
Head and Neck Cancer Surgery
Overview of Surgery for Head and Neck Cancer
Head and neck cancer surgery is a specialized area of medicine performed by doctors who specialize in surgery for tumors of the head and neck. Often these are sub-specialists within the field of otolaryngology or ear, nose and throat surgeons (also called ENT surgeons). These surgeons focus on the surgical treatment of cancerous tumors and conditions within the head and neck region. This can include cancers of the mouth, throat, larynx (voice box), nose, sinuses, and salivary glands. The goal of this type of surgery is not only to remove the cancer but also reconstruction to preserve your ability to speak, eat, and breathe as normal as possible and maintain your quality of life.
Reducing the chance that the cancer will come back is also an objective. Depending on the cancer’s size and location, doctors aim to keep the nearby organs and nerves working well.
There are different surgical techniques used, depending on where the cancer is and how advanced it is. These can range from more minor surgeries to remove a small tumor to more extensive surgeries that may involve removing more significant areas of tissue. Surgery for head and neck cancer sometimes requires removing substantial amounts of tissue. In that case, you might need reconstructive surgery to help restore appearance and function. This can involve using tissue from other parts of your body to help rebuild the affected area.
Whenever possible, ENT surgeons use minimally invasive techniques, such as transoral laser microsurgery or transoral robotic surgery. These methods can lead to quicker recovery times and less impact on your body.
Treatment often involves a team of specialists, including otolaryngologists/ENT surgeons, medical and radiation oncologists, radiologists, speech therapists, and nutritionists, to provide comprehensive care. This team approach helps manage the surgical aspects and the recovery and rehabilitation process.
After surgery, you’ll have follow-up appointments to monitor your recovery and manage any side effects. Rehabilitation, including speech and swallowing therapy, may be necessary to help you regain function affected by the surgery.
It’s important to discuss all available treatment options with your doctor, including the benefits and risks of surgery, to make an informed decision about your care. At Barrow Neurological Institute, your team of head and neck cancer specialists is there to support you through each step of the process, from diagnosis and treatment to recovery and beyond.
What do Head and Neck surgeons treat?
Head and neck surgeons treat a variety of tumors located in the head and neck region, including the following kinds of head and neck cancer:
- Oral Cavity Cancer: Cancer that affects the lips, the front two-thirds of the tongue, the gums, the lining inside the cheeks and lips, the bottom (floor) of the mouth under the tongue, the hard palate (the front part of the roof of the mouth), and the small area of the gum behind the wisdom teeth.
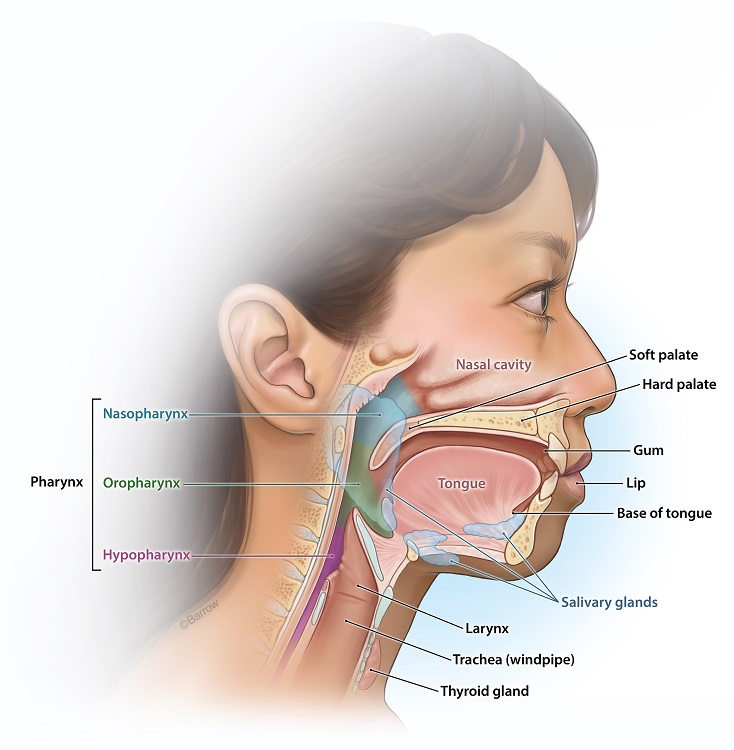
- Oropharyngeal (Throat) Cancer: Cancer of the nasopharynx, or the upper part of the throat behind the nose; the oropharynx, or the middle part, including the soft palate (the back part of the roof of the mouth), the base of the tongue, and the tonsils; and they hypopharynx, or the lower part of the pharynx.
- Laryngeal Cancer: Cancer that involves the vocal cords and the epiglottis (a flap of tissue that prevents food from entering the airway).
- Nasal Cavity and Paranasal Sinus Cancers: Cancer that affects the nasal cavity, or the space just behind the nose, and the sinuses, which are small, air-filled cavities inside the bones of the nose.
- Salivary Gland Cancer: There are several salivary glands in the mouth and throat areas, including the parotid, sublingual, and submandibular glands, which produce saliva. Cancer can affect all of these glands.
- Thyroid Cancer: There are a several types of thyroid cancer and generally surgery is an important part of the surgical treatment of thyroid cancer.

Head and neck surgeons also treat benign, noncancerous tumors and diseases of the head and neck. These include:
- Benign salivary gland tumors
- Salivary stones
- Benign thyroid nodules/goiters
- Congenital neck anomalies like branchial cleft cysts and thyroglossal duct cysts
- Benign but locally destructive lesions of the bones of the skull, jaw, and other bony structures in the head and neck
The main objective of head and neck cancer surgery is to remove the cancerous tumor and some of the healthy tissue around it to ensure the removal of all cancerous tissue. The surgery may also be used to remove lymph nodes in the neck if there is a risk that the cancer has spread. Depending on the location and stage of the tumor, surgery can vary from minimally invasive procedures to more extensive operations that may require reconstruction of the affected area. Surgery aims to eliminate the cancer while striving to preserve your appearance and the function of critical structures like your tongue, voice box, and swallowing mechanisms as much as possible.
Am I a good candidate for head and neck cancer surgery?
Determining whether you are a good candidate for head and neck cancer surgery involves careful evaluation of various factors related to your overall health, the type and stage of your cancer, and the specific characteristics of the tumor. Therefore, consulting with your healthcare provider for personalized advice is crucial. With that said, there are some factors you will want to discuss with your head and neck surgeon as you contemplate surgery:
- Cancer Type and Stage: Your otolaryngologist will more likely recommend surgery for specific types and stages of head and neck cancer. Early-stage cancers are often treated successfully with surgery, possibly followed by radiation or chemotherapy. For more advanced cancers, surgery might be combined with other treatments.
- Tumor Location and Size: The tumor’s location and size can affect whether surgery is feasible and what type might be most effective. Tumors in areas that can be operated on without causing significant functional or cosmetic issues are more likely to be treated surgically.
- Your Overall Health: Good candidates for surgery are typically those who are in otherwise good health and are capable of withstanding the stresses of surgery and recovery. Factors like heart health, lung function, and the ability to recover from anesthesia are essential considerations.
- Potential Impact on Function and Quality of Life: Surgeons will consider the impact of surgery on functions such as speech, swallowing, and breathing, as well as the potential need for reconstructive surgery to restore appearance and function.
- Your Preferences and Goals: Your preferences, lifestyle, and goals are crucial in deciding the treatment plan. Some people may prioritize preserving function or appearance, while others may prioritize the most aggressive cancer treatment available.
- Other Medical Conditions: Existing medical conditions that could complicate surgery or recovery need to be considered. These might include diabetes, immune system disorders, or a history of smoking, which can affect healing.
- Availability of Other Treatments: In some cases, non-surgical treatments like radiation therapy, chemotherapy, or targeted therapy may be preferred based on the cancer’s characteristics or your health.
It’s essential to have a thorough discussion with your medical or radiation oncologist, a head and neck surgeon, and possibly other multidisciplinary cancer care team members. They can provide detailed information based on diagnostic tests (like imaging and biopsy results), your health history, and treatment preferences to help you make an informed decision.
What are the steps of head and neck cancer surgery?
The specific steps of head and neck cancer surgery can vary widely depending on the type, location, and stage of the cancer, as well as the surgical technique. However, most surgical procedures for head and neck cancer follow a general sequence of steps, from preparation through to recovery. Here is what you can expect:
Preoperative Assessment and Planning
Your care team will perform a medical evaluation to ensure you’re fit for surgery, including assessments of your overall health, the function of vital organs, and any existing medical conditions.
Imaging studies like MRI, CT scans, or PET scans may be done to determine the location and extent of the tumor and to aid in planning your surgery.
In addition, your doctor might perform a biopsy to confirm the type and grade of cancer.
At Barrow, every new cancer patient is presented at our multidisciplinary head and neck tumor board. You case will be reviewed by our team of surgeons, medical and radiation oncologists, radiologists, and pathologists to discuss the best treatment approach.
Finally, your surgeon will review the surgery’s risks, benefits, and alternatives with you and ask you to consent to the operation.
Preparation for Surgery
You’ll be asked not to eat or drink for a certain period before the surgery.
Before surgery begins, an anesthesiologist will give you medicine to ensure you’re asleep and pain-free during the procedure.

The Surgery
Your surgeon will start by making an incision in the skin to access the tumor. The location and size of the incision depend on the tumor’s location. Some operations may be done through the mouth or endoscopically and may not involve an external skin incision.
Next, your surgeon will remove the tumor along with a margin of healthy tissue around it to ensure the removal of all cancer cells. The extent of tissue removal varies by the tumor’s size and spread.
If there’s a concern about cancer spreading, lymph nodes in the neck may also be removed (neck dissection).
For surgeries that result in significant tissue loss, reconstructive surgery may be performed immediately after tumor removal to restore form and function. This might involve using skin, muscle, or bone grafts from other parts of the body.
Finally, your surgeon will close the incisions with sutures or staples and apply dressings.
Postoperative Care
Immediately after surgery, your postoperative team will monitor you to manage your pain, prevent infection, and ensure stable vital signs.
You may need to stay in the hospital for a length of time, which will vary depending on the extent of your surgery and your overall health. Depending on the surgery’s impact, you may need speech therapy, physical therapy, or other rehabilitation services to help restore function.
Follow-Up and Adjuvant Treatment
Your care team will schedule several appointments to monitor your healing and manage complications.
Radiation, chemotherapy, or other treatments may be recommended depending on the cancer stage and pathology results.
Long-Term Recovery and Monitoring
Ongoing monitoring for any signs of cancer recurrence and management of any long-term effects from the surgery will be an essential part of your long-term postoperative care.
Every person’s experience with head and neck cancer is unique, and the specifics of your surgery will depend on your situation. It’s essential to have open and detailed conversations with your surgical team to understand the steps and implications of your particular procedure.
Common Surgical Procedures and Techniques for Head and Neck Cancer
Transoral Robotic Surgery
Transoral robotic surgery, or TORS, is a modern way doctors can remove cancers in the throat and other parts of the head and neck without making large incisions on the outside of your body. Instead, the surgery is done through your mouth.
In this procedure, your surgeon uses a sophisticated robot with a camera and very small, precise instruments. This system gives your surgeon a detailed, 3D view of the area being operated on and allows for exact movements within tight spaces.
The entire procedure is done through the mouth, meaning no external scars exist. This approach can reduce the surgery’s impact on appearance and lead to a quicker recovery than traditional surgery.
TORS allows for the precise removal of tumors with potentially fewer side effects. Patients often experience less pain, a shorter hospital stay, and a quicker return to normal activities and functions like eating and speaking.
Recovery from TORS is generally faster than traditional head and neck surgery. Your healthcare team will closely monitor you, and you may need rehabilitation services, such as speech therapy, to help you recover fully.
TORS is not suitable for all types of head and neck cancer. It’s typically used for cancers that are hard to reach with conventional surgery and for people where the cancer has been detected at an early or intermediate stage. It is also important to note that TORS may be combined with a traditional operation to address lymph nodes within the neck
It’s important to discuss with your doctor whether TORS is a suitable option for you based on the specific details of your cancer, your overall health, and your treatment goals. Your doctor can provide more information about the procedure, its benefits, and what you can expect during recovery.

Transoral Laser Microsurgery
Transoral laser microsurgery, or TLM, is a procedure doctors use to treat some throat cancers and other cancers of the head and neck. It involves using a special kind of intense light, called a laser, to remove unhealthy tissue.
Since the surgery is done through the mouth, there are no incisions made on the outside of your neck or face. This means less pain and scarring for you compared to traditional surgery. The laser allows your surgeon to accurately target and remove the cancerous tissue, which helps preserve as much of the healthy surrounding tissue as possible. This focus on precision can lead to better outcomes in terms of your ability to speak and swallow after surgery.
During TLM, you’ll be under general anesthesia, which means you’ll be asleep and won’t feel anything. The surgeon uses a microscope to get a detailed view of the area and then directs the laser to remove the tumor.
Generally, recovery from TLM is quicker than traditional open surgery. You may have a shorter hospital stay and get back to your normal activities and diet sooner.
TLM is particularly useful for early-stage cancers but might also be an option for more advanced cases, depending on several factors. Your healthcare team will consider the specific characteristics of your cancer, your overall health, and other treatments you might need.
It’s important to discuss all available treatment options with your doctor, including TLM, to understand the best approach for your specific situation.
Both TORS and TLM allow your surgeon to treat a primary tumor through the mouth and avoid the morbidity, scarring, and other complications from open approaches to the mouth and throat. However, lymph node and neck metastases still need to be addressed with a conventional open operation. Fortunately, this is much more straightforward and far less disfiguring and easier to recover from than a traditional open operation for the throat and voice box.
Reconstructive Surgery for Head and Neck Cancer
After removing the cancer from your head or neck, doctors may need to do another surgery to help repair the area. This is called reconstructive surgery, and its goal is to help you look and feel as close to normal as possible and help you eat, speak, and breathe better.
The surgery aims to rebuild the parts of your head and neck that were affected by cancer or its treatment. For example, if the surgery was on your mouth or throat, the goal is to help you swallow and speak. If it affected your appearance, doctors would try to restore it as much as possible.
The type of reconstruction depends on what area was affected and how much tissue was removed. Sometimes, surgeons can use tissue like skin, muscle, or bone from other parts of your body to rebuild the area (this is called flap surgery). In other cases, they might use prosthetics or artificial materials.
Reconstruction is often done right after the cancer is removed in the same surgery. Occasionally it might be done later, after you’ve healed or finished other treatments like radiation or chemotherapy.
The recovery process varies depending on the type of reconstruction done. It might include staying in the hospital, taking it easy for a while, and going to rehabilitation therapies, like speech therapy, if your mouth or throat is involved.
A team of specialists, including surgeons, oncologists, speech therapists, and nutritionists, will be involved in your care. This team works together to plan the best approach for your reconstruction, considering your specific needs and the specifics of your cancer treatment.
You should have open discussions with your healthcare team about your concerns and expectations and any questions about the reconstruction process. They can provide detailed information and support to help you through your recovery.
Reconstructive surgery is a complex but essential part of treatment for many people with head and neck cancer. It is crucial in improving your quality of life after cancer treatment.
References
- Yang JC, Yang AI, Gross RE. Sensing-Enabled Deep Brain Stimulation in Epilepsy. Neurosurg Clin N Am. 2024 Jan;35(1):119-123. doi: 10.1016/j.nec.2023.08.005. Epub 2023 Sep 21. PMID: 38000835.
- Hageboutros K, Hewitt KC, Lee GP, Bansal A, Block C, Pedersen NP, Willie JT, Loring DW, Schoenberg MR, Smith KA, Giller CA, Gross RE, Drane DL. Comparison of minimally invasive to standard temporal lobectomy approaches to epilepsy surgery: Seizure relief and visual confrontation naming outcomes. Epilepsy Behav. 2024 Jun;155:109669. doi: 10.1016/j.yebeh.2024.109669. Epub 2024 Apr 24. PMID: 38663142.
- Yang AI, Isbaine F, Alwaki A, Gross RE. Multitarget deep brain stimulation for epilepsy. J Neurosurg. 2023 Jul 14;140(1):210-217. doi: 10.3171/2023.5.JNS23982. PMID: 37486888.
- Whiting AC, Chen T, Swanson KI, Walker CT, Godzik J, Catapano JS, Smith KA. Seizure and neuropsychological outcomes in a large series of selective amygdalohippocampectomies with a minimally invasive subtemporal approach. J Neurosurg. 2020 Jun 12;134(6):1685-1693. doi: 10.3171/2020.3.JNS192589. PMID: 32534491.



