
Management of Thoracic Vertebral Giant Cell Tumor with Complete Spondylectomy: Case Report
Ratul Raychaudhuri, BA*
Pankaj Gore, MD
Michael Webb, MD
Curtis A. Dickman, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona *University of Texas Southwestern Medical Center, Dallas, Texas
Abstract: Extrasacral spinal giant cell tumors are rare entities. Total en bloc spondylectomy offers the best chance for curing these potentially locally aggressive lesions. We report the management of a patient with an invasive grade III giant cell tumor of the T2-4 vertebrae with spondylectomy and reconstruction of the vertebral defect.
Key Words: giant cell tumor, spondylectomy, thoracic spine
Abbreviations Used: CT, computed tomography; MR, magnetic resonance
Giant cell tumors of the spine are uncommon lesions that afflict young to middle-aged individuals. The locally aggressive behavior and high recurrence rate associated with this tumor can necessitate radical resection and complex spinal reconstruction for potential cure. We present the management of a patient with high-grade multilevel thoracic giant cell tumor.
Case Illustration
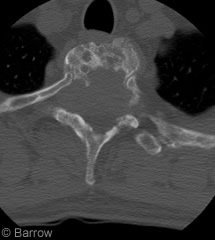
Figure 1. Preoperative CT scan shows a destructive lesion involving all three spinal columns within the T3 vertebrae.
Presentation
A 45-year-old man had a history of diffuse back and shoulder pain that progressed to bilateral weakness and myelopathy of the lower extremities. He had no history of a prior malignancy or other comorbidity. CT demonstrated expansile lytic lesions within the vertebral bodies of T2 and T3 with extensions into the lamina, facets, and transverse processes on the left (Fig. 1).
MR imaging showed a heterogeneously enhancing and destructive mass centered within the vertebral bodies of T2 and T3 (Fig. 2). The lesion involved the posterior elements bilaterally and extended into the ventral epidural space. A contour deformity of the spinal cord and abnormal T2-weighted hyperintensity within the spinal cord were apparent. The superior aspect of the T4 vertebral body was also involved, and the T1 through T4 neural foramina were narrowed bilaterally. These findings were thought to be most compatible with a neoplastic process. The initial biopsy at an outside institution was inconclusive but suspicious for malignant spindle cell tumor. The patient was treated at the outside facility with a single radiation dose of 6 Gy. A second biopsy was conducted and definitively interpreted as giant cell tumor. The patient was referred to our institution for further care.
Surgical Technique
The surgical procedure was staged. In the initial posterior approach, the C5 to T9 levels were instrumented (lateral mass screws at the cervical levels, transverse process screws at T1, and pedicle screws from T5-T9). The laminae, facets, transverse processes, and pedicles of T1 to T4 were excised. The T1 through T4 nerve roots, which were thoroughly involved with tumor, were sacrificed to permit partial spondylectomy of the posterior and middle columns of the T2-4 vertebrae. The posterior elements were resected in piecemeal fashion with the double-action rongeur. The osteotome was used to free the middle column for resection through the posterior approach. Use of the high-speed drill was avoided to prevent tumor spillage. Five days later the patient underwent a transsternal approach for completion of the spondylectomy, C5-T1 anterior cervical diskectomies, fusion with a T1-T5 Harms cage, and C5 to T5 anterior plating (Fig. 3).
Hospital Course and Follow-Up
After the second procedure the patient’s postoperative hospital course was complicated by a sterile left pleural effusion that was treated with thoracentesis. On neurological examination he exhibited slight intrinsic muscle weakness in both hands, which was expected after bilateral sacrifice of the T1 root. He also had mild persistent weakness of the left iliopsoas (grade 4/5). He was fitted with a cervicothoracolumbosacral orthosis and mobilized. After 29 days of hospitalization, the patient was discharged to a neurorehabilitation facility. A course of three-dimensional conformal radiation with a total dose of 45

Gy was initiated 10 weeks after the patient’s discharge. At his 6-month follow-up examination, CT and radiographs demonstrated satisfactory fusion of the instrumented levels. The patient was independently ambulatory with 5/5 strength in his lower extremities. Mild proprioceptive deficits and numbness were still present in his lower extremities but were significantly improved compared to his preoperative status. At his 1-year follow-up examination, he had no evidence of recurrent tumor.
Discussion
Giant cell tumors were first reported by Cooper and Travers.[7] These benign but locally aggressive primary bone neoplasms have a predilection for epiphyseal areas surrounding the knee joint[9] and a tendency toward pulmonary metastases. Both local recurrence and pulmonary metastasis can be compatible with longterm survival.[6] Spinal involvement outside the sacrum is rare, estimated at 1.3 to 3.3%.[8,12]

Histologically, giant cell tumors consist of two main cell types, stromal and giant cells. Mononuclear stromal cells exhibit true cytologic atypia and are the only proliferating element within the lesion.[31] Giant cells are large and have more than 20 to 30 nuclei, mostly in a pericentral location.[23] These non-neoplastic cells are a fusion of monocytes that has been recruited into the lesion. Morphologically, the ruffled appearance of these cells is similar to that of osteoclasts. Giant cells can be found in a number of reactive and neoplastic bony lesions, including brown tumors in hyperparathyroid disease, chondroblastomas, chondromyxomas, giant cell reparative granulomas, and giant cell osteosarcomas.
Campanacci et al.[3] devised a radiographic grading system for giant cell tumors based on their x-ray appearance. Grade I tumors have a well-marginated border composed of a thin rim of bone, with an intact or slightly thinned cortex that is not deformed. Grade II tumors have relatively well-defined margins but no radio-opaque rim. The cortex and rim of reactive bone are thin and moderately expanded. Grade III tumors have indistinct borders, suggesting rapid growth. The tumor mass, which does not follow the contour of the bone, bulges into soft tissue. The recurrence rate after surgery does not correlate with radiographic grade but rather with extent of excision.[3]
The optimal management of giant cell tumors within the long bones involves excision with wide margins.[17,22,28] Dahlin[8] reported that the recurrence rate of giant cell tumors in the spine (16.5%) was one-third of that associated with other locations (44%). In this series, resection was almost uniformly subtotal. Hart et al. reported that high recurrence rates of vertebral giant cell tumors are associated with initial surgical excision at a nontertiary care center (83%), involvement of both anterior and posterior elements (24%), and combined extension into the spinal canal and paraspinous soft tissues (21%).[13]
The efficacy of radiation therapy in the management of vertebral giant cell tumors is uncertain. Khan et al. reported six vertebral giant cell tumors that were subtotally resected or biopsied and treated with a mean radiation dose of 39 Gy.[16] Three of these six tumors recurred and required surgical salvage. Caudell et al.[4] reported 25 giant cell tumors of which 20 involved the spine. All patients underwent radiation therapy with a median dosage of 46 Gy. Eleven patients underwent gross total resection of their tumor before radiation treatment. The remaining 14 had bulk disease at the time of treatment. At a median follow-up of 8.8 years, 12 patients had developed a local or distant recurrence or both. The authors concluded that radiation should be considered as an adjuvant to surgery or as primary therapy in cases of “unresectable” giant cell tumors. The study, however, spanned 44 years and does not reflect contemporary radiation oncological planning and stereotactic technology. In a series of 21 patients (13 with a primary tumor, 8 with a recurrence) with a mean follow-up of 15.4 years, Malone et al.[19] reported that the local control rate associated with radiotherapy was 92%. Miszczyk et al. have suggested that a radiotherapy dose of 40 to 45 Gy is an “effective sole treatment” for giant cell tumors smaller than 4 cm.[21]
Most authors agree that spondylectomy with or without adjuvant radiation remains the gold standard.[1,11,15,18,25,26] Stener and Johnsen[27] were among the first to describe total spondylectomy for vertebral giant cell tumors. Since then multiple authors have reported successful cervical, thoracic, and lumbar spondylectomy for surgical treatment of giant cell tumors.[1,11,14,15,18,25,26] After total spondylectomy for lower thoracic vertebrae, complications such as anterior spinal artery syndrome have been reported.[10]
When a giant cell tumor does not involve the posterior elements of the vertebrae, Fidler[11] has advocated en bloc spondylectomy, which can be achieved through a single-stage approach or through a two-stage combined anteriorposterior approach.[11,20,29] Fidler also emphasized extralesional dissection during spondylectomy to prevent tumor spillage. Despite meticulous technique and liberal use of frozen sections to check margins, there were two recurrences in Fidler’s nine patients, one local and the other distant (mean follow-up, 6.4 years).
Given the extension of tumor to the epidural space and posterior elements in our patient, wide en bloc excision was infeasible. The posterior elements were resected piecemeal with the Leksell and large Kerrison rongeur. The involved pedicles were osteotomized as were the T2-4 vetebral bodies and T1-2 and T4-5 disk spaces. Involved nerve roots were ligated, and the posterior half of the T2-4 vertebral bodies was resected. The transsternal approach facilitated en bloc removal of the remaining anterior portion of the T2-4 vertebral bodies. At the conclusion of the second-stage procedure, we believed that gross total resection had been achieved.
Although several authors have used the high-speed bur for intralesional tumor removal,[2,14,30] we believe that its use increases the likelihood of tumor spillage.
Local recurrence of giant cell tumor can typically manifest 3 to 5 years after a patient’s initial surgery.[3,13,24] During this period and beyond, our patient will require vigilant follow-up.
Conclusions
En bloc resection is the best primary treatment for a giant cell tumor of the spine. When three-column spinal involvement precludes en bloc resection, complete spondylectomy can still result in gross total resection of tumor. Tumor spillage should be avoided to the fullest extent.[5] Radiotherapy should be considered as an adjuvant to surgery rather than as a primary treatment for vertebral giant cell tumors.
References
- Abe E, Sato K, Tazawa H, et al: Total spondylectomy for primary tumor of the thoracolumbar spine. Spinal Cord 38:146-152, 2000
- Blackley HR, Wunder JS, Davis AM, et al: Treatment of giant-cell tumors of long bones with curettage and bone-grafting. J Bone Joint Surg Am 81:811-820, 1999
- Campanacci M, Baldini N, Boriani S, et al: Giantcell tumor of bone. J Bone Joint Surg Am 69:106-114, 1987
- Caudell JJ, Ballo MT, Zagars GK, et al: Radiotherapy in the management of giant cell tumor of bone. Int J Radiat Oncol Biol Phys 57:158-165, 2003
- Chen LH, Niu CC, Lai PL, et al: Recurrent giant cell tumor of the thoracic spine with bilateral pulmonary metastases. J Formos Med Assoc 103:957-961, 2004
- Cheng JC, Johnston JO: Giant cell tumor of bone. Prognosis and treatment of pulmonary metastases. Clin Orthop Relat Res (338):205-214, May 1997
- Cooper AS, Travers B: Surgical Essays. London: Cox Longman & Co., 1818
- Dahlin DC: Giant-cell tumor of vertebrae above the sacrum: A review of 31 cases. Cancer 39:1350-1356, 1977
- Dahlin DC, Cupps RE, Johnson EW Jr: Giant-cell tumor: A study of 195 cases. Cancer 25:1061-1070, 1970
- Doita M, Marui T, Nishida K, et al: Anterior spinal artery syndrome after total spondylectomy of T10, T11, and T12. Clin Orthop Relat Res (405): 175-181, December 2002
- Fidler MW: Surgical treatment of giant cell tumours of the thoracic and lumbar spine: Report of nine patients. Eur Spine J 10:69-77, 2001
- Goldenberg RR, Campbell CJ, Bonfiglio M: Giantcell tumor of bone. An analysis of two hundred and eighteen cases. J Bone Joint Surg Am 52:619-664, 1970
- Hart RA, Boriani S, Biagini R, et al: A system for surgical staging and management of spine tumors. A clinical outcome study of giant cell tumors of the spine. Spine 22:1773-1782, 1997
- Hwang G-J, Kim K-N, Yoon D-H, et al: Total spondylectomy for giant cell tumor of cervical spine. J Korean Neurosurg Soc 34:262-264, 2003
- Kawahara N, Tomita K, Matsumoto T, et al: Total en bloc spondylectomy for primary malignant vertebral tumors. Chir Organi Mov 83:73-86, 1998
- Khan DC, Malhotra S, Stevens RE, et al: Radiotherapy for the treatment of giant cell tumor of the spine: A report of six cases and review of the literature. Cancer Invest 17:110-113, 1999
- Lausten GS, Jensen PK, Schiodt T, et al: Local recurrences in giant cell tumour of bone. Longterm follow up of 31 cases. Int Orthop 20:172-176, 1996
- Lubicky JP, Patel NS, DeWald RL: Two-stage spondylectomy for giant cell tumor of L4. A case report. Spine 8:112-115, 1983
- Malone S, O’Sullivan B, Catton C, et al: Longterm follow-up of efficacy and safety of megavoltage radiotherapy in high-risk giant cell tumors of bone. Int J Radiat Oncol Biol Phys 33:689-694, 1995
- Marmor E, Rhines LD, Weinberg JS, et al: Total en bloc lumbar spondylectomy. Case report. J Neurosurg 95:264-269, 2001
- Miszczyk L, Wydmanski J, Spindel J: Efficacy of radiotherapy for giant cell tumor of bone: Given either postoperatively or as sole treatment. Int J Radiat Oncol Biol Phys 49:1239-1242, 2001
- Prosser GH, Baloch KG, Tillman RM, et al: Does curettage without adjuvant therapy provide low recurrence rates in giant-cell tumors of bone? Clin Orthop Relat Res (435): 211-218, June 2005
- Rosai J, Ackerman LV: Ackerman’s Surgical Pathology 8th ed. New York: Elsevier Science, 1996
- Sanjay BK, Sim FH, Unni KK, et al: Giant-cell tumours of the spine. J Bone Joint Surg Br 75:148-154, 1993
- Shikata J, Yamamuro T, Shimizu K, et al: Surgical treatment of giant-cell tumors of the spine. Clin Orthop Relat Res (278): 29-36, May 1992
- Shimizu K, Ido K, Fujio K, et al: Total spondylectomy and spinal shortening for giant-cell tumour of spine. Lancet 348:342, 1996
- Stener B, Johnsen OE: Complete removal of three vertebrae for giant-cell tumour. J Bone Joint Surg Br 53:278-287, 1971
- Su YP, Chen WM, Chen TH: Giant-cell tumors of bone: An analysis of 87 cases. Int Orthop 28:239-243, 2004
- Tomita K, Kawahara N, Baba H, et al: Total en bloc spondylectomy. A new surgical technique for primary malignant vertebral tumors. Spine 22:324-333, 1997
- Turcotte RE, Wunder JS, Isler MH, et al: Giant cell tumor of long bone: A Canadian Sarcoma Group study. Clin Orthop Relat Res (397): 248-258, April 2002
- Yoshida H, Akeho M, Yumoto T: Giant cell tumor bone. Enzyme histochemical, biochemical and tissue culture studies. Virchows Arch A Pathol Anat Histol 395:319-330, 1982
