
The Two-Point Method: Evaluating Brain Stem Lesions
Authors
Adam P. Brown, MD*
B. Gregory Thompson, MD
Robert F. Spetzler, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
*Current Address: Coastal Neurosurgical Associates, Wilmington NC 28401
Abstract
Many brain stem masses are amenable to surgical therapy. The technical options for accessing these lesions include one of the standard approaches (i.e., suboccipital, retrosigmoid) or a more extensive skull base approach. The most critical factor in deciding upon the surgical route is to choose a pathway that avoids incising essential neural tissue if possible. To comply with this requirement, we use a simple paradigm, the two-point method. Intuitively used by experienced surgeons, this method dictates the surgical approach to brain stem lesions that provides the best exposure while minimizing tissue retraction. Several case examples demonstrate the use of this method.
Key Words : brain stem, cavernous malformation, skull base, surgical approaches
One of the difficulties that arises during the surgical removal of lesions involving the brain stem is that essential tissue often must be traversed to gain access to the path-ology. The recent explosion of skull base techniques, however, enables neurosurgeons to gain access to most surfaces of the brain stem. The dilemma becomes which technique or route is best for approaching a given lesion. Should the most direct and therefore shortest approach be selected or should a line of sight through the center of the mass be chosen? A simple paradigm, proposed by the senior author (RFS), is presented for selecting the safest route. This two point method is universally applicable to surgical lesions of the brain stem, encompassing the regions from below the craniovertebral junction to above the tentorial incisura. This method, intuitively used by experienced neurosurgeons, is presented to simplify the correct choice of approach.
Description of the Two-Point Method
The objective in using the two-point method is to select the approach that leads to the pathology while avoiding incision of brain stem tissue. Hence most lesions that are to be approached surgically are close to or contact a pial or ependymal surface.
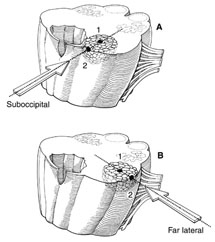
The patient is evaluated in a standard neurosurgical fashion. A magnetic resonance (MR) imaging study of the lesion, including the sagittal, coronal, and axial planes, is obtained. The appropriate images are selected such that the center of the lesion can be assigned as well as those in which the lesion abuts or comes closest to a pial or ependymal surface or overlying tissue (Fig. 1). A line is then drawn from the center point (point 1) through the superficial point (point 2) and out toward the skull, subcutaneous tissues, and skin. This line dictates the approach to be used for resection of the lesion.
Important factors to be considered are, for example, the eloquence of the floor of the fourth ventricle, which often dictates a lateral approach even though a direct approach through the floor of the fourth ventricle would be technically easier. Placing a point in the center of the lesion and connecting it to the appropriate entry point dictate an angle that avoids a tangential approach to the lesion, which would be possible if one considered only where the lesion comes closest to the surface. This important concept decreases the risk of additional damage from retraction while removing the lesion.
Case 1
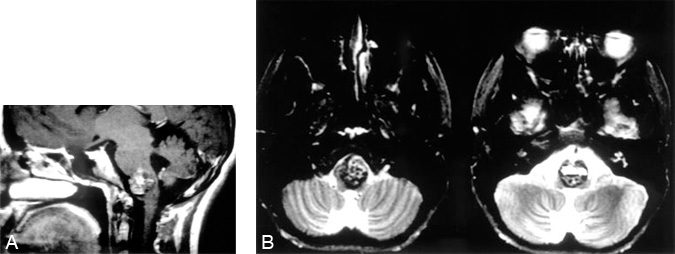
A 17-year-old female presented with complaints of right-sided clumsiness and incoordination after a severe headache. A detailed neurological examination revealed intact cranial nerves and motor strength with right-sided dysmetria and ataxia. A computed tomography scan of the brain revealed a hypointense area in the lower brain stem. An MR image demonstrated the same lesion (Fig. 2A), which was thought to be most consistent with a cavernous malformation. The MR study also revealed a large cisterna magna and a thin rim of neural tissue separating the malformation from this cistern. While planning the surgery, it was thought that this posterior rim of tissue would prohibit the midline suboccipital exposure. On axial images (Fig. 2B), however, the cavernoma was seen to extend to the left lateral pial surface. Using these images with the two-point method, the first point was placed in the center of the lesion with the second point at the left lateral pial surface. Connecting points 1 and 2 and extrapolating the line suggested a lateral operation. When the size and location of the lesion and its rostralcaudal dimension were considered, the far-lateral approach was selected.2-4 This exposure did not require incision of essential neural tissue, which would have been required if a midline suboccipital operation had been chosen. In addition, the far-lateral approach provided a flatter line of sight to the ventrolateral aspect of the brain stem, enabling less brain retraction than might have been necessary had a retrosigmoid exposure been used. A cavernous malformation was removed uneventfully.
Case 2
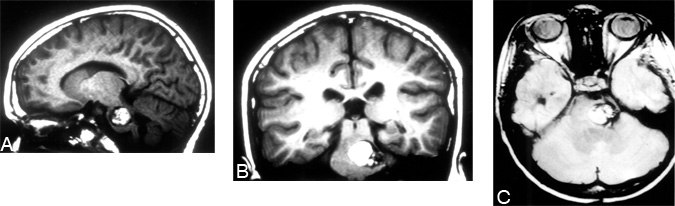
A 13-year-old male with several cavernous malformations, including one located in the pons, was referred to our institution. His history suggested multiple hemorrhages. Serial MR imaging demonstrated progressive enlargement of the brain stem cavernoma. Upon examination at the time of referral, the patient exhibited right hemiparesis, gait ataxia, and a right facial droop with facial numbness. MR imaging before surgery showed the malformation (Fig. 3) located eccentrically in the pons. Applying the two-point method to the lesion dictated a lateral approach. Because of the lesion’s lateral axis, however, we believed that visualization with a standard retrosigmoid approach would be inadequate without excessive brain retraction. Therefore, a left retrolabyrinthine (hearing-sparing) craniectomy was performed. A gross total resection was achieved. Postoperatively, the patient had no new neurological deficits, and he was discharged home 6 days after surgery.
Case 3
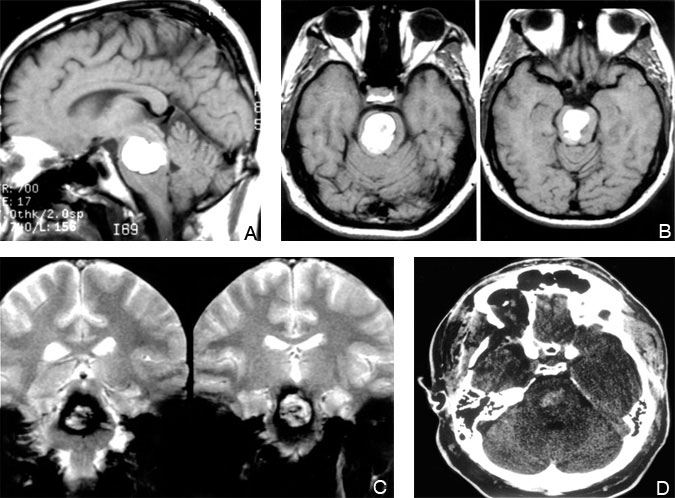
A 25-year-old female had been followed for a cystic mass of the brain stem since the age of 5 years. Recently, she complained of worsening right-sided weakness, numbness, gait difficulty, diplopia, nausea, and headache. Follow-up MR imaging demonstrated an increase in the size of the lesion (Figs. 4A, B, and C). Application of the two-point method to this lesion suggested an anterolateral approach. A subtemporal craniotomy with a zygomatic osteotomy was performed and gross total resection achieved (Fig. 4D). Pathological examination revealed a pilocytic astrocytoma. Postoperatively, her strength and gait improved and her numbness, nausea, and headaches resolved.
Case 4
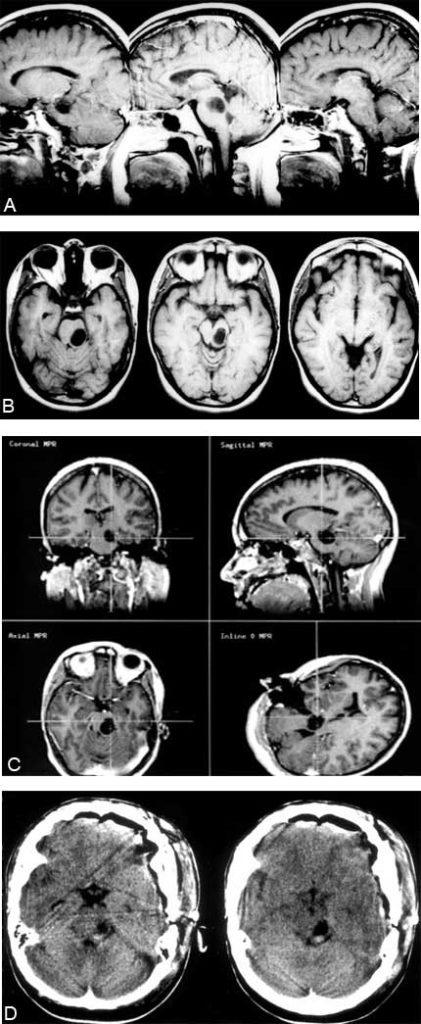
A 30-year-old male suffered the acute onset of slurred speech, numbness and weakness of the left hand and face, and decreased coordination. T1-weighted MR images revealed a large hyperintense mass centered in the rostral pons (Fig. 5). T2-weighted images showed a hypointense rim consistent with hemosiderin. Application of the two-point method placed the first point in the lesion’s center and the second point anteriorly almost in the midline. Connecting these two points with a line dictated an anterior approach to the mass. Alternatively, a subtemporal exposure would enable removal but at the cost of traversing a rim of essential tissue (Fig. 5). A cavernous malformation was removed via a right pterional craniotomy in conjunction with an orbitozygomatic osteotomy (Fig. 5). The patient was discharged home on the 10th postoperative day while continuing outpatient therapy.
Most neurosurgeons are becoming increasingly familiar and comfortable with skull base approaches for deep seated masses. For brain stem lesions that must be removed or biopsied, many surgical exposures are possible, from the midline posteriorly to the lateral and anterior routes. The exposure selected may depend on several factors, including the technical ease of the approach, the most direct (shortest) approach, or the exposure that transverses the least neural tissue. Sometimes these considerations can be accomplished simultaneously as, for example, with a lesion protruding through the floor of the fourth ventricle. A question may arise about the most suitable approach, however, when the shortest or most direct route crosses eloquent tissue—for example, when a cavernous malformation lies a couple of millimeters below the surface of the fourth ventricle as in Cases 1 and 4. Such a situation may dictate an alternative approach to spare essential neural tissue. Often the approach selected may be more technically demanding and time consuming, but it is preferable to avoid the risk of a neurological deficit. Therefore, a full command of these approaches is mandatory in evaluating and removing brain stem lesions.
T1- and T2-weighted images are helpful to determine the surgical exposure by the two-point method. For example, in lesions that do not reach a surface, images should be examined carefully to select the safest approach. A frameless stereotactic guidance system becomes invaluable in selecting the point of incision on the exposed brain stem.
All brain stem lesions at our institution are evaluated with the two-point method. If the lesion is considered amenable to surgery, the approach is selected based on this evaluation. To date we have used the method to determine the surgical approach in more than 85 operations, including for cavernous malformations, tumors, and arteriovenous malformations. The institution of this method has led to a change in our standard operative approach to these lesions. Furthermore, the acquisition and routine use of intraoperative frameless stereotactic guidance have been invaluable in using this method to its full potential and in helping to achieve gross total resections.1
In conclusion, we believe every effort should be made to avoid traversing the neural tissue of the brain stem. Consequently, a slightly less direct surgical approach may be needed to remove lesions in the brain stem. Furthermore, the selected skull base exposure may require more time, greater technical expertise, and a longer reach than the “shorter” route. However, in most instances, both the patient and the surgeon are rewarded by superior access to the lesion with less neural retraction.
References
- Golfinos JG, Fitzpatrick BC, Smith LR, et al: Clinical use of a frameless stereotactic arm: Results of 325 cases. J Neurosurg 83:197-205, 1995
- Heros RC: Lateral suboccipital approach for vertebral and vertebrobasilar artery lesions. J Neurosurg 64:559-562, 1986
- Sen CN, Sekhar LN: An extreme lateral approach to intradural lesions of the cervical spine and foramen magnum. Neurosurgery 27:197-204, 1990
- Spetzler RF, Grahm TW: The far-lateral approach to the inferior clivus and the upper cervical region: Technical note. BNI Quarterly 6:35-38, 1990
