
Vertebral Hemangioma with Unexpected Juxtaposed Plasma Cell Neoplasm Treated with Intralesional Ethanol as a Preoperative Adjunct: Case Report
Authors
Dean G. Karahalios, MD**
Nicholas Theodore, MD***
Allan D.O. Levi, MD, PhD****
Stephen W. Coons, MD*
Cameron G. McDougall, MD
Volker K.H. Sonntag, MD
Divisions of Neurological Surgery and *Neuropathology, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Current Address:
**Evanston Hospital, Evanston, Illinois
***Naval Medical Center San Diego, San Diego, California
****University of Miami, Miami, Florida
Abstract
A 38-year-old man complained of severe back pain but had a normal neurological examination. Radiographic studies demonstrated compression of the T12 vertebral body with associated spinal canal compromise and kyphosis as well as features consistent with a vertebral hemangioma. The patient underwent angiography with embolization of the lesion followed by computed tomography-guided intralesional sclerotherapy, an anterior decompression via a combined transthoracic and retroperitoneal approach, and reconstruction and fixation. Intraoperatively, the lesion was significantly devascularized, which greatly facilitated its safe removal. The patient recovered well from surgery. The final pathologic diagnosis confirmed the presence of the vertebral hemangioma and, unexpectedly, a juxtaposed plasma cell tumor. The patient was referred to medical oncology to rule out multiple myeloma or systemic disease and to plan further treatment. Minimally invasive techniques are effective treatments for symptomatic vertebral hemangiomas. However, when patients meet criteria for surgical intervention, these techniques also can play a significant role as adjuncts to surgery. The classic appearance of a vertebral hemangioma may disguise additional underlying pathology. In planning conservative nonsurgical management of symptomatic vertebral hemangiomas, one might consider performing biopsies despite a low index of suspicion for a coexistent malignancy.
Key Words: intralesional ethanol, plasma cell neoplasm, vertebral hemangioma
This report describes the treatment of a patient who was thought to harbor a symptomatic vertebral hemangioma with associated vertebral collapse, kyphosis, and spinal canal compromise.
The case is interesting because intralesional ethanol sclerotherapy and endovascular embolization were used as preoperative adjuncts to surgery. Unexpectedly, a plasma cell tumor was found juxtaposed to the vertebral hemangioma.
This coincidental finding is exceedingly rare but not completely surprising. The incidence of vertebral hemangiomas is relatively high (10 to 12%),[8,38,43,46] and plasma cell tumors are the most common primary malignant neoplasms of the adult spine.[7]
Case Report
A 38-year-old Brazilian man presented with severe back pain that persisted after he had sustained an injury 6 months earlier while playing squash. With coughing, sneezing, or the Valsalva maneuver, pain radiated into his right lower extremity. He denied numbness, weakness, or bowel and bladder dysfunction.
Otherwise, the patient was healthy and took no medications. A detailed neurological examination revealed no evidence of radiculopathy or myelopathy. There was no tenderness to palpation over the spine, but the pain restricted his movement.
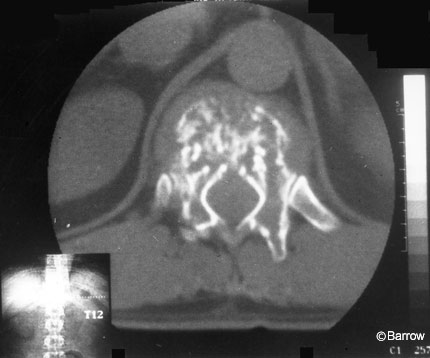
Plain radiography showed compression of the T12 vertebral body with significant kyphosis. Computed tomography (CT) demonstrated an enhancing lesion predominantly involving the anterior elements. Its trabeculated and “honeycomb-like” pattern was classic for a vertebral hemangioma (Fig. 1).
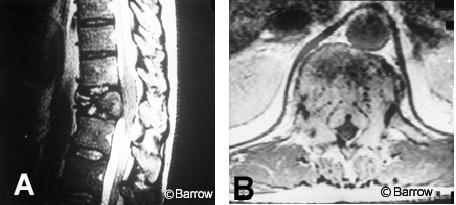
On magnetic resonance (MR) imaging (Fig. 2A), the heterogeneously enhancing mass involved the T12 vertebral body. The lesion extended into the ventral spinal canal and compressed the spinal cord. Axial MR images (Fig. 2B) showed flow voids within the lesion ventrally and also involving the posterior elements. These findings were consistent with the diagnosis of vertebral hemangioma.
Routine preoperative laboratory studies were unremarkable except that urinalysis revealed occult blood and 1+ protein. Liver enzyme studies were mildly elevated.

Preoperative Endovascular and Intralesional Treatments
The vascular character of the presumptive hemangioma indicated that a preoperative attempt to decrease the vascularity of the lesion might facilitate resection and decrease blood loss during surgery. Selective spinal angiography was performed with a 6-French introducer sheath, Bentson guide wire, and a 5-French Cobra-2 catheter (Cook, Bloomington, IN). The artery of Adamkiewicz was identified at T9 on the left. The hemangioma appeared to be supplied primarily and bilaterally by the T12 radicular arteries (Fig. 3A). At each level the subcostal arteries were occluded with 3- to 5-mm straight-fibered platinum coils (Target Therapeutics, Fremont, CA). Next, provocation tests were performed by injecting lidocaine proximally into the vascular pedicles. No neurological sequelae ensued. Polyvinyl alcohol (Target Therapeutics, Fremont, CA) particles (250-350 microns) were used to embolize the vascular supply to the lesion to stasis. Finally, selective catheterizations and angiographic runs were performed bilaterally at T11-L1 to ensure that the collateral vessels had not replaced the embolized T12 pedicles. There was no significant residual blood supply to the lesion (Fig. 3B).
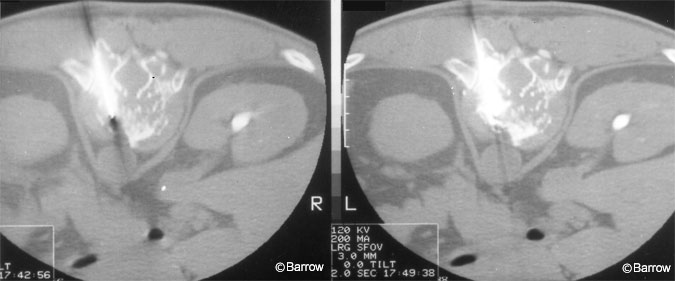
The patient was brought to the CT suite for intralesional therapy. Under CT guidance, a 16-gauge Jeremiah needle (Cook, Bloomington, IN) was advanced into the vertebral body of T12 via a transpedicular approach (Fig. 4). No blood was aspirated from the lesion. Contrast media was injected to confirm intralesional distribution and the absence of extravasation into the spinal canal or surrounding tissues. Ethanol mixed with contrast was infused into the lesion using the distribution of the contrast within the lesion as an indication of adequate coverage. This procedure was performed bilaterally. The patient tolerated the procedures well and experienced no neurological or other complications. The next day he underwent surgery.
Operative Technique
Given the degree of vertebral compression, spinal canal compromise, and kyphosis suggesting instability, the patient was an appropriate candidate for decompression and tumor resection followed by reconstruction and fixation. An anterior approach was selected because most of the pathology was located ventrally.
A left-sided thoracotomy and retroperitoneal dissection were performed to expose the ventrolateral surface of the spine at the thoracolumbar junction. The T12 vertebral body was identified by its abnormal appearance, and the vertebral level was confirmed radiographically.
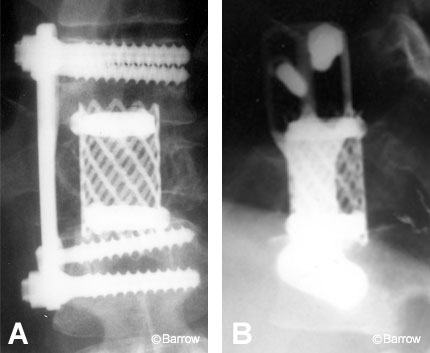
A standard T12 corpectomy, including diskectomies at T11-12 and T12-L1, was performed. The lesion was relatively soft and avascular. After decompression, the corpectomy site was reconstructed with a Harm’s cage (Depuy Motech, Warsaw, IN) packed with autologous bone graft material. An anterior screw plate system (Z-plate; Sofamor Danek, Memphis, TN) was used to fixate the construct (Fig. 5). The length of surgery was about 7 hours, and the estimated blood loss was 1 L. The patient tolerated the procedure well and experienced no neurologic or other complications.
Pathology
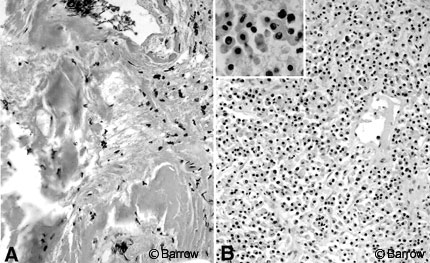
Intraoperatively, the frozen-section diagnosis was consistent with hemangioma. Paraffin sections of additional resected tissue also showed a plasma cell tumor. Histologically, part of the lesion consisted of a network of dilated vascular channels filled with amorphic or poorly cellular eosinophilic material, surrounded by extensively homogenized collagen and a lymphoid infiltrate (Fig. 6A).
This portion of the lesion was considered consistent with a vertebral hemangioma after embolization and intralesional sclerotherapy. Another specimen showed sheets of plasma cells with typical abundant eosinophilic cytoplasm, mild atypia, and occasional binucleate cells (Fig. 6B). Focal necrosis was also identified. This specimen was consistent with the diagnosis of plasma cell tumor.
Postoperative Course
Postoperatively, plain radiography and CT confirmed good decompression of the spinal canal and appropriate placement of the instrumentation (Figs. 5 and 7). The thoracostomy tube was removed on the second postoperative day, allowing the patient to be mobilized in a thoracolumbosacral orthosis. Upright and supine plain radiographs of the spine with the orthosis in place showed no instability. The patient was discharged on the seventh postoperative day.

The patient was referred to a medical oncologist for further evaluation and treatment of the plasma cell tumor. He denied any history of anemia, infections, bleeding disorders, renal failure, or other mass lesions. Despite the patient’s relatively young age, additional studies were obtained to determine whether the lesion was a solitary plasmacytoma or, less likely, a manifestation of multiple myeloma. A skeletal survey was negative for additional lesions. A 24-hour urine specimen contained 1051 mg of protein (normal range, 40 to 150 mg) with 97% globulin and 3% albumin. Electrophoresis demonstrated a faint monoclonal spike secondary to k light chains. IgG was 599 mg/dl (normal range, 690 to 1615 mg/dl) and IgA was 100 mg/dl (normal range, 68 to 378 mg/dl). Serum (beta)2 microglobulin was 2.5 mg/l (normal range, 1.1 to 2.4 mg/l). A bone marrow biopsy was recommended, but the patient elected to return to Brazil for further evaluation and treatment.
These findings raised suspicions that the patient had multiple myeloma for which he would need chemotherapy rather than a solitary plasmacytoma that could be treated with local radiation therapy alone.
Discussion
Vertebral hemangiomas are the most common benign neoplasms involving the spine.[8,13,21,38,43,46] They are usually asymptomatic[13,25,40] and often found incidentally on radiographic studies. Their classic radiographic appearance makes diagnosis straightforward. On plain radiographs, dense vertical striations or trabeculations are prominent. On CT, a “polka-dot” or “honeycomb” appearance of the involved bone is usually striking.[5,8,13,26,39]
If asymptomatic, vertebral hemangiomas can be followed. They usually remain asymptomatic and require no treatment,[13,25,40] and there appears to be no risk of malignant degeneration.[11] For symptomatic lesions, a number of therapeutic modalities are available depending on the severity of symptoms. Patients with only pain may be followed.[8,13] If the pain is severe, radiation therapy[11,13,16,35,47] or embolization[36] has been used with success. Patients with neurologic deficits from either nerve root or spinal cord compression have been treated with surgical resection and decompression, radiation therapy, endovascular embolization, intralesional sclerotherapy, or combinations of these modalities.[1,2,4,6,8-13,16-22,25,27,28,30-32,35-38,40,41,44,47]
The main risks of surgery are excessive intraoperative blood loss and postoperative epidural hematoma.[4,5,12,13,17,22,25,41] Preoperative embolization significantly decreases the vascularity of hemangiomas, facilitating their safe removal by minimizing intraoperative blood loss.[1,2,8,10,13,18,21,22,27,28,31,32,37,38,44] However, recanalization can follow initially successful embolization of feeding vessels.[2,3,17,21,36,44] If surgery is planned, it should follow embolization immediately to avoid reperfusion of the lesion.
Intralesional sclerotherapy is also an effective treatment for vertebral hemangiomas. For example, two patients with myelopathy due to compression from vertebral hemangiomas underwent intralesional injections of ethanol in lieu of surgery.[19] In both cases, tumoral compression of the spinal cord resolved radiographically as did the patients’ myelopathy. The authors concluded that this technique may be a useful alternative to surgery or radiation treatment.
Methylmethacrylate can also be injected intralesionally to treat painful vertebral hemangiomas.[14,15] It also may help stabilize associated compression fractures. However, the methylmethacrylate does not destroy the hemangioma, which can continue to grow and worsen symptoms.[19] Unlike ethanol, which shrinks the lesion and may reverse neural compression, acrylic forms a cast that can exacerbate spinal cord compression.[15,19,33] Consequently, this treatment was deemed inappropriate for our patient.
Our patient required surgery because the lesion was associated with such severe spinal pathology. We used intralesional sclerotherapy as an adjunct to surgery to reinforce or extend the devascularization afforded by embolization and to avert any possibility of recanalization before surgery. The lesion may already have been sufficiently devascularized before the intralesional treatment, especially given that blood could not be aspirated from the lesion before the ethanol injection. The intralesional treatment alone also might have been sufficient to devascularize the lesion before surgery. Given the tendency for recanalization, however, and the high risk of hemorrhage associated with hemangiomas, we combined the modalities to insure maximal devascularization. As a preoperative adjunct, intralesional therapy might be more beneficial if embolization is incomplete or contraindicated because of the possibility of compromising the blood supply to the spinal cord.[36] Based on our limited experience, we would recommend combining embolization and intralesional ethanol treatments when possible to minimize intraoperative blood loss from these dangerous lesions.
When surgery is necessary for either hemangiomas or plasma cell lesions, the approach is directed by the location of the compressive pathology. Because most of these lesions involve the vertebral body, anterior or anterolateral approaches are usually indicated.[12,13,17,21,22,31,40,41] Less commonly, a posterior approach with laminectomy is indicated if the pathology and compression are based dorsally,[13,31] if the lesion involves the vertebral body without bony expansion but with a lateral soft-tissue component,[13] if an extensive lesion leads to circumferential compression,[13,25,28,31] or if compression causes rapid neurological deterioration.[6,13,25,31] A posterior approach rarely destabilizes the spine. However, extensive dissection laterally or into the pedicles can cause spinal instability that requires fixation.[13]
On spinal radiographs, plasma cell tumors, whether solitary or manifestations of multiple myeloma, appear as lytic lesions.[7,23,34] Like hemangiomas, they usually involve the vertebral body and may be associated with pathologic fractures, extra-osseous soft-tissue extensions, or both.[7] For both solitary lesions and multiple myeloma, pain is usually the presenting symptom. Solitary plasmacytomas, which represent about 3% of plasma cell neoplasms,[23,24] are usually diagnosed by needle biopsy[7,23,42] and are treated with radiotherapy.[7,23,24,29,45] Multiple myeloma is treated with systemic chemotherapy.[23] Symptomatic spinal lesions of either type may be treated with radiation or surgical decompression if necessary.[7,23,24,29]
From a surgical perspective, the finding of a coincidental plasma cell tumor did not change the management of our patient. The preoperative embolization was appropriate for devascularizing the plasma cell tumor,[23] which also is hypervascular and associated with excessive intraoperative blood loss. Postoperatively, radiation therapy would be appropriate for either residual hemangioma or plasma cell tumor.[6-8,10,13,14,23-25,28-30,45]
What differs in the management of these two lesions is the evaluation required to rule out systemic disease in the latter case. Notably, the plasma cell tumor could have been missed had the lesion, which originally was thought to be a hemangioma alone, been treated nonsurgically. Percutaneous vertebral biopsy has been shown to be efficacious and associated with a low rate of morbidity.[42] Thus, a biopsy of all symptomatic vertebral lesions might be considered despite a low index of suspicion for malignancy.
References
- Bell RL: Hemangioma of a dorsal vertebra with collapse and compression myelopathy. J Neurosurg 12:570-576, 1955
- Benati A, Da Pian R, Mazza C, et al: Preoperative embolisation of a vertebral haemangioma compressing the spinal cord. Neuroradiology 7:181-183, 1974
- Berenstein A, Russell E: Gelatin sponge in therapeutic neuroradiology: A subject review. Radiology 141:105-112, 1981
- Bergstrand A, Höök O, Lidvall H: Vertebral haemangiomas compressing the spinal cord. Acta Neurol Scand 39:59-66, 1963
- Blankstein A, Spiegelmann R, Shacked I, et al: Hemangioma of the thoracic spine involving multiple adjacent levels: Case report. Paraplegia 26:186-191, 1988
- Bremnes RM, Hauge HN, Sagsveen R: Radiotherapy in the treatment of symptomatic vertebral hemangiomas: Technical case report. Neurosurgery 39:1054-1058, 1996
- Cahill DW: Malignant tumors of the bony spine, in Menezes AH, Sonntag VKH (eds): Principles of Spinal Surgery. New York: McGraw-Hill, 1996, pp 1401-1421
- Dagi TF, Schmidek HH: Vascular tumors of the spine, in Sundaresan N, Schmidek HH, Schiller AL, et al (eds): Tumors of the Spine: Diagnosis and Clinical Management. Philadelphia: W.B. Saunders, 1990, pp 181-191
- Eisenstein S, Spiro F, Browde S, et al: The treatment of a symptomatic vertebral hemangioma by radiotherapy. A case report. Spine 11:640-642, 1986
- Esparza J, Castro S, Portillo JM, et al: Vertebral hemangiomas: Spinal angiography and preoperative embolization. Surg Neurol 10:171-173, 1978
- Faria SL, Schlupp WR, Chiminazzo H, Jr.: Radiotherapy in the treatment of vertebral hemangiomas. Int J Radiat Oncol Biol Phys 11:387-390, 1985
- Feuerman T, Dwan PS, Young RF: Vertebrectomy for treatment of vertebral hemangioma without preoperative embolization. J Neurosurg 65:404-406, 1986
- Fox MW, Onofrio BM: The natural history and management of symptomatic and asymptomatic vertebral hemangiomas. J Neurosurg 78:36-45, 1993
- Galibert P, Deramond H: Percutaneous acrylic vertebroplasty as a treatment of vertebral angioma as well as painful and debilitating disease [French]. Chirurgie 116:326-335, 1990
- Galibert P, Deramond H, Rosat P, et al: Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty [French]. Neurochirurgie 33:166-168, 1987
- Glanzmann C, Rust M, Horst W: Irradiation therapy of vertebral angiomas: Results in 62 patients during the years 1939 to 1975 [German]. Strahlentherapie 153:522-525, 1977
- Graham JJ, Yang WC: Vertebral hemangioma with compression fracture and paraparesis treated with preoperative embolization and vertebral resection. Spine 9:97-101, 1984
- Gross CE, Hodge CH, Jr., Binet EF, et al: Relief of spinal block during embolization of a vertebral body hemangioma. Case report. J Neurosurg 45:327-330, 1976
- Heiss JD, Doppman JL, Oldfield EH: Relief of spinal cord compression from vertebral hemangioma by intralesional injection of absolute ethanol. N Engl J Med 331:508-511, 1994
- Hekster RE, Lyuendijk W, Tan TI: Spinal-cord compression caused by vertebral haemangioma relieved by percutaneous catheter embolisation. Neuroradiology 3:160-164, 1972
- Hemmy DC: Vertebral hemangiomas, in Wilkins RH, Rengachary SS (eds): Neurosurgery. New York: McGraw-Hill, 1985, pp 1076-1079
- Hemmy DC, McGee DM, Armbrust FH, et al: Resection of a vertebral hemangioma after preoperative embolization. Case report. J Neurosurg 47:282-285, 1977
- Kempin S, Sundaresan N: Disorders of the spine related to plasma cell dyscrasias, in Sundaresan N, Schmidek HH, Schiller AL, et al (eds): Tumors of the Spine. Diagnosis and Clinical Management. Philadelphia: W.B. Saunders, 1990, pp 214-225
- Knowling MA, Harwood AR, Bergsagel DE: Comparison of extramedullary plasmacytomas with solitary and multiple plasma cell tumors of bone. J Clin Oncol 1:255-262, 1983
- Krueger EG, Sobel GL, Weinstein C: Vertebral hemangioma with compression of spinal cord. J Neurosurg 18:331-338, 1961
- Laredo JD, Reizine D, Bard D, et al: Vertebral hemangiomas: Radiologic evaluation. Radiology 161:183-189, 1986
- MacErlean DP, Shanik DG, Martin EA: Transcatheter embolisation of bone tumour arteriovenous malformations. Br J Radiol 51:414-419, 1978
- McAllister VL, Kendall BE, Bull JW: Symptomatic vertebral haemangiomas. Brain 98:71-80, 1975
- Mill WB, Griffith R: The role of radiation therapy in the management of plasma cell tumors. Cancer 45:647-652, 1980
- Mohan V, Gupta SK, Tuli SM, et al: Symptomatic vertebral haemangiomas. Clin Radiol 31: 575-579, 1980
- Nguyen JP, Djindjian M, Gaston A, et al: Vertebral hemangiomas presenting with neurologic symptoms. Surg Neurol 27:391-397, 1987
- Nguyen JP, Djindjian M, Pavlovitch JM, et al: Vertebral hemangioma with neurologic signs. Therapeutic results. Survey of the French Society of Neurosurgery [French]. Neurochirurgie 35:299-303, 1989
- Nicola N, Lins E: Vertebral hemangioma: Retrograde embolization-stabilization with methyl methacrylate. Surg Neurol 27:481-486, 1987
- Paul LW, Pohle EA: Solitary myeloma of bone. A review of the roentgenologic features, with a report of four additional cases. Radiology 35:651-666, 1940
- Pavlovitch JM, Nguyen JP, Djindjian M, et al: Radiotherapy of vertebral hemangioma with neurologic complications (French). Neurochirurgie 35:296-298, 1989
- Picard L, Bracard S, Roland J, et al: Embolization of vertebral hemangioma. Technic-indications-results [French]. Neurochirurgie 35:289-293, 1989
- Raco A, Ciappetta P, Artico M, et al: Vertebral hemangiomas with cord compression: The role of embolization in five cases. Surg Neurol 34:164-168, 1990
- Reizine D, Laredo JD, Riche MC, et al: Vertebral hemangiomas, in Jeanmart L (ed): Radiology of the Spine. Tumors. Berlin: Springer-Verlag, 1986, pp 73-80
- Ross JS, Masaryk TJ, Modic MT, et al: Vertebral hemangiomas: MR imaging. Radiology 165: 165-169, 1987
- Roy-Camille R, Monpierre H, Saillant G, et al: Role of surgical resection in the treatment of vertebral hemangioma [French]. Neurochirurgie 35:294-295, 1989
- Ryopy S, Poussa M, Heiskanen O, et al: Resection of a thoracic vertebra for hemangioma–operation under deep hypothermia and circulatory arrest. A case report. J Bone Joint Surg Am 72:1245-1249, 1990
- Schajowicz F, Hokama J: Aspiration (puncture of needle) biopsy in bone lesions. Recent Results Cancer Res 54:139-144, 1976
- Schmori G, Junghanns H: The Human Spine in Health and Disease. New York: Grune & Stratton, 1971
- Smith TP, Koci T, Mehringer CM, et al: Transarterial embolization of vertebral hemangioma. J Vasc Interv Radiol 4:681-685, 1993
- Tong D, Griffin TW, Laramore GE, et al: Solitary plasmacytoma of bone and soft tissues. Radiology 135:195-198, 1980
- Topfer DI: Uber ein infiltrierend wachsendes Hämangiom der Haut und multiple Kapillarektasien der Haut und inneren Organe: Zur Kenntnis der Wirbelangiome. Frankf Z Pathol 36:337-345, 1928
- Yang ZY, Zhang LJ, Chen ZX, et al: Hemangioma of the vertebral column. A report on twenty-three patients with special reference to functional recovery after radiation therapy. Acta Radiol Oncol 24:129-132, 1985
