
Herniated Thoracic Disc
Herniated Thoracic Disc Overview
A herniated thoracic disc (also called thoracic disc herniation or thoracic herniated disc) is a serious but treatable spinal condition in which the soft center of a thoracic intervertebral disc (the nucleus pulposus) pushes through a tear in the tough outer layer of the disc (the annulus fibrosus) and into the spinal canal. The protruding disc fragment can put pressure on the thoracic segment of the spine and spinal cord, causing upper back and chest pain and dysfunction in the thoracic spinal cord.
Intervertebral discs act as shock absorbers for the spine and enable its movement. These discs can tear due to degeneration, injury, or a combination of both, and damaged discs can be a source of pain and other symptoms.
Herniated discs can occur in the lumbar spine (lower back), cervical spine (neck), or thoracic spine (mid-back).
Anatomy of the Thoracic Spine
Your spine is made up of 33 vertebrae divided into five different segments, which are listed below in order from your head to your legs:
- Cervical, or the neck
- Thoracic, the middle of the back
- Lumbar, or lower back
- Sacrum, where the spine connects to the hips
- Coccyx, the tailbone
Thoracic herniated discs occur in the thoracic spine, which is made up of the 12 vertebrae that extend from the base of your neck to the bottom of your rib cage.
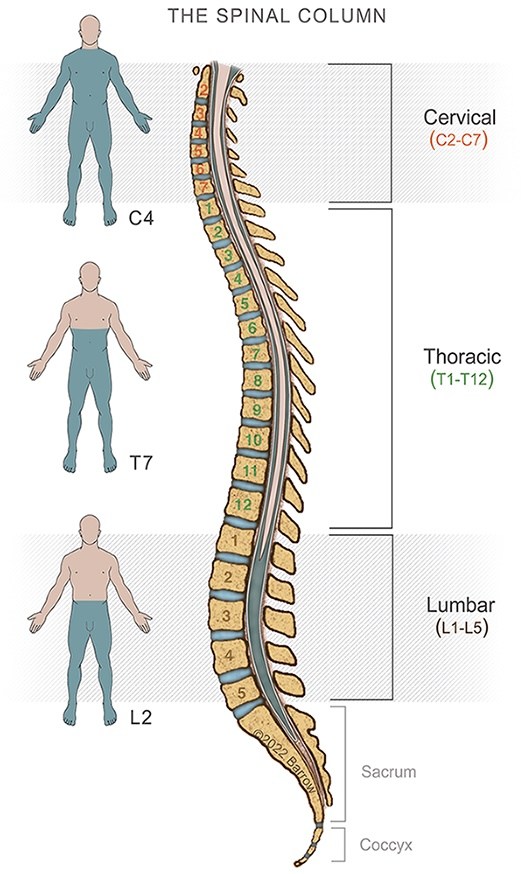
One of the main differences between thoracic vertebrae and vertebrae in other levels of the spine is that each thoracic vertebra has joints that connect it to the rib bone on each side of the spine. The support that the rib cage provides to the thoracic spine means it experiences less wear and tear than the other segments of the spine, making it less likely for the thoracic segment to develop thoracic herniated discs and other conditions.

Thoracic Herniated Disc Symptoms
Symptoms of a herniated thoracic disc may include:
- Radiculopathy: Pain in the mid-back, which may wrap around the chest
- Myelopathy: Difficulty walking, progressive weakness, numbness in the lower extremities, and occasionally bowel dysfunction
Radiculopathy
Radiculopathy is the technical term for pain or other symptoms caused by pinching of a nerve root that enters the spinal cord.
People often describe radiculopathy as feeling like a strap is being tightened around their chest. The location of this “strap” corresponds to the level of the spine where the herniated thoracic disc is located. It also corresponds to the parts of the body supplied by the nerve that is being pinched.
About 52% of people with a symptomatic herniated thoracic disc experience radiculopathy.
Many people assume that radiculopathy involves a sensation of pain, but that is not always the case. In addition to pain in or around the spine, radiculopathy can also describe numbness, weakness, a feeling of pressure, or generalized discomfort. Many people diagnosed with thoracic herniated disc experience no spine pain at all.
Myelopathy
Myelopathy describes the symptoms caused when pressure from the herniated disc puts pressure on the spinal cord. This can cause dysfunction in areas of the body below the level of the herniated thoracic disc, including the leg weakness and numbness mentioned above.
Myelopathy also can cause pain in the area where the spinal cord is compressed or pain in the extremities, although some people with myelopathy experience no pain at all.
Symptoms vary depending on the quantity of thoracic disc material that has escaped and which structures the escaped material is putting pressure on. In some instances, a thoracic herniated disc may not produce pain or any other symptoms.
It is common for doctors to suspect and investigate other, more common conditions because thoracic herniated discs are rare. Often times, people may be tested for heart problems, gastrointestinal problems, angina, lung issues, and shingles in this process.
About 70% of people with symptomatic thoracic disc herniation experience myelopathy.
Pain and other symptoms consistent with radiculopathy and myelopathy can be caused by other medical conditions. Only a medical professional can confirm or rule out a diagnosis of herniated thoracic disc.
Classification of Herniated Thoracic Discs
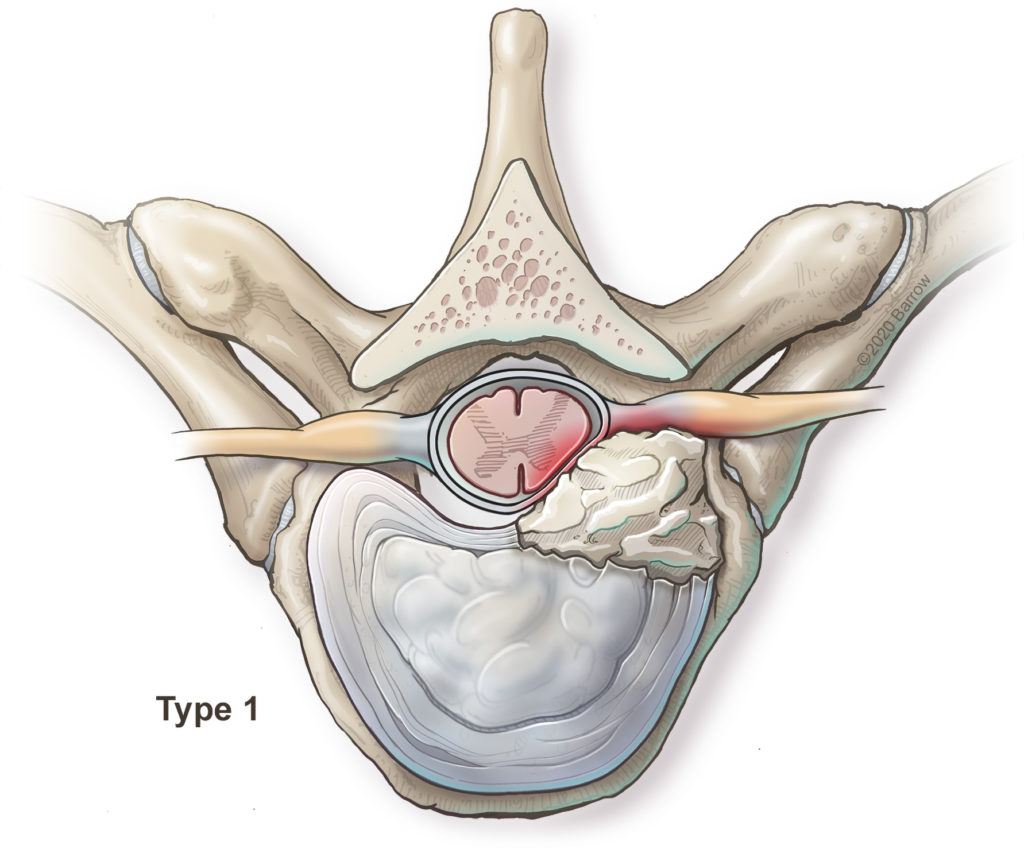
Spinal neurosurgeons at Barrow recently led the creation of a classification system for herniated thoracic discs based on their size, location, and whether or not they are calcified.1

Type 0 herniated thoracic discs are small, taking up 40% of the spinal canal or less, and do not put large amounts of pressure on the spinal cord or spinal nerves. Most surgeons recommend observation for these lesions.
Type 1 herniations are also small, but located to the side of the spinal canal, where they are more likely put pressure on the nerve roots that exit the spine and spinal cord or the side of the spinal cord itself. Most surgeons favor approaching these discs from the back (posterior approach).
Type 2 herniations are small but located in the middle of the spinal canal and are more likely to involve the spinal cord and not the spinal nerve roots. Spine surgeons may elect to approach these from the side or the back.
Type 3 herniations are very large and located to the side of the spinal canal.
Type 4 thoracic disc herniations are giant and located in the center of the spinal canal. Most surgeons prefer to approach type three and four herniations from the side.
Herniated Thoracic Disc Treatments
Most cases of thoracic disc herniation can be treated with a nonsurgical approach, which usually consists of rest, anti-inflammatory medication, and physical therapy. However, you may be a candidate for surgery if you have severe back pain and/or neurological symptoms that are not responding to conservative treatment.
Thoracic Discectomy
In this procedure, the neurosurgeon removes the protruding fragment of the disc that is compressing the spinal cord or spinal nerves and causing thoracic pain or other symptoms.
Traditionally, thoracic discectomy has been performed through an anterior (front) approach or a posterior (back) approach. At Barrow Neurological Institute, our spine surgeons are leaders in minimally invasive techniques, including minimally invasive lateral thoracic discectomy. The benefits of this approach, in which the spine surgeon accesses the spine through the side of the body using a less disruptive approach, include:
- A shorter hospital stay
- Less post-operative pain
- Less time in surgery
- Reduced blood loss
- Usually no need for chest tubes
Thoracic Fusion
In some cases, a degenerated disc may need to be removed entirely and the adjacent vertebrae fused together to stabilize the spine.
In this process, the neurosurgeon first removes the damaged thoracic disc. Then, the disc is replaced with a bone graft. This graft can be taken from the patient’s rib or hip (autograft) or from a cadaver donor (allograft).
After the bone graft has been placed, the neurosurgeon will usually place rods ands screws in the vertebrae above and below the disc that has been removed. This hardware stabilizes and supports the spine while the bone graft fuses with the surrounding vertebrae.
Spinal fusion can also be performed using minimally invasive techniques. Many people report that their pain and other symptoms are reduced or eliminated after surgery.
Common Questions about Herniated Thoracic Disc
How common is thoracic herniated disc?
Herniated discs are very common, but they usually occur in the lumbar spine as opposed to the thoracic region. Herniated discs in the thoracic region account for less than 1 percent of all herniated discs.
The thoracic region, which has more vertebrae than any other part of the spine, is the least-mobile region of the spine and therefore the least susceptible to disc herniation. Herniated discs in the thoracic spine have a tendency to become calcified, also known as hard disc herniation.
Who gets thoracic disc herniation?
Because thoracic disc herniation can be caused by an injury, it can affect anyone. However, it is most common in men between the ages of 40 and 60. As people age, their thoracic intervertebral discs may lose their cushioning ability and become more likely to rupture. Some research has shown that herniated discs run in families, suggesting that your genes can make it more likely that you will develop a herniated thoracic disc.
How is thoracic herniated disc diagnosed?
Your doctor may use the following to diagnose a thoracic herniated disc:
- Magnetic resonance imaging (MRI) is the best tool for observing and diagnosing problems with intervertebral discs
- Other Imaging tests, such as X-ray or computed tomography (CT) may be used, but are not as accurate as MRI in diagnosing a herniated thoracic disc
- Myelography, which involves injecting dye into the space around your spinal cord and taking X-ray or CT images to identify any narrowing in the spinal canal
- Medical history to identify any accidents, pre-existing conditions, or trauma that may have caused an injury to your spine
- Physical examination to record the type, severity, and location of your pain or other symptoms and draw conclusions about their cause
Sometimes other tests may be ordered because herniated thoracic disc pain and symptoms can mimic heart, lung, and stomach conditions.


Can a herniated thoracic disc heal on its own?
These lesions of the thoracic spine rarely heal on their own. However, many are found incidentally and never produce thoracic pain or other symptoms. In this case, they can be monitored over time until they begin to cause pain or other symptoms in the thoracic region.
Because this thoracic spine condition is so rare, there are not good data showing what percentage of herniated thoracic discs heal on their own.
Can a herniated thoracic disc cause paralysis?
Herniated thoracic discs can cause paralysis. However, the onset of paralysis in this condition is gradual. You will not be suddenly and completely paralyzed by a herniated thoracic disc.
The majority of herniated thoracic discs are diagnosed and treated before they progress to even partial paralysis.
Can paralysis caused by herniated thoracic disc be reversed?
Surgery can usually reverse gradual onset paralysis caused by a herniated thoracic disc, along with pain in the thoracic region and other symptoms.
However, there is a chance that some symptoms from a thoracic lesion will not improve after surgery. For this reason, it is important to see a doctor if you are experiencing pain or any of the symptoms listed above or if your existing symptoms become worse.
What causes thoracic disc herniation?
Sometimes the cause of a thoracic disc herniation is idiopathic, meaning the cause is not known. Other causes include trauma to the spine, such as a motor vehicle accident, and degenerative conditions.
When should I call a doctor?
If you are experiencing pain or others symptoms of a herniated thoracic disc, you should make an appointment to see your primary care doctor. They can help rule out other conditions and give you a referral to a specialist.
A spine surgeon or spinal neurosurgeon can assess your herniated thoracic disc and help you decide if it would be best to have surgery or to try conservative treatment.
When should I consider surgery?
Generally speaking, most neurosurgeons will advise against surgery if you are not experiencing pain or symptoms. If you begin to experience symptoms, or if your mild symptoms like pain, radiculopathy, myelopathy become worse, it may be time to consider surgery.
The exception to this is for a giant herniated thoracic disc, which almost always requires surgery. A herniated thoracic disc is considered giant if it obstructs more than 50% of the central canal of the spine (the central canal is the part of the spine that protects the spinal cord). Even if it is not causing pain or symptoms, a giant disc herniation will usually require surgical treatment.
Videos


Additional Resources
References
- Farber SH, Walker CT, Zhou JJ, Godzik J, Gandhi SV, de Andrada Pereira B, Koffie RM, Xu DS, Sciubba DM, Shin JH, Steinmetz MP, Wang MY, Shaffrey CI, Kanter AS, Yen CP, Chou D, Blaskiewicz DJ, Phillips FM, Park P, Mummaneni PV, Fessler RD, Härtl R, Glassman SD, Koski T, Deviren V, Taylor WR, Kakarla UK, Turner JD, Uribe JS. Reliability of a Novel Classification System for Thoracic Disc Herniations. Spine (Phila Pa 1976). 2023 May 1. doi: 10.1097/BRS.0000000000004701. Epub ahead of print. PMID: 37134139.
- Farber SH, Xu DS, Walker CT, Godzik J, Turner JD, Uribe JS. Minimally Invasive Retropleural Thoracic Diskectomy: Step-by-Step Operative Planning, Execution, and Results. Oper Neurosurg (Hagerstown). 2022 Oct 1;23(4):e220-e227. doi: 10.1227/ons.0000000000000315. Epub 2022 Jul 11. PMID: 36001756.
- Uribe JS, Smith WD, Pimenta L, Härtl R, Dakwar E, Modhia UM, Pollock GA, Nagineni V, Smith R, Christian G, Oliveira L, Marchi L, Deviren V. Minimally invasive lateral approach for symptomatic thoracic disc herniation: initial multicenter clinical experience. J Neurosurg Spine. 2012 Mar;16(3):264-79. doi: 10.3171/2011.10.SPINE11291. Epub 2011 Dec 16. PMID: 22176427.
- Christiansen PA, Huang S, Smith JS, Shaffrey ME, Uribe JS, Yen CP. Mini-open lateral retropleural/retroperitoneal approaches for thoracic and thoracolumbar junction anterior column pathologies. Neurosurg Focus. 2020 Sep;49(3):E13. doi: 10.3171/2020.6.FOCUS20360. PMID: 32871570.
- Yen CP, Uribe JS. Mini-open Lateral Retropleural Approach for Symptomatic Thoracic Disk Herniations. Clin Spine Surg. 2018 Feb;31(1):14-21. doi: 10.1097/BSD.0000000000000580. PMID: 28857966.






