Herniated Disc
Herniated Disc Overview
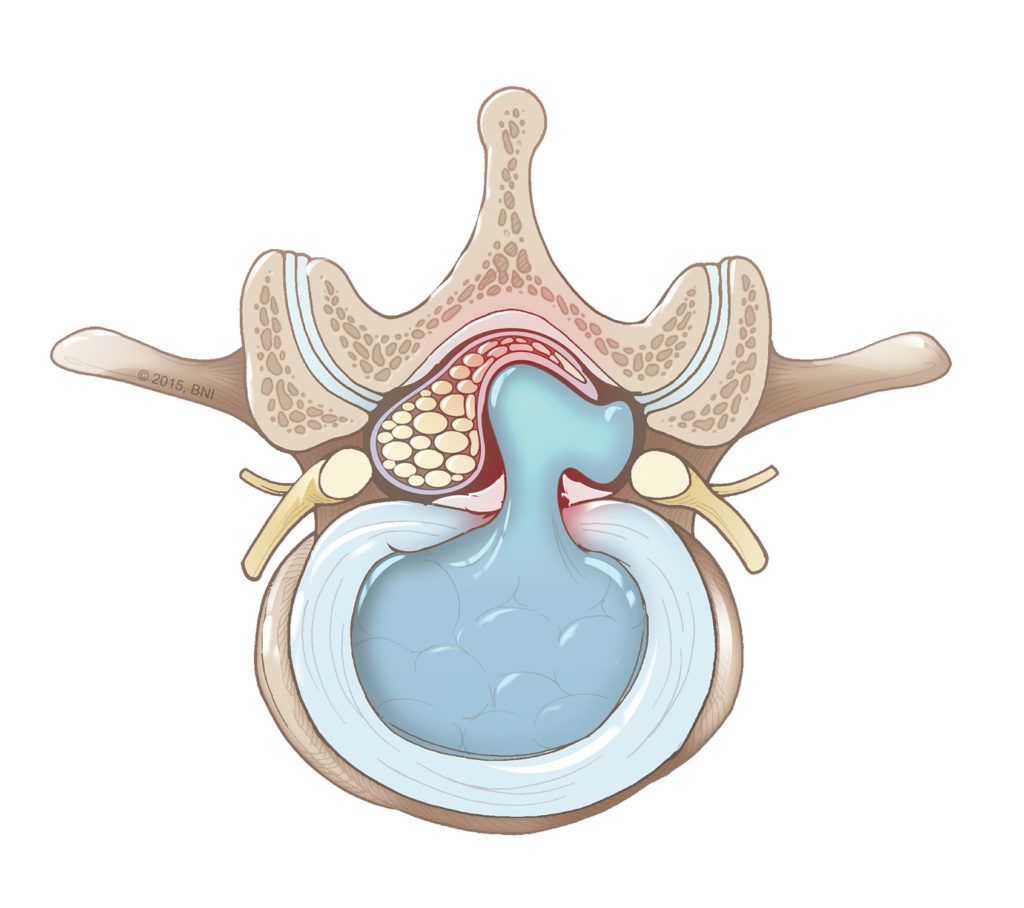
A herniated disc occurs when the soft center (the nucleus pulposus) of an intervertebral disc pushes through a tear in the tough outer layer (the annulus fibrosus) of the disc and into the spinal canal. The protruding disc fragment can put pressure on the spinal cord, causing back pain and spinal cord dysfunction.
Intervertebral discs act as shock absorbers for the spine and enable it to move. These discs can tear due to degeneration, injury, or a combination of both.
Herniated discs can occur in any part of the spine but are most common in the lower back (lumbar spine) followed by the neck (cervical spine). Herniated discs are least common in the mid back (thoracic spine).

Disc Herniation Symptoms
Symptoms of a herniated disc vary depending on the location and severity of the disc herniation.
Symptoms of a herniated disc in the lumbar spine may include:
- Bowel and bladder dysfunction
- Lower back pain
- Sciatic nerve pain, an electric shock-like pain which radiates from the buttocks down into one leg
- Weakness in the leg and/or foot
Symptoms of a herniated disc in the cervical spine may include:
- Dull or sharp pain in the neck or between the shoulder blades
- Neck pain that increases with movement
- Neck pain that radiates down the arm to the hand
- Numbness or tingling in a shoulder or arm
Symptoms of a herniated disc in the thoracic spine may include:
- Bowel and bladder dysfunction
- Difficulty walking
- Pain in the mid back, which may wrap around the chest
- Progressive weakness and numbness in the lower extremities

Disc Herniation Treatments
Conservative Treatment for Herniated Disc
Most herniated discs don’t require surgery. Your doctor may initially prescribe a conservative treatment plan consisting of rest or a reduced activity level, anti-inflammatory medication, and/or physical therapy.
If the pain affects your quality of life and is not relieved with conservative treatments, you may be a candidate for surgery. Surgery also may be recommended if you develop progressive neurological deficits, such as leg weakness or numbness, loss of normal bowel or bladder functions, or difficulty walking.
Surgical Treatment for Herniated Disc
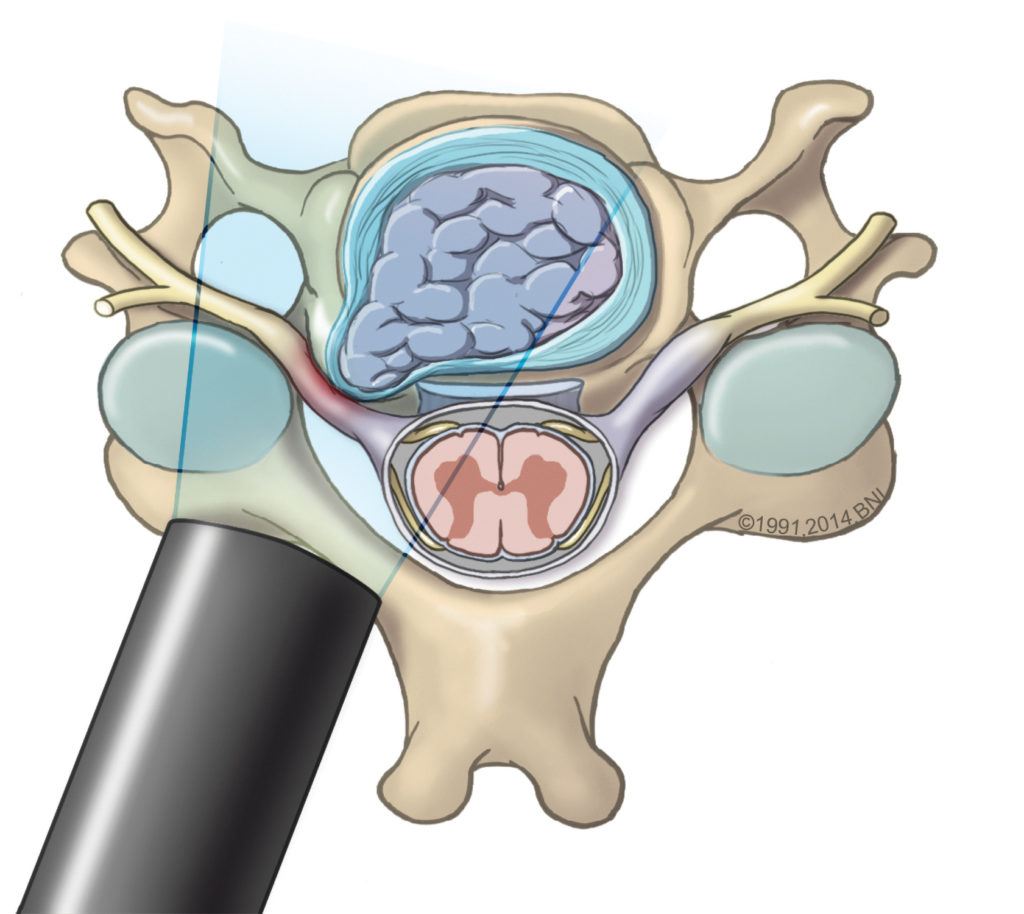
Discectomy – In this procedure, the neurosurgeon removes the protruding fragment of the disc that is compressing the spinal cord or spinal nerves and causing symptoms. Our spinal surgeons are leaders in minimally invasive techniques for disc herniation, in which they use specialized instruments to operate through smaller incisions. The benefits include:
- A shorter hospital stay
- Less post-operative pain
- Less time in surgery
- Reduced blood loss
- Faster recovery
Additional Information
How common are herniated discs?
Disc herniation is a common spinal condition. It has been estimated that 5 to 20 cases per every 1,000 adults occur annually.
Who gets herniated discs?
Because disc herniation can be caused by an injury, it can affect anyone. However, it is most common in people between the ages of 30 and 50, and it occurs more often in men than in women. As people age, their intervertebral discs may lose their cushioning ability and become more vulnerable to rupture. Research has shown that herniated discs run in families, suggesting a genetic predisposition.
How are herniated discs diagnosed?
Your doctor may use the following to diagnose a herniated disc:
- Imaging tests, such as X-ray, magnetic resonance imaging (MRI), or computed tomography (CT)
- Medical history
- Physical examination