
Myelomeningocele Repair
Author
W. Bruce Cherny, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Abstract
The technique for repairing myelomeningoceles is reviewed.
Key Words : myelomeningocele, spina bifida

Spina bifida may be associated with a wide range of meningeal and neural herniations that varies from a small outpouching of the meninges to complete rachischisis. Meningoceles and myelomeningoceles (Fig. 1) pre sent with a great variety of locations, forms, sizes, and coverings.
Neurological function varies from complete paralysis below the level of the lesion to patients being neurologically intact. The most common location for these congenital anomalies is over the lumbo sacral region. These children may also have many other congenital abnormalities.
In most instances, myelodysplasia should be treated surgically as soon after birth as possible, irrespective of whether the meningocele has ruptured. The goals of surgery are to protect the neural elements, to remove excess skin tissue, and to obtain a watertight dural closure to prevent infection without exacerbating neurological deficits.

Technique
After general anesthesia has been induced, the baby is placed prone on the operating table with the head slightly lower than the back so that the cerebrospinal fluid will not be replaced by air (Fig. 2). The operative site is cleaned appropriately. The myelomeningocele is irrigated well with warm sterile saline, and the surrounding skin is cleansed with Betadine (Purdue Frederick Co., Norwalk, CT) or Hibiclens (Zeneca Pharmaceuticals, Wilmington, DE). Betadine and Hibiclens are neurotoxic and should not be placed directly on the exposed neural placode. The anus is sealed off from the operative field by proper draping. The drapes are applied with a generous area exposed so that extensive skin flaps can be mobilized.
The skin incision is sketched on the baby’s back. Vertical extensions are planned to undermine the skin and to achieve a midline closure, if possible. The skin is incised immediately adjacent to the exposed meninges (Fig. 3). Even if the skin extends well on to the dome of the lesion, it should be preserved. Redundant skin is excised later. The incision is carried down and often into the meningeal sac, initially in an area free of neural elements. The skin edges are retracted laterally. In the wall of the sac, nerve roots that course back into the spinal canal are mobilized. Some neural elements are atretic and terminate in the sac itself and may be sacrificed. The edges of the neural placode are then folded and sutured with interrupted 6-0 monofilament nylon (Fig. 4) to reanimate (restore) the configuration of the spinal cord. Within the spinal canal, the filum terminale can often be identified. It should be cut sharply to release the associated tethering of the spinal cord.

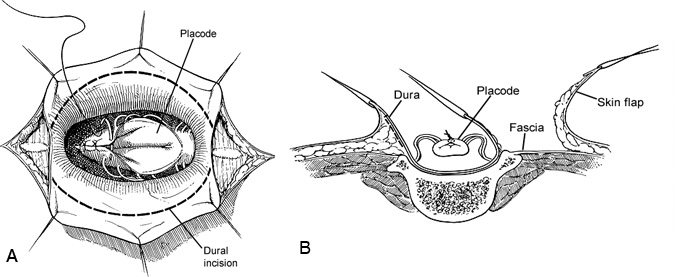
The dura is then dissected from the subcutaneous tissue and lumbosacral fascia (Fig. 4). A watertight closure is essential and can be verified by the anesthesiologist performing a Valsalva maneuver on the patient. To reinforce the dural suture line, the paravertebral muscles and fascia are mobilized to close in the midline, if possible, and to reestablish their proper dorsal position relative to the vertebral elements (Fig. 5). Alternatively, semilunar flaps of lumbosacral fascia can be swung across the midline and sutured to the base of the opposite side (Fig. 6). The skin margins are undermined to the extent that the wound can be reapproximated without tension, often far out to the lateral flank areas bilaterally. Placement of small subcutaneous drains bilaterally along the flank is optional and helps prevent seromas that might be confused with cerebrospinal fluid leakage from the spinal column (1 to 2 days of drainage is adequate). A layer of absorbable, undyed suture is used to close the subcutaneous dissection.


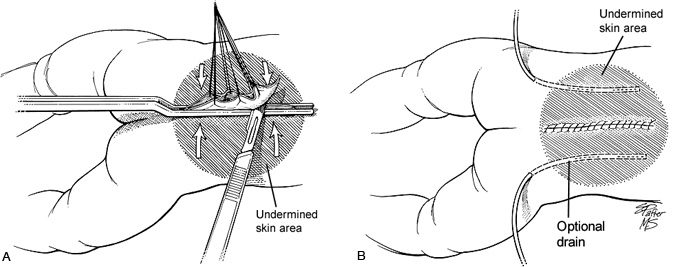
Nylon is used to suture the skin and is left in place about 10 days (Fig. 7B). The dressing must remain dry and the wound isolated from feces. The child is nurtured prone or lateral 3 to 4 days after surgery to avoid undue pressure on the fresh surgical wound and to allow dependent drainage of urine and feces.
