The Neuropsychological Examination of Children with Hypothalamic Hamartomas: Preliminary Observations
George P. Prigatano, PhD
Camia Gagliardi, MEd
Jennifer Wethe, PhD
Susan Borgaro, PhD
Division of Neurology, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Abstract
In this pilot investigation, six children with a hypothalamic hamartoma were compared to six asymptomatic children with a history of mild traumatic brain injury (TBI). Based on the BNI Screen for Children (BNIS-C) and selected subtests of the Wechsler Intelligence Scale for Children (3rd ed), the performance of all but one child with a hypothalamic hamartoma was impaired. In contrast, the neuropsychological performances of the six children with a history of mild TBI were normal. Children with a hypothalamic hamartoma showed a special vulnerability for performing poorly on tests sampling speech and language function. They also had difficulty generating affect and perceiving facial affect, behaviors not previously documented. Guidelines for the neuropsychological examination of hypothalamic hamartoma children are suggested.
Key Words: BNI Screen for Children, hypothalamic hamartoma, neuropsychological tests
The neuropsychiatric and neuropsychological literature on children diagnosed with a hypothalamic hamartoma emphasizes two points. First, these children show considerable variability in neuropsychological disturbances. Second, without treatment, the cognitive and/or psychiatric status of these children often deteriorates.[2,4]
The literature on the neuropsychological examination of children with a hypothalamic hamartoma has reported the results of standardized tests of intelligence and academic achievement.[6,7] However, a number of neuropsychological disturbances may not be captured by these traditional measures. For example, Berkovic and colleagues[2] have observed that children with a hypothalamic hamartoma often show a variety of neurocognitive deficits with no underlying consistent pattern. Methods or guidelines for assessing the neuropsychological disturbances in these children are lacking.
This preliminary report outlines what we consider to be a brief but reliable approach to assessing these children’s neuropsychological difficulties. The initial observations from six children with a hypothalamic hamartoma (and six neurological controls) studied using a newly standardized test called the BNI Screen for Children (BNISC) and related subtests from the Wechsler Intelligence Scale for Children (3rd ed.,WISC-III) are reported.
Neuropsychological Evaluation
The neuropsychological examination of children involves at least four challenges. First, the neuropsychological measures used must be sensitive to developmental changes. Otherwise, children of different ages cannot be examined meaningfully. Second, tests should sample a wide variety of cognitive and noncognitive (affective) factors important for adaptation and learning. Third, tests must be sensitive to brain disorders, or it is difficult to determine if poor performance on different tests (e.g., intelligence tests) represents an impaired psychiatric status or an actual neuropsychological impairment. Fourth, tests should provide information that is useful in managing the child and monitoring changes. This last requirement becomes especially important for the pre- and postoperative assessment of these children.
Children often cannot tolerate lengthy examinations, especially children who have problems with impulse control and a propensity for rage reactions. Consequently, the examination must be brief and must engage children enough so that their abilities and behavior can be estimated reliably. Finally, as with all neuropsychological instruments, the information provided must be compared meaningfully to a reference or “control” group. Thus, the test must be standardized, and normative data must be available on which to base statements concerning the child’s neuropsychological status.
With these guidelines in mind, we selected tests that could sample a wide range of abilities within one or two hours. When children (and adults) are examined, their ability to follow verbal (and auditory) instructions must be assessed first so that the examination can proceed as smoothly as possible. The BNIS-C quickly tests verbal fluency, articulation skills, and auditory comprehension by assessing the capacities to name objects, repeat sentences, read, write, and spell. A child’s ability to perform basic arithmetic operations is also assessed.
Orientation to time and place, basic visuospatial abilities, attention and concentration, and learning and memory skills are then sampled briefly. The ability of children to predict their performance on a memory test is assessed. The BNIS-C also assesses children’s ability to generate affect in their tone of voice, to perceive facial affect, and to show spontaneous affect. The test thereby provides various “subtest” scores as well as a “total” score that can be used to compare a child’s relative strengths and difficulties. It samples both cognitive and noncognitive dimensions.
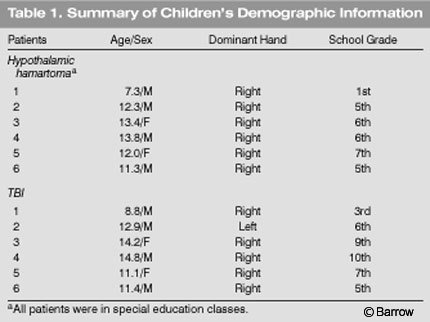
Selected subtests of WISC-III were also administered: the Vocabulary, Block Design, and Digit Symbol Coding subtests. The first two measures provide reasonable estimates of verbal and nonverbal problem-solving skills. The Digit Symbol Coding test measures a number of factors, including the speed of new learning, an ability that is often compromised after brain injury. We also routinely administer the Trail Making tests, Parts A and B, and the Halstead Finger-Tapping test. These tests form our “core” battery. Other tests are administered depending on a child’s ability to tolerate them. This report, however, is limited to our observations on these children’s performance on the BNIS-C and the selected subtests of the WISC-III.
Methods
Six children diagnosed with a hypothalamic hamartoma were compared to six children of a comparable age with a history of mild traumatic brain injury (TBI). The latter were at least 1 year beyond the time of injury and were considered asymptomatic. That is, they and their parents reported no residual cognitive or behavioral problems after their mild TBI. These six children were involved in another study focusing on community reentry after TBI during childhood.
Each child was administered the BNIS-C and three subtests of the WISC-III as described above (Vocabulary, Block Design, and Digit Symbol). The tests were administered either by a board-certified clinical neuropsychologist, a resident in clinical neuropsychology, or a predoctoral student in psychology who was working as a psychometrician.
 Means and standard deviations with appropriate t-tests were calculated and compared.
Means and standard deviations with appropriate t-tests were calculated and compared.
Results
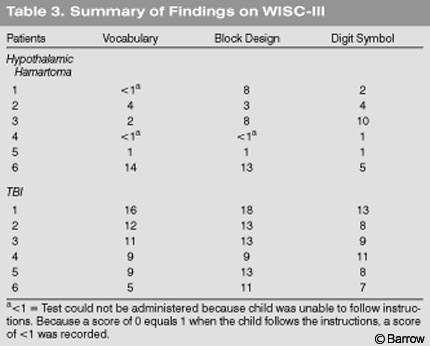
There were four boys and two girls. The ages of the children with a hypothalamic hamartoma ranged from 7 years, 3 months to 13 years, 8 months (mean age, 11 years, 6 months), while the ages of the children with a mild TBI ranged from 8 years, 8 months to 14 years, 8 months (mean age, 12 years, 2 months). There was no statistical difference in mean age (t =.393, df =10, p=.70, Table 1).
Each child with a hypothalamic hamartoma was involved in special education classes. In contrast, none of the children with a mild TBI required such educational support. The mean educational level of the former was the fifth grade compared to 6.6 years of education in the latter. Even though the mean difference in grade level was not statistically significant (t =1.27, df =10, p =.248), the educational level of the two groups was clearly different.
The total possible points on the BNIS-C is 50 points. The performance of children with hypothalamic hamartoma varied greatly (Tables 2 and 3). Only one of the six children actually performed normally on the BNIS-C. In contrast, children with a mild TBI performed within the normal range and obtained almost maximum scores on the BNIS-C. In fact, the test was developed so that normal children would perform almost perfectly on each subtest.
The hypothalamic hamartoma children obtained a mean BNIS-C total score of 23.6 points (standard deviation (sd)=14.8) compared to a mean of 42.5 points (sd =1.04) obtained by the children with a mild TBI. The difference was statistically significant (t = 3.0, df =10, p=.02).
In the hypothalamic hamartoma group, three children performed almost normally on the speech and language tasks (13 or more of 15 possible points). However, two of the children who performed normally on these tasks still had exceptionally low vocabulary scores. The performances of the other three children were clearly abnormal. These three children either could not take the Vocabulary subtest of the WISC-III, or their scale score was 1.
Except for Patient 6, most of the children with a hypothalamic hamartoma had difficulty on the other subtests of the BNIS-C. The BNIS-C measures not only cognitive functioning but affective functioning. Only Patient 6 was able to generate affect in his tone of voice and to identify facial affect. These findings document both cognitive and affective disturbances in the children with hypothalamic hamartoma as a group.
None of the children with a hypothalamic hamartoma performed normally on the three subtests of WISCIII. Even Patient 6 showed substantial impairment in the speed of new learning as reflected by his low Digit Symbol subtest score. In contrast, the children with a mild TBI performed within the normal range on both the BNIS-C and WISC-III subtests.
Discussion
The examination of children with known or suspected brain disorders requires reliable and efficient methods of assessment. Children must be engaged in the examination process so that reliable estimates of their ability can be obtained. An axiom of neuropsychological testing is that reliability precedes validity. That is, a wide enough sample of behavior must be obtained for valid conclusions to be drawn.
The present examination of children with a hypothalamic hamartoma using the BNIS-C reveals great variability in their performances. More than 80% of these children showed difficulties in speech and language function, and more than 50% showed unequivocal difficulties on tests of learning and memory. All but one showed significant impairments in the ability to perceive and judge facial affect. Given that the neurological control group had almost no difficulties in any of these areas, these findings are striking.
Not surprisingly, the children with a hypothalamic hamartoma showed difficulties on at least one of the three subtests from the WISC-III. Again, there was great variability. Speed of information processing was normal in some children but not in most. All but one of these children had significant difficulties on the Vocabulary subtest, a finding that highlights the potential vulnerability of speech and language functions in this patient group. In half the patients, visuospatial problem-solving skills were low average to average. This finding was paralleled by observations on the BNIS-C. Language functions appear to be much more at risk than visuospatial functions in these children. However, this pattern is not universal and a more extensive examination of children with a hypothalamic hamartoma with a larger sample size is needed before firm conclusions can be made.[2]
The underlying etiology of these neurocognitive and neuroaffective deficits remains unclear, although various potential mechanisms have been suggested. [3,4] The neuropsychological disturbances may be related to time of seizure onset, the nature of the seizures, and the areas of the brain most affected by abnormal electrical discharges. Interestingly, Patient 6, who had the most “normal” neuropsychological test findings, reportedly had relatively mild gelastic seizures (twice a week). His primary difficulty involved behavioral problems, that is, he was prone to rage reactions. However, his neurocognitive performance revealed no typical abnormalities. This particular child’s examination findings emphasize that the neuropsychological disturbances of these children may be disassociated from their rage reactions.
Other authors have noted the apparent relationship between seizures and cognitive dysfunction in patients with a hypothalamic hamartoma.[2,4] In many patients cognitive function seems to deteriorate over time.[2] Deonna and Ziegler[4] listed several arguments supporting the idea that the cognitive and behavioral symptoms associated with hypothalamic hamartomas with gelastic seizures may be a direct result of the epilepsy. They cited three considerations. First, children with a hypothalamic hamartoma associated with gelastic seizures typically have no history of abnormal development before the onset of epilepsy. Second, the onset of uncontrolled epilepsy is often associated with a standstill or deterioration in cognitive development and significant behavioral problems. Finally, children with a hypothalamic hamartoma associated with precocious puberty, but not with epilepsy, do not manifest the same behavioral and cognitive problems.[1,5] These ideas will need to be evaluated further in more children with this complicated neurological disorder.
References
- Arroyo S, Santamaria J, Sanmarti F, et al: Ictal laughter associated with paroxysmal hypothalamopituitary dysfunction. Epilepsia 38:114-117, 1997
- Berkovic SF, Andermann F, Melanson D, et al: Hypothalamic hamartomas and ictal laughter: Evolution of a characteristic epileptic syndrome and diagnostic value of magnetic resonance imaging. Ann Neurol 23:429-439, 1988
- Berkovic SF, Kuzniecky RI, Andermann F: Human epileptogenesis and hypothalamic hamartomas: New lessons from an experiment of nature. Epilepsia 38:1-3, 1997
- Deonna T, Ziegler AL: Hypothalamic hamartoma, precocious puberty and gelastic seizures: A special model of “epileptic” developmental disorder. Epileptic Disord 2:33-37, 2000
- Diebler C, Ponsot G: Hamartomas of the tuber cinereum. Neuroradiology 25:93-101, 1983
- Frattali CM, Liow K, Craig GH, et al: Cognitive deficits in children with gelastic seizures and hypothalamic hamartoma. Neurology 57:43-46, 2001
- Weissenberger AA, Dell ML, Liow K, et al: Aggression and psychiatric comorbidity in children with hypothalamic hamartomas and their unaffected siblings. J Am Acad Child Adolesc Psychiatry 40:696-703, 2001