XLIF Surgery
Extreme Lateral Interbody Fusion (XLIF) Overview
XLIF, which is short for extreme lateral interbody fusion, is a minimally invasive approach to lumbar spinal fusion surgery, also called lumbar interbody fusion, in which the neurosurgeon accesses the spine from the side of the body.
Spinal fusion is performed to join together two or more bones of the back, called vertebrae, eliminating movement between them. This is done by inserting a bone graft in between the two vertebrae and allowing the body to heal it over several months, much like it would heal a bone fracture. The bone graft is usually held in place with spinal instrumentation like rods, screws, and plates.
Traditionally, surgeons accessed the spine through the front of the body (anterior) or the back (posterior) when performing spinal fusion surgery. With the side (lateral) approach, the surgeon does not have to cut through major muscles in the back or abdomen. It also eliminates the need to move the organs of the abdomen to the side to access the spine, as is required in anterior procedures. This approach has several benefits, including:
- A shorter hospital stay
- Less post-operative pain
- Less time in surgery
- Minimal blood loss
This surgery may also allow you to return to normal activities more quickly.
To access the spine from the side of the body, the neurosurgeon makes a small incision and inserts an instrument called a dilator between the side of the abdomen and the muscles covering the spine. The surgeon then uses retractors to gently widen the opening in the muscle tissue, remove any damaged or defective disc material, and insert the bone graft. Electromyography (EMG) allows the surgeon to monitor the position of the surgical instruments in relation to the nerves.

What is XLIF used for?
Extreme lateral interbody fusion can be used to treat the following spinal conditions:
- Lumbar spinal stenosis
- Degenerative disc disease with instability
- Recurrent herniated disc
- Low-grade spondylolisthesis, a condition in which one vertebra slips over another
- Spinal deformities, such as mild scoliosis
Anatomy of the Lumbar Spine
Your spine is made up of 33 vertebrae divided into five different segments, which are listed below in order from your head to your legs:
- Cervical, or the neck
- Thoracic, the middle of the back
- Lumbar, or lower back
- Sacrum, where the spine connects to the hips
- Coccyx, the tailbone
XLIF spine surgery is used to treat conditions in the lumbar spine, which is made up of the five vertebrae that extend from the bottom of your rib cage to the top of your pelvis.
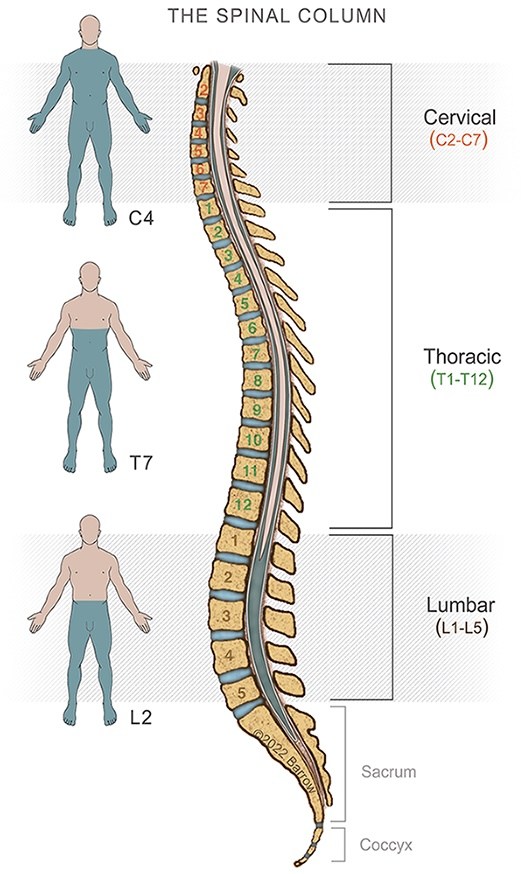
The lumbar spine has a natural lordotic curve, meaning it curves inward toward the front of the body. The lumbar vertebrae are generally larger and sturdier than the thoracic and cervical vertebrae because they provide support for the entire body above the level of the lower back. Similarly, lumbar spinal discs tend to be thicker and tougher than those in higher levels of the spine.
About the Procedure
Extreme lateral interbody fusion is performed under general anesthesia and generally takes 30 minutes to an hour from the time the first incision is made until the operation is completed. Before the surgical procedure begins, a neuro-anesthesiologist administers medications that keep you asleep during surgery. Then, after the operating room staff have positioned you on your side and prepared the surgical site, the following steps occur:
- The neurosurgeon opens a 1.5-inch incision on the side of your body, between your ribs and hip bone.
- Using a gloved finger and navigating by feel, your neurosurgeon develops a natural corridor through the fatty tissue behind your abdominal cavity, navigating around your bowel and kidney.
- When the psoas muscle is reached, intraoperative neurophysiological monitoring (IONM) begins. This technology is used to map the nerves coming out of the spine to ensure they aren’t damaged during the procedure. Intraoperative x-rays are also used to ensure that nerves and vital structures are protected at all times.
- A retractor is placed into the corridor, then an ever larger series of tubes (called tubular retractors) are placed into the corridor to give your neurosurgeon room to work.
- Special tools are used to remove the intervertebral disc.
- An implant and cage are placed between the two vertebra and packed with bone and proteins to promote fusion between the two vertebrae in the former disc space.
- The position of the implant and any screws used to secure the fusion are verified using intraoperative imaging.
- The incision is closed.


Recovery
You will likely be able to go home on the same day as your surgery if you are only having one level fused. For multiple-level fusions, a hospital stay of 1-2 days is usually required.
For the first six weeks after surgery, you will likely experience some mild pain related to manipulation of the psoas muscle, along with some pain in your hip flexor and general lower back soreness.
A complete return to normal activity is usually possible after 12 weeks.
Am I a candidate?
You may be a good candidate for this surgery if you have one of the conditions listed above and have already tried conservative, non-surgical treatments. The location of the vertebrae to be fused will determine which approach is best.
Having one of the previously listed conditions does not necessarily mean you will need XLIF. More conservative treatments such as physical therapy or pain medication may be effective. Extreme lateral interbody fusion changes the normal movement of the spine, which may accelerate wear and tear of the vertebral joints adjacent to the fused vertebrae.
Frequently Asked Questions
What is the success rate?
Most people achieve very good to excellent results after XLIF surgery, with 80-85% of patients reporting a reduction in pain and the ability to return to their normal activities. The fusion rate is nearly 100%, meaning that the adjacent vertebrae successfully and permanently joint together in almost all cases.
Will I be in pain while I recover?
Most people experience only mild pain after XLIF surgery that continually improves over the following weeks.
What are the possible complications of XLIF?
The primary complication is lumbar plexus injuries and damage to the nerves around the plexus. The occurrence of this complication is highly correlated with surgeon experience, with surgeons who have performed 200-300 procedures generally achieving better outcomes with complication rates below 1%.
Minor damage to the lumbar plexus can heal slowly over the course of six weeks.
How long does XLIF surgery take?
A single-level procedure without screws can be completed in as little as 30 minutes. If screws are required, the procedure can take up to 90 minutes. Multilevel procedures can take 2-3 hours.
Additional Resources
Surgical Videos
Warning: This video contains surgical footage. Viewer discretion is advised.
References
- DenHaese R, Gandhi A, Ferry C, Farmer S, Porter R. An In Vitro Biomechanical Evaluation of a Lateral Lumbar Interbody Fusion Device With Integrated Lateral Modular Plate Fixation. Global Spine J. 2021 Apr;11(3):351-358. doi: 10.1177/2192568220905611. Epub 2020 Feb 20. PMID: 32875868; PMCID: PMC8013934.
- Walker CT, Farber SH, Cole TS, Xu DS, Godzik J, Whiting AC, Hartman C, Porter RW, Turner JD, Uribe J. Complications for minimally invasive lateral interbody arthrodesis: a systematic review and meta-analysis comparing prepsoas and transpsoas approaches. J Neurosurg Spine. 2019 Jan 25:1-15. doi: 10.3171/2018.9.SPINE18800. Epub ahead of print. PMID: 30684932.
- Xu DS, Paluzzi J, Kanter AS, Uribe JS. Anterior Column Release/Realignment. Neurosurg Clin N Am. 2018 Jul;29(3):427-437. doi: 10.1016/j.nec.2018.03.008. PMID: 29933810.