Microvascular Decompression
Overview of Microvascular Decompression
Microvascular decompression is a neurosurgical procedure for the treatment of pain or muscle twitching caused by blood vessel in the head or neck putting pressure on a nearby nerve.
There are several syndromes or neuralgias that are caused in this manner, and they include:
- Trigeminal Neuralgia is a sharp or stabbing pain, sometimes described as being like an electric shock, affecting either the left or right side of the face. It is most commonly caused by a blood vessel putting pressure on the trigeminal nerve.
- Hemifacial Spasm is a twitching or muscle spasm that affects either the right or left half of the face, usually caused by a blood vessel putting pressure on the facial nerve.
- Glossopharyngeal Neuralgia is frequently described as sharp, stabbing, or pulsing pain affecting the inner ear, throat, and back of the mouth. It is frequently caused by a blood vessel putting pressure on the glossopharyngeal nerve.
Trigeminal neuralgia is the most common of the three conditions listed above and also the most common reason for performing microvascular decompression.
Anatomy of the Cranial Nerves and Cerebrovascular System
From the neck down, the nerves that control your body are connected to your brain via your spinal cord. However, the nerves that control movement and sensation in your head and face bypass the spinal cord and are connected directly to your brain.
These are called the cranial nerves, and there are 12 pairs of them. In some parts of your head the arteries and veins responsible for circulating blood are located very close to a cranial nerve. When these vessels directly contact and pound against a cranial nerve, the problems listed above can occur.
The symptoms caused by trigeminal neuralgia, hemifacial spasm, and glossopharyngeal neuralgia correlate directly to the nerve that is affected.
- The trigeminal nerve is the largest and most complex of the cranial nerves. Among its many functions is to transmit sensation—especially temperature and pain–from the face to the brain, and this is why damage or irritation to the nerve can cause intense pain.
- The facial nerve, among other roles, is responsible for moving the muscles of the face. This is why hemifacial spasm can result from irritation or damage to that nerve.
- The glossopharyngeal nerve is responsible for motor, autonomic, and sensory function in the throat and back of the mouth, and glossopharyngeal neuralgia therefore describes pain or dysfunction caused in the areas innervated by that nerve

What is Microvascular Decompression Used For?
Microvascular decompression is used to alleviate pain or other symptoms caused by a blood vessel putting pressure on a cranial nerve. This is accomplished through a neurosurgical procedure that relocates the blood vessel or places a barrier between the blood vessel and the affected nerve.
Steps of Microvascular Decompression
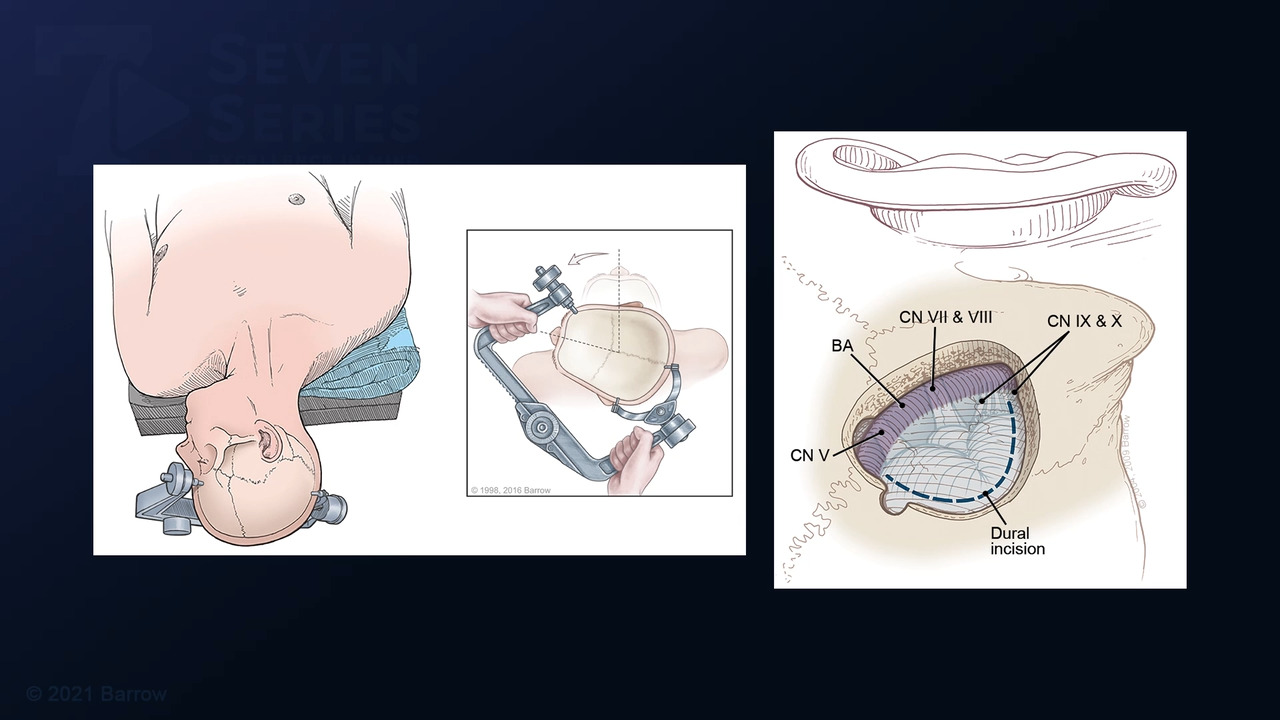
1) Opening of the Skin, Skull, and Dura
Microvascular compression is always performed under general anesthesia. The neurosurgeon begins by making an incision in the skin to expose the skull. A small piece of the skull is then removed to expose the dura, which is the tough outer covering of the brain. An incision is made in the dura to expose the brain.
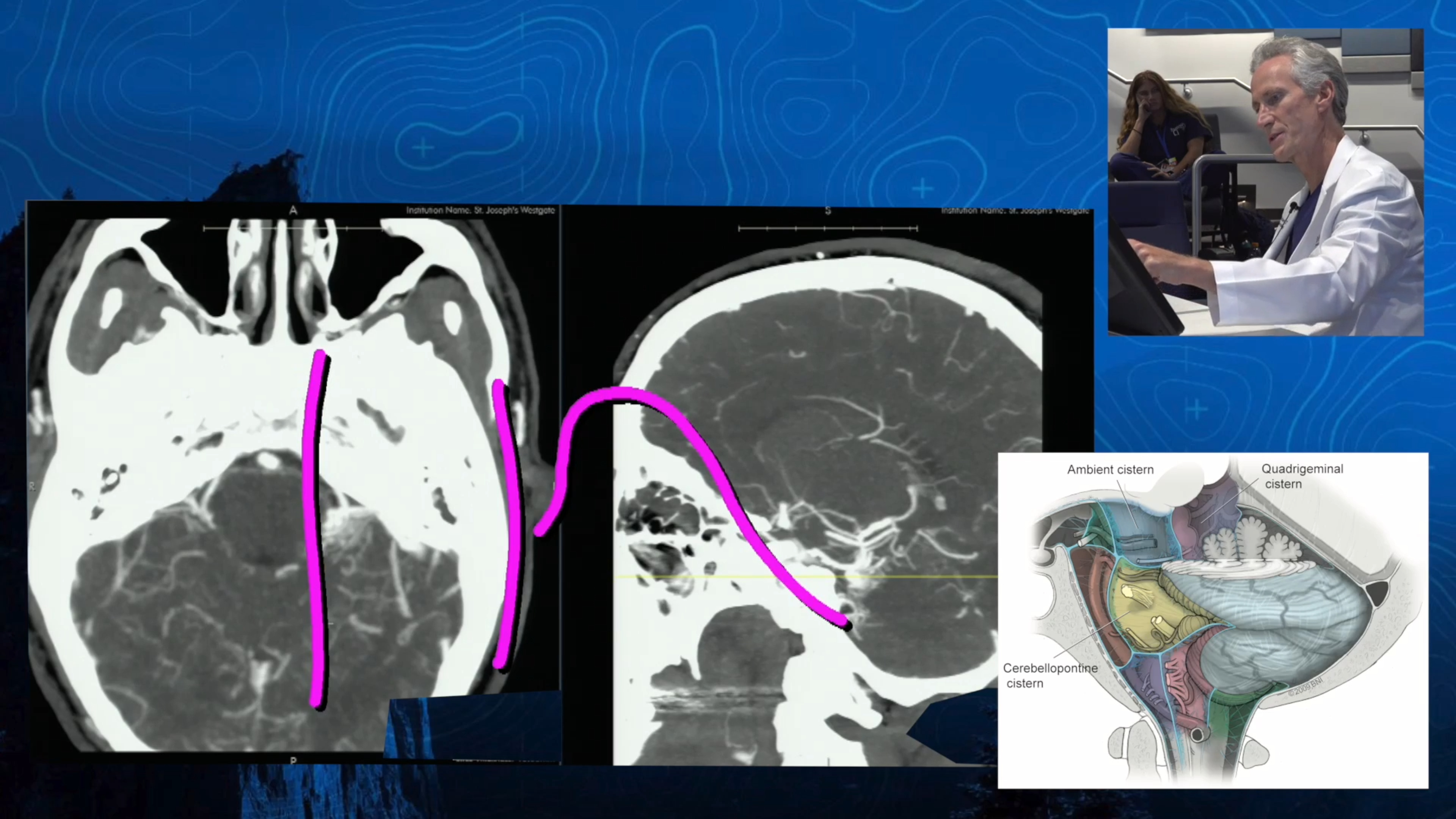
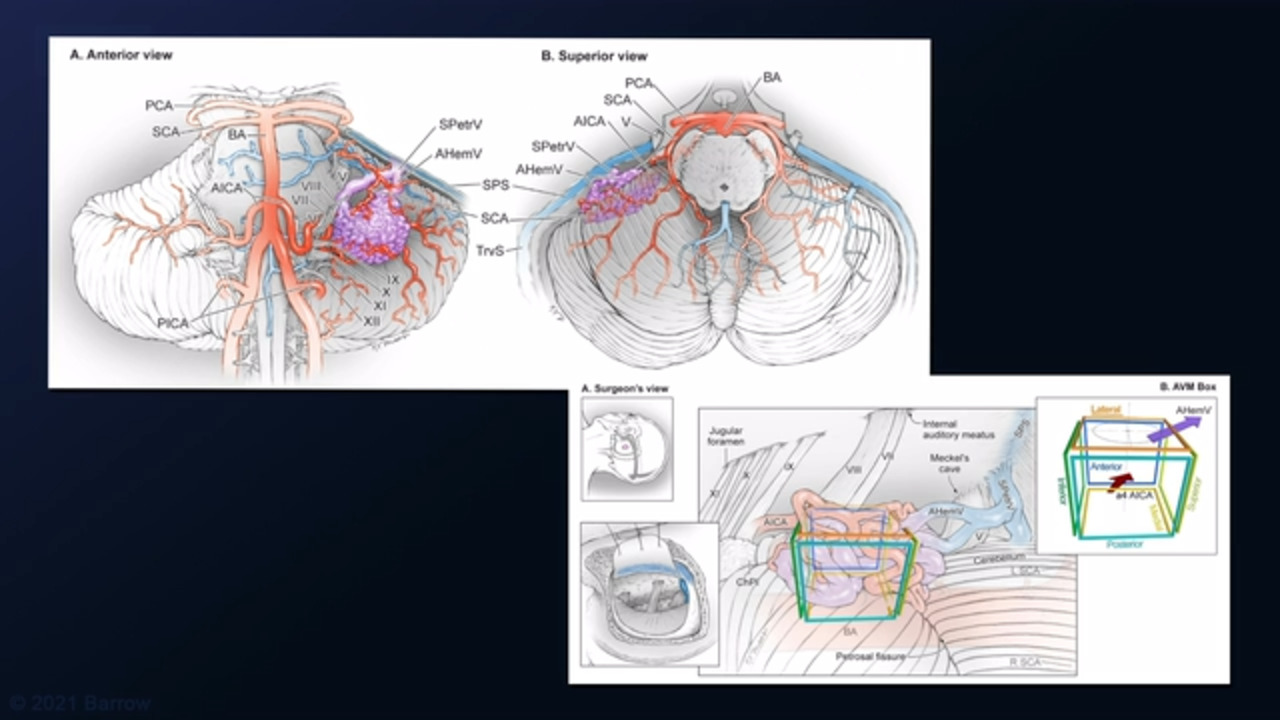
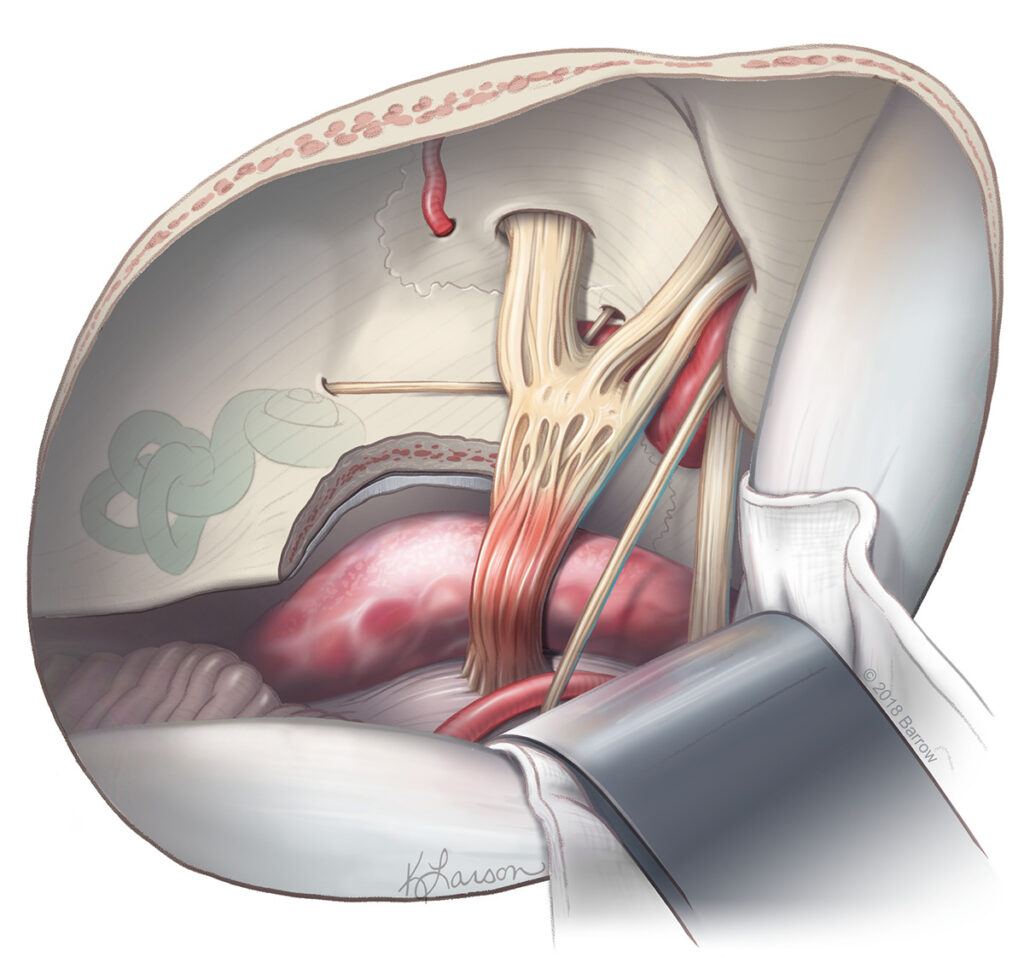
2) Exposure of the Cranial Nerve and Blood Vessel
The neurosurgeon uses natural corridors to gently navigate through the spaces around the brain without entering or harming brain tissue. Once the neurosurgeon can see the affected nerve and blood vessel, the artery is freed from the nerve.
3) Decompression of the Cranial Nerve
Depending on the location of the blood vessel in proximity to the affected cranial nerve, the neurosurgeon may use one or a combination of several techniques to achieve microvascular decompression of the nerve. These can include:
- Placing a small sponge between the nerve and the blood vessel to cushion the nerve from the blood vessel (microvascular decompression)
- Using a sling to pull the blood vessel away from the nerve (macrovascular decompression)
- Rerouting the blood vessel using a procedure called cerebrovascular bypass (macrovascular bypass)
Macrovascular Decompression versus Microvascular Decompression
In some cases, the symptoms of trigeminal neuralgia, hemifacial spasm, and glossopharyngeal neuralgia are caused by a diseased, abnormal, or enlarged artery. In these instances, neurosurgeons use a modified version of microvascular decompression known as macrovascular decompression.
Macrovascular decompression can describe the use of a sling to separate the artery from the affected cranial nerve and keep it positioned far away, or the process of disconnecting and rerouting the artery using vascular bypass. Macrovascular decompression is used for large and diseased arteries because a sponge does not provide enough cushion to alleviate symptoms in these cases.
4) Closure
The neurosurgeon closes the dura, replaces the removed portion of the skull, and closes the incision in the scalp to complete the operation.
Many people experience near immediate symptom relief when they wake up from this procedure.
The steps for macrovascular decompression are largely the same
Am I a good candidate for microvascular decompression?
You might be a good candidate for microvascular decompression if you have trigeminal neuralgia, hemifacial spasm, or glossopharyngeal neuralgia and the following are also true:
- You have tried conservative treatments like medication and nerve blocks with little or no success, or if these treatments originally provided temporary relief but no longer do
- You are healthy enough to undergo a surgical procedure under general anesthesia
What are the risks of microvascular decompression surgery?
Any neurosurgical procedure comes with at least a small amount of risk. These can include bleeding, postoperative infection, allergic reactions to anesthesia or medications given before, during, and after surgery, blood clots, and stroke.
Microvascular decompression surgery carries with it a risk of nerve damage. This is because the neurosurgeon is required to work in close proximity to a cranial nerve to relieve the pressure being exerted by the nearby blood vessel.
The likelihood of experiencing these complications is exceedingly rare provided you are under the care of an experienced neurosurgeon, especially if the neurosurgeon specializes in neurovascular and cerebrovascular neurosurgery.
Additional Resources
Neuroanatomy, Cranial Nerve 5 (Trigeminal)
References
- Srinivasan VM, Labib MA, Furey CG, Catapano JS, Lawton MT. The “Binder Ring” Bypass: Transection, Rerouting, and Reanastomosis as an Alternative to Macrovascular Decompression of a Dolichoectatic Vertebral Artery. Oper Neurosurg (Hagerstown). 2022 Apr 1;22(4):224-230. doi: 10.1227/ONS.0000000000000099. PMID: 35147579.
- Tabani H, Yousef S, Burkhardt JK, Gandhi S, Benet A, Lawton MT. Macrovascular Decompression of Facial Nerve With Anteromedial Transposition of a Dolichoectatic Vertebral Artery: 3-Dimensional Operative Video. Oper Neurosurg (Hagerstown). 2019 Jan 1;16(1):E4. doi: 10.1093/ons/opy117. PMID: 29788154.
- Choudhri O, Connolly ID, Lawton MT. Macrovascular Decompression of the Brainstem and Cranial Nerves: Evolution of an Anteromedial Vertebrobasilar Artery Transposition Technique. Neurosurgery. 2017 Aug 1;81(2):367-376. doi: 10.1093/neuros/nyx110. PMID: 28402528.
- Wang DD, Burkhardt JK, Magill ST, Lawton MT. Anterior Transposition of Anomalous Tortuous Vertebral Artery Causing Cervical Radiculopathy: A Report of 2 Cases and Review of Literature. World Neurosurg. 2017 May;101:289-295. doi: 10.1016/j.wneu.2017.01.129. Epub 2017 Feb 9. PMID: 28192269.