removing the tumor, controlling its spread, and managing symptoms.
Given their rarity, any new or worsening symptoms in individuals with a history of neurofibromatosis or other nerve-related tumors should prompt immediate medical evaluation to rule out malignancy and determine the most appropriate course of action.
Information and Resources for Schwannoma
References
- Hendricks BK, DiDomenico JD, Barani IJ, Barranco FD. ZAP-X Gyroscopic Radiosurgery System: A Preliminary Analysis of Clinical Applications within a Retrospective Case Series. Stereotact Funct Neurosurg. 2022;100(2):99-107. doi: 10.1159/000519862. Epub 2021 Dec 23. PMID: 34942629.
- Breshears JD, Osorio JA, Cheung SW, Barani IJ, Theodosopoulos PV. Surgery After Primary Radiation Treatment for Sporadic Vestibular Schwannomas: Case Series. Oper Neurosurg (Hagerstown). 2017 Aug 1;13(4):441-447. doi: 10.1093/ons/opx023. PMID: 28838116..