Introduction
This guidebook will help you understand your diagnosis and treatment plan for your stroke recovery. The information presented here may answer many of your questions, but please speak to any of our staff if you have further questions or concerns. We are here for you.
We recommend that you print this guidebook and keep it in your room so that your health care team may add materials that are specific to your care. This guidebook is intended to be an introductory resource and to serve as a part of your comprehensive rehabilitation program.
Patient: You are the most important member of the recovery team and will be included in the decision making when appropriate. If you are unable to assist with decision making, then an alternate decision maker will be identified, based on hospital policy, until you are able to make decisions for yourself.
Family/Caregiver: With the patient’s consent, you will be included in the decision making processes to help with discharge planning. You will be included in family teaching/education, and you should be an advocate for the patient’s current and future care.
Some of the team members that you may meet during your stay:
Care Management/Case Management*: The nurse case manager is a registered nurse who works together with social work to help with post hospital care planning in cooperation with insurance coverage and community options for patients and families.
Chaplain Services: The chaplains provide emotional and spiritual support during your recovery at your request.
Neuropsychology: Neuropsychologists specialize in how changes in the brain affect thinking skills, mood, and behavior. They can provide neuropsychological testing to assess memory, attention, language abilities, visuospatial functions, and problem-solving skills. Neuropsychologists can provide education to you and your family regarding cognitive and behavioral effects of stroke. They may also help provide emotional support and education to patients who are adapting/adjusting to life after stroke.
Nursing: Nurses have special education and training to care for patients with stroke. They are responsible for planning your care, helping you understand your medications, watching for side effects of medicines, treating your pain and keeping you as comfortable as possible. Nurses make decisions about your care, watch your vital signs (heart rate, blood pressure, and breathing) and supervise care given to you by other staff such as nurse’s aides. The nurses work closely with the doctors and therapists to teach you about your illness, medication and therapies so you can take an active part in your recovery.
Nurse Practitioners (NPs) are registered nurses with graduate education and advanced clinical training. Our NPs work collaboratively with the physicians and other members of the health care team to assist in providing high quality, individualized care.
Occupational Therapy (OT)*: Occupational therapy works on returning you to daily life through occupation (an occupation is anything that people do during the course of everyday life). This will include the physical and cognitive skills to engage in activities in your environment and resume your life roles which include self care, productivity and leisure. They will also address, as needed, your neuromuscular recovery, vision, visual perceptual issues, positioning, splinting, sensation, tone management, adaptive equipment use, range of motion (ROM) and strengthening in attempt to return you to your everyday life.
Physical Therapy (PT)*: Physical therapy focuses on functional mobility training, gait/assistive device training, seating/positioning, tone management, therapeutic exercise to enhance strength and ROM, pain management, balance and neuromuscular re-education to assist with restoration of function and prevent disability.
Physicians (MD or DO): The physicians who will work together in managing your care may include specialists in multiple areas including, neurology, neurosurgery, internal medicine, physiatry* and other specialties depending on your specific needs.
Registered Dieticians: These professionals ensure that you receive nutrition to promote healing and help with any issues that stem from lack of appetite or difficulty eating.
Rehabilitation Psychology: Rehabilitation psychologists will assist you and your family with adjustments to medical conditions and provide education related to emotional, physical, cognitive and behavioral correlates of injury/illness.
Rehabilitation Technicians/Aides: They work alongside the nurses to assist you with basic care that you may be unable to do for yourself. This may include helping you get in and out of bed, going to the bathroom and assisting with your personal daily needs.
Respiratory Therapy (RT): Respiratory therapy includes the assessment and treatment of breathing disorders and lung conditions. Respiratory therapists are experts in airway management, including tracheostomy/stoma care for you, if you’re having difficulties managing your airway.
Social Worker (SW)*: The social worker is a valuable resource for you and your family. With a vast knowledge of benefits and services offered, the social worker’s primary focus is helping you smoothly transition out of the hospital to the next level of care and helps you address social problems.
Speech Language Pathology (SLP or ST)*: Speech Language Pathologists or Speech Therapists assess and treat swallowing, cognitive issues and communication skills, including understanding (receptive) and using (expressive) language skills, swallow assessment and intervention, clarity of speech, and alternate communication methods.
Therapeutic Recreation (TR): Therapeutic Recreation includes educating you and your family on the importance of continuing leisure interests after discharge. TR will incorporate community reintegration therapy, adaptive sports/recreation, leisure skill building and education, aquatic therapy, community resources, assistance with peer mentors and practice of the skills you learn from other therapists in the clinic to translate those to real life settings.
* Team members required to meet criteria of IRF (Inpatient Rehabilitation Facility) admission.
A stroke is an emergency, just like a heart attack, and medical help is needed right away. The brain controls important functions like movement, breathing and sensory perceptions (for example, sight, touch and taste). It also controls higher functions like thinking, learning, and emotions. The brain needs an adequate supply of oxygenated blood in order to operate.
Strokes usually give warnings.
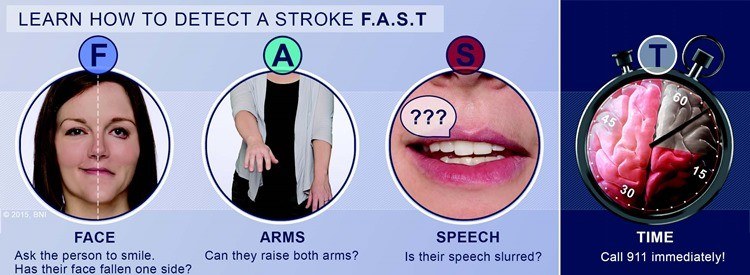
Warning Signs of a Stroke
- sudden numbness and tingling or weakness of the face, arm, or leg, usually on one side of the body
- sudden loss of speech, trouble speaking, or understanding
- sudden vision problems
- sudden unexplained dizziness, unsteadiness or sudden falls, especially with any of the other symptoms
- sudden severe headache with no apparent cause, described as the “worst headache” of your life
If you notice one or more of these signs, call 911 and say you are having a stroke. Seek appropriate medical attention immediately at a qualified hospital with a stroke center.
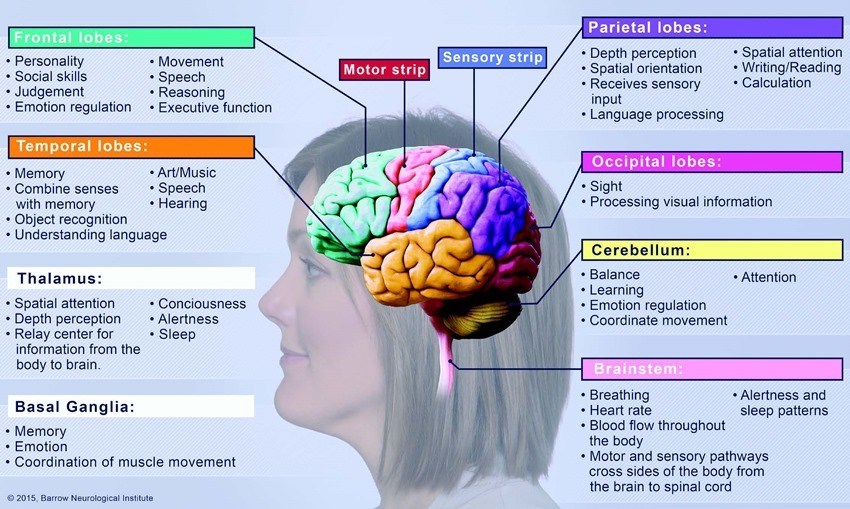
The brain controls important functions like movement, breathing, and sensory perception. It also controls higher functions like thinking, learning, and emotions. These functions may be associated with specific parts of the brain. A stroke causing damage in one of these parts of the brain may affect function associated with the damaged area.
Ventricles: A set of four (4) cavities in the brain where cerebrospinal fluid (CSF) is produced, responsible for the production and flow of the CSF from the brain to the spinal cord. If this stops working it can cause fluid buildup, pressure and trapping of CSF and blood which needs to be drained by a device such as an external ventricular drain (EVD) or shunt.