Loyal & Edith Davis Neurosurgical Research Laboratory
Laboratory Focus
The Loyal & Edith Davis Neurosurgical Research Laboratory is a world-class facility that mentors, coordinates, and manages neurosurgical, surgical, and medical research, education, and training. Led by Mark C. Preul, MD, our laboratory has been termed the foremost and most productive neurosurgical research laboratory in the world. We are the research facility of the Barrow Department of Neurosurgery and, in that capacity, coordinate research periods and projects for neurosurgery residents and fellows.
Our laboratory has won the Vesalius Prize 16 times since its inception in 2001, more than any other institution.
Our staff collaborates with academic, institutional, and medical industry partners to conduct neurosurgery research projects, science and technology development, testing, and education programs. We manage the logistics of Barrow and corporate-sponsored teaching events, courses, and conferences while serving as liaison for neurosurgery research to other departments and laboratories at Barrow. Our team engages in all phases of medical procedural training and courses for physicians, residents, fellows, medical students, nurses, technicians, industry personnel, and researchers (including applied and basic research, device research, pharmaceutical research, technology research, and biomaterials testing and development).
The laboratory comprises 11,000 square feet of high-throughput, state-of-the-art facilities for the most complex research and training initiatives covering:
- Neurosurgery
- Cardiac surgery
- Endovascular surgery
- Acute and survival surgery
- Technology development and testing
- Image capture
- Neurosurgery neuroanatomy dissection
- Cadaver tissue investigations and training
- Imaging
- Pre-clinical technology testing, development, and project performance, management, and support
We provide these services for industry, federal, and other healthcare or scientific organization’s regulatory approval.
Since 2000, more than 140 neurosurgery research fellows have received training and mentorship in the Loyal and Edith Davis Neurosurgery Research Laboratory. Many have become prominent national and international leaders in the field of neurosurgery. The list of national and international corporate technology partners and projects is long, and spans large to start-up entities.
- 10-station surgery or cadaver teaching laboratory
- Sterile operating suite
- Dedicated endovascular surgery laboratory
- Full performance and support for sterile animal surgery individual training
- Full cadaver tissue capabilities
- Preclinical testing
- FDA study support and product and technology testing in various disciplines
- Complete cadaver preservation, cerebrovascular infusion, and anatomical dissection laboratory
- Operating rooms
- Sterile surgery
- Full operative instrumentation, including microinstrumentation and power instruments
- Operating microscopes
- Full operative physiological data recording
A Miniaturized Valve That Mimics Functional Arachnoid Granulations to Treat Hydrocephalus
Grantees: Jennifer Blain Christen, PhD (ASU Bioengineering), Mark C. Preul, MD (The Loyal and Edith Davis Neurosurgical Research Laboratory)
Collaborator: Ruth Bristol, MD (Phoenix Children’s Department of Neurosurgery)
DOD Grant
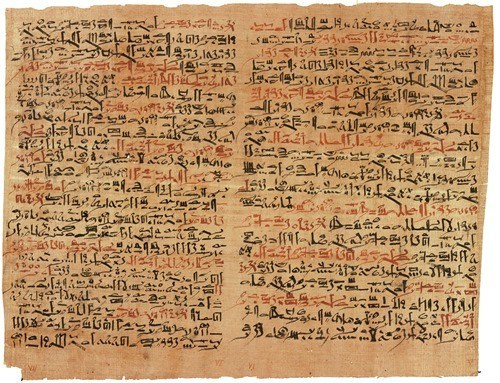
Hydrocephalus (HCP) is a chronic neurological disorder characterized by the inability to automatically adjust the drainage physiology of cerebrospinal fluid (CSF). Nearly 1 in 500 infants born in the United States suffer from hydrocephalus. CSF is a vital supporting liquid that flows through and around the cerebral cortex, functioning as:
- A “cushion” for protecting the brain and spinal cord from external shocks
- A “vehicle” for nutrients necessary for the brain and removing waste
- A “regulator” to adjust intracranial pressures (ICP) by flowing between the cranium and spine
With regard to ICP adjustment, CSF is partially drained through the arachnoid granulations (AG), which act as one-way biological valves from the subarachnoid space (SAS) to the superior sagittal sinus (SSS). In the case of hydrocephalic patients, this draining pathway of AG is disrupted, which causes an imbalance between the amount of produced and drained CSF, leading to excess accumulation of CSF in the ventricles, the subarachnoid space, and other cisternal regions of the brain.
The current standard treatment for HCP is the implantation of a drainage tube, termed a shunt, between the ventricles of the brain and the abdominal cavity or atrium of the heart for providing drainage of excessively accumulated CSF. These are implanted such that an outflow catheter directs CSF away from the ventricle through the skull and into a valve that controls CSF flow into another outflow catheter from the valve, which then directs CSF into distal drainage spaces.
Unfortunately, shunts in current usage have a notoriously high failure rate. Fifty percent of shunts fail within the first two years of implantation, even though shunts are the most popular and primary treatment method for hydrocephalus. The majority of shunt complications are catheter-based occlusion failures. Catheters of an implanted shunt are exposed to blood and cellular debris, both containing proteins that bind to the shunt, which further cause macrophages and monocytes to produce growth factors. Such accumulations of debris can cause clogging of the tubing and valve. Accumulations on the outside of the tubing and valve, in turn, can attract astrocytes and microglia, potentiating an inflammatory response. Generally, occlusion-based shunt failures are caused by foreign body response, infection, and cellular growth. Therefore, a catheter-less approach to reduce the overall implant surface area would be appealing to reduce these complications.
Alternative shunt methods have been studied to improve current shunt systems, including MicroElectroMechanical System (MEMS)-based devices. MEMS valves have been extensively researched and developed, with fluidic valves proposed to control CSF as an implantable valve in various forms, such as cantilever, bridge, perforated membrane, or spherical ball-type valves. However, critical challenges still exist, such as reverse flow leakage, valve deformation in long-term operations, valve stiction, imperfect sealing, etc., leading to low reproducibility and durability of the valves. To overcome these challenges, our earlier work has proposed the hydrogel check valve, meeting the two required features:
- A non-zero cracking pressure (from 20 to 110 mmH2O)
- Negligible reverse flow leakage
However, the previous work suffered from a deficiency in the accurate measurement of fluid pressure across the valve as measured inside the setup and a lack of verification of the valve in realistic environments. First, we have reported a physiologically and biologically realistic evaluation of the hydrogel check-valve to therapeutically manage hydrocephalus and propose a wireless measurement of fluid pressure across the valve, all designed to reduce current problems with shunt management for hydrocephalus. Additionally, we developed a fully passive wireless pressure sensor to measure the pressure applied to the valve. Currently, clinical diagnosis of HCP is based on symptoms such as headache, sleepiness, vomiting, etc., which could be unrelated to HCP if there are other disease processes or comorbidities. Brain imaging usually shows the increased ventricular size, but not always. The intracranial pressure may be measured, and for those that have a valve in place, the valve may be checked for its operational status. If their HCP treatment device is malfunctioning, the ICP range will likely be abnormal, leading to HCP or collapsed CSF spaces (i.e., ventricles). In the worst case, the HCP patients will undergo surgery to interrogate their implanted device, remove it, and, if necessary, replace the valve and tubing. In order to avoid this situation, wireless pressure measurement has distinct potential as a non-invasive and non-surgical method.
Laboratory Director
Mark Preul, MD
Newsome Chair of Neurosurgery Research
Director, Loyal & Edith Davis Neurosurgical Research Laboratory
Barrow Neurological Institute

Contact Information
For information on educational opportunities, training, technology testing, or bioskills courses, please contact:
William Bichard
William.Bichard@DignityHealth.org
(602) 406-3268
Overview
Since 1999, more than 140 research fellows have been in residence at The Loyal and Edith Davis Neurosurgical Research Laboratory at Barrow Neurological Institute. The fellowship is a laboratory-based fellowship, not a clinical neurosurgery fellowship, and is not a combined laboratory-clinical fellowship. The position is for one year minimum, with additional time contingent on appropriate performance and supervisor review during the year and adequate funding. Foreign fellows are processed through the human resources and visa department of St. Joseph’s Hospital and Medical Center, and the hospital reserves the right to refuse visa sponsorship. Senior neurosurgery residents, fellows, or recently graduated neurosurgeons are preferred applicants, although this will depend upon the record of the applicant, or special needs of the laboratory according to Dr. Preul.
Regular clinical contact or exposure, such as clinical rounding or clinic duties or observation with patients, is not included in the fellowship. Research work may allow observation of surgery, but such observation of surgery is within the scope of a research project and is not to be construed as a constant clinical neurosurgery observership position. Research within the our laboratory spans neurosurgical anatomical science and cadaveric dissection and basic or applied projects in neurosurgery, neuroscience, and research and development into medical and surgical technology. The fellowship time is devoted to research that is within the laboratory, but also may entail appropriate and related clinical research.
The laboratory is one of the finest equipped facilities in the world for dedicated cadaveric, animal, and technology research with surgical instruments, power instrumentation, large operating rooms including an endovascular operating room, c-arm angiography, endoscopic instrumentation, laboratory support staff, and connection with the other laboratories at Barrow and many other institutions. Dr. Preul directs, supervises, and mentors the projects and fellows. There will be assistance on projects and work with other neurosurgery clinical staff, such as Dr. Lawton, fellows, and residents.
The expectation for the fellow is to produce the highest level of neurosurgery research work that is authored and published with supervision in high-level, peer-reviewed scientific medical journals and for presentations at meetings. The period of research is not designed for mere surgical technique practice; improvement in surgical technique is gained through steady, intricate, and demanding systematic work in the laboratory. There are opportunities for microsurgical skills practice and the laboratory sponsors many surgical courses during the year. It is expected that the fellow will work with the other fellows in the laboratory on a collaborative basis. Projects in the must be submitted in writing to, discussed with, and approved by Dr. Preul. Work and attendance in the hospital or away from the hospital will be verified by Dr. Preul and other Barrow Neurological Institute administrators.
Funding
There is limited funding. There are two funded research positions per year, and one of these positions is taken by a fellow in the PhD Neuroscience Graduate Program who is in residence for several years. This does not mean two new funded fellowships each year. Rather, it means two people will be on funding that may last several years. Thus, there are years when no new funding is available.
The other fellowship position is awarded competitively and also with regard to timing of the intent to begin work at the laboratory. Not being awarded the fellowship does not preclude coming to the laboratory. Thus, the funding opportunity is very limited and in many cases it will be necessary to self-fund the fellowship period. Once here, there is not availability to apply for funding from the hospital, thus complete funding must be established and attested for the whole period or the position will be terminated. Information concerning funding is available from Dr. Preul.
Medical students or recently graduated medical students will be assistants according to their abilities and experience and need to arrange their own funding. They may not have a permanent place in the laboratory if there are residents or fellows who arrive and who are given priority status.
We encourage potential fellows to apply for financial sponsorships from their home institution or other sources, such as from associations, organizations, corporate, or government entities. Applicant arrangements for self funding must be comparable to the limited funded positions and must be substantiated and processed by Barrow and St. Joseph’s administrators. Other costs such as health insurance, travel, and dependents also must be borne by the applicant. Hospital research administration and human resources visa officials will provide information on the funding you must achieve and processing or sponsorship of visas.
It is strongly suggested that you consider coming self-funded, as this is the way the vast majority of fellows have come to the laboratory. We do not have the funds to support salaries as well as project costs. If the fellow brings their family, the fellow is responsible for their adequate funding, including housing and living costs. Work positions or government subsidies will not be available for their support, and we cannot be responsible for their funding. The cost of living in Phoenix, Arizona is quite high, and verification of the adequate funding is necessary to secure a visa.
The position of neurosurgery research fellow does not lead to a clinical position and is not to be used as a base for seeking a clinical or residency position with frequent or long absences from the laboratory. All project expenses as mentioned above are covered by the our laboratory.
Research Opportunities and Benefits
The great benefit in this laboratory is the ability to be quickly involved in projects and to be a part of rapid publications and presentations. This is because we are able to fund project costs so that there is no need to apply for funds to produce projects in most cases, although large, intricate projects may require arrangement for funding (which can take time). Costs for neurosurgical anatomical and other neurosurgical research work are very expensive because of the cadaveric material used, our staff support, instruments, and other equipment available such as operating microscopes, endoscopy instrumentation, imaging, etc. Therefore, it is impossible for us to fund fellows with a stipend or salary in addition to funding projects. Our fellows have produced exquisite, state-of-the-art research projects, which is the main goal, and become leaders in neurosurgery around the world.
A certificate from the Institute is awarded at the end of the fellowship from that recognizes the fellowship period, however, the research fellowship does not confer any advanced clinical training status or graduate or clinical degree. For review of what the lab has produced, please examine our scholarly commons database, although this is not necessarily a complete list.
How to Apply
One funded position will be available within 2023 or late 2023 (although the timing is not guaranteed), and these are awarded on a competitive basis as described above. We already have several applicants for the position that may become available in 2023. Our team does not direct or process inquiries for clinical positions.
Required documents for application are:
- Curriculum vitae
- Background statement of experience in research and general description of intent and proposed work at the laboratory
- Three letters of recommendation from faculty, including your department chair
- Proposed timeframe and arrival date
Further vetting of each applicant will be conducted after the above materials are received. All candidates will be interviewed by Dr. Preul before an offer is extended.
Thank you for your inquiry into our neurosurgery research fellowship. Our work in the neurosurgery research laboratory requires a maturity and surgical experience to accomplish, especially our surgical neuroanatomy work and technology development projects. Our laboratory is a place where you can develop knowledge and produce work that will make you a better neurosurgeon. It is not a place for doing clinical review projects, or case studies.
Contact Information
Mark C. Preul, MD
Newsome Chair of Neurosurgery Research
Director, The Loyal and Edith Davis Neurosurgical Research Laboratory
Professor of Neurosurgery
Barrow Neurological Institute
Phoenix, Arizona 85013
(602) 406-3268 – Office
Mark.Preul@DignityHealth.org
- Mark C. Preul, MD – Director
- William Bichard – Clinical Coordinator
- Steve Marsh – Senior Research Assistant
- Tim Martin, DVM, MBA
- Research Fellows, Graduate Students, Medical Students
Located near the I-10 and I-17 Freeways, Barrow Neurological Institute at St. Joseph’s Hospital and Medical Center is about a 20-minute cab ride from Sky Harbor International Airport in Phoenix and a 30-minute drive from Scottsdale Airport.
Note: The external website links are provided for your convenience only. Barrow Neurological Institute does not necessarily endorse the views expressed or the facts presented on the site, nor is responsible for the content on the site in any way.